Imaging of the Injured Cervical Spine and Spinal Cord
David W. Cadotte
David Mikulis
Michael G. Fehlings
Imaging of the injured cervical spine can be broken down into imaging of the soft tissues, imaging of the vasculature, imaging of the bones, and imaging of the spinal cord itself. There is an armamentarium of imaging tools that enables evaluation of each of these domains. The main purpose of imaging the injured cervical spine and spinal cord is to establish an accurate diagnosis and guide treatment directed toward maintaining spinal alignment with preservation of neurologic function. In addition, imaging methods may offer prognostic value, as is discussed below.
This chapter is arranged in two parts. Part one provides an overview of the imaging features of cervical spine injury organized from the occiput to T1. Part two discusses the radiographic features of cervical spine trauma in patients with specific conditions that affect the cervical spine such as diffuse idiopathic skeletal hyperostosis (DISH) and ankylosing spondylitis.
PART 1: DETAILED RADIOGRAPHIC ASSESSMENT OF THE CERVICAL SPINE FOLLOWING TRAUMA
INITIAL EVALUATION OF THE CERVICAL SPINE FOLLOWING TRAUMA
In the event of traumatic injury to the cervical spine, the initial means of investigation is usually a plain x-ray or a computed tomography (CT) scan. Much debate has arisen as to what method provides the most reliable and cost-effective means of diagnosing injury and providing optimal care for patients. While this debate is beyond the scope of this text, we provide an overview of the evaluation that should take place regardless of the modality chosen to investigate the cervical spine injury.
Plain Radiography
The use of plain radiographs of the cervical spine occupies an important niche in the evaluation of the trauma patient both in terms of initial evaluation and for follow-up. An upfront note of caution must be conveyed, however, as several authors have demonstrated fractures undetected on plain film later revealed by CT scan (1,2). The standard views are anterior-posterior (AP), lateral, and openmouth odontoid; a lateral swimmer’s view may also be obtained to examine the cervicothoracic junction if C7 and T1 are not adequately assessed on the true lateral projection. Dynamic flexion/extension views have limited role in the acute setting as muscle spasm and other distracting injuries often preclude an adequate examination (3). This dynamic study is of value during the follow-up period to assess potential ligamentous instability during recovery from injury.
The AP radiograph of the normal cervical spine should reveal the midline spinous processes at each level. The uncovertebral joints (C3-C6) should be symmetric and vertically aligned at all levels. The vertebral bodies should be of equal height and have a smooth cortical surface.
In evaluating the lateral radiograph, one should systematically proceed through the following checklist: (a) The radiograph should display the occiput through the level T1, (b) the lines connecting the anterior and posterior margins of the vertebral bodies and the spinolaminar line (the anterior margin of the junction of the spinous process and lamina) should form a gentle convex curve with no steps or discontinuities, (c) the laminar space (the distance from the posterior aspect of the articular pillars to the spinolaminar line) should be uniform throughout the cervical spine, (d) the prevertebral soft tissues should be examined for increased opacity indicating swelling and possible ligamentous injury, (e) the intralaminar spaces (the space between the laminar arches) should not be widened, and (f) the lateral atlantodental interval can be visualized.
The open-mouth odontoid view reveals the atlantoaxial articulation. One must examine for the lateral masses of C1, the dens, and the superior facets of C2. The occipital condyles may also be visualized. There should be no offsets between the occipital condyles, lateral masses of C1, and the lateral masses of C2.
Computed Tomography
While plain radiographs provide a fast means of surveying the regional anatomy in the initial evaluation of cervical spine trauma, especially in low-income countries where other modalities may not be readily accessible, CT scan has become the most common method of evaluation in most institutions and certainly in larger trauma centers. Some advantages of CT over plain x-rays are improved visualization of the craniocervical junction and the cervicothoracic junction, improved rate of fracture detection, and the ability to reformat images for surgical planning in three dimensions. Additionally, reformatted images enable detection of fractures in the plane of section of acquired CT slices.
When considering the cost of CT over plain films, many factors must be considered including the time required to complete the study, the technologist’s time, film viewing stations, and, perhaps most importantly, the accuracy of the diagnosis and its resultant costs both in terms of individual patient care and economic costs of misdiagnosis (4—6). Several studies have attempted to gauge the cost of CT versus plain films, with CT showing greater efficacy (7).
CT protocol should be performed with 1-mm slices enabling reformats. Sagittal and coronal reformats are then reviewed just as the plain radiographs. The axial images are then reviewed individually using both bone and soft tissue settings to assess fractures and soft tissue injury including extradural hematoma and herniated disks.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) should be used to further evaluate patients with either evidence of bony or soft tissue injury (plain films or CT) or with neurologic deficit (myelopathy or radiculopathy). MRI has superior soft tissue screening capability and is the only modality that can accurately assess injury to the spinal cord itself. The addition of pulse sequences such as Short TI Inversion Recovery (STIR) and fat-suppressed images has led to more sensitive evaluation of ligament damage.
EVALUATION OF ATLANTOAXIAL REGION
Atlas Fractures
Fractures of the atlas are by and large not associated with neurologic deficit (8) but are associated with a higher rate of fracture elsewhere in the cervical spine, particularly C2 and C7 (9). This is presumably due to the mechanism of injury that results in atlas fractures, namely axial loadingtype injuries. This results in burst pattern upon the atlas and expansion of the spinal canal. One should therefore screen carefully for additional injuries when a C1 fracture is identified. While plain films may identify atlas fractures, the highest yield is with CT scan. Axial source images should be carefully examined for evidence of fracture lines. C1 fractures have typically been described as Jefferson, lateral mass, or isolated to the anterior or posterior arch. Classical Jefferson (10) fractures are a four-point disruption of C1 at the junction of the anterior and posterior arches with the lateral masses. These represent the weakest structural zones of the atlas. It is now accepted that any fracture pattern that contains a disruption of both the anterior and posterior arches be classified a variation of the Jefferson fracture (11). When disruption of fracture fragments more than 6 to 7 mm is present, one should consider a transverse atlantal ligament disruption, which is potentially unstable. When viewing plain films, it is often difficult to view the fracture itself, but it may be implied from the lateral displacement of the lateral masses of C1 relative to the lateral margins of the superior facet of C2 on the open-mouth odontoid view. In addition, the lateral view may reveal increased atlantoaxial distance (>3 mm should be considered suspicious for fracture) and anterior or posterior displacement of the C1 spinolaminar line. The presence of prevertebral soft tissue swelling may be the only clue to the presence of a fracture on plain x-ray. CT is very effective for revealing the number and position of fracture fragments. Coronal reconstructions will demonstrate the offset of the lateral masses relative to C2. Sagittal reformats will enable assessment of the atlantoaxial distance and the anterior/posterior displacement of the C1 spinolaminar line.
Isolated fractures of one lateral mass may occur as a result of an eccentric axial loading injury. Rarely do these fractures occur in isolation but more commonly in combination with occipital condyle fractures or fracture of the articular process of C2. The open-mouth odontoid view may reveal the fracture. CT scan is usually diagnostic.
Distinct from Jefferson fractures are isolated fractures of the posterior arch of C1. This may occur secondary to a hyperextension injury where the posterior arch is wedged between the occiput and the posterior elements of C2. Rarely, an avulsion injury of the anterior arch of C1 can occur where the tendinous insertion of the longus colli muscle and the anterior longitudinal ligament can result in a horizontal fracture of the anterior arch.
One difficulty associated with the diagnosis of atlas fractures are clefts and aplasias that may occur in the bony ring. One must therefore learn to distinguish from the smooth cortical surface of normal variants with disrupted cortical lines that indicate fracture.
Axis Fractures
Approximately 15% to 20% of cervical spine fractures involve the axis, and about 20% of these are associated with fractures elsewhere in the cervical spine (12,13). To further breakdown the axis fractures, over 50% are odontoid fractures, approximately 25% are hangman’s fractures (fracture of both pars interarticularis of C2), and the remainder are fractures involving the body, lateral mass, or spinous process of C2 (14,15).
Odontoid Fractures
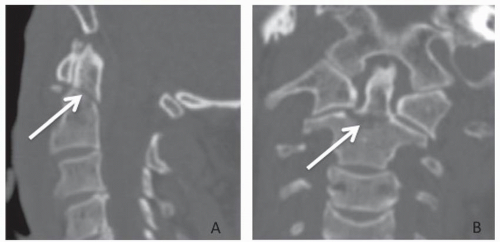
While open-mouth odontoid and lateral plain radiographs are often diagnostic, CT has become the investigation of choice. When describing the bony characteristics of an odontoid fracture, the most used classification is that of Anderson and D’Alonzo (16). This system divides odontoid fractures into three types (I, II, and III) based on the location of the fracture line. Type IIa was introduced somewhat later by Hadley et al. (17) to describe a comminuted and potentially unstable subtype of II. These
fractures and classification systems are described in detail elsewhere in this book and therefore only briefly described here. Type I is an oblique fracture of the superior-lateral aspect of the dens representing an avulsion at the alar ligament attachment. Type II is a fracture through the base of the dens. Type IIa is a comminuted fracture. Type III is an oblique fracture of the superior aspect of the C2 body that extends in an oblique direction to the base of the dens. A case example is presented in Figure 43.1.
fractures and classification systems are described in detail elsewhere in this book and therefore only briefly described here. Type I is an oblique fracture of the superior-lateral aspect of the dens representing an avulsion at the alar ligament attachment. Type II is a fracture through the base of the dens. Type IIa is a comminuted fracture. Type III is an oblique fracture of the superior aspect of the C2 body that extends in an oblique direction to the base of the dens. A case example is presented in Figure 43.1.
Hangman’s Fractures
The forces applied to the cervical spine during judicial hangings produced a specific fracture pattern; this pattern was studied in the mid-1900s, and the name hangman’s fracture was adopted (18). Three patterns can coexist within this description including traumatic spondylolisthesis of the axis, fractures of the neural arch, and fractures of the ring of the axis. The most common cause in our era is that of automobile accidents resulting in a sudden hyperextension of the neck, which occurs during fast deceleration with the head hitting the windshield. The AP plain film is not of much value in identifying this fracture, but the lateral film readily shows the injury. Several aspects of the film must be carefully examined: soft tissue swelling in the prevertebral soft tissue, oblique fractures extending from posterior-superior to anterior-inferior, widening of the body of C2 in comparison to C3 due to a fracture involving the body with posterior displacement, posterior displacement of the C2 spinolaminar line, and finally an avulsion fracture of the anterior-inferior segment of C2 that indicates disruption of the anterior longitudinal ligament. While each of the patterns may be identified on plain radiography, CT is valuable to clarify the full extent of the fracture lines and also to evaluate the remainder of the cervical spine. The classification of axis fractures is discussed in a forthcoming chapter. Neurologic deficit is rare in this type of injury as the fracture pattern usually results in expansion of the spinal canal. MRI is warranted if neurologic deficits are present, enabling visualization of the degree of spinal cord compression (disk rupture or extradural hematoma) as well as the presence of cord contusion (either hemorrhagic or nonhemorrhagic).
Other C2 Fractures
Occasionally, axis fractures occur outside the abovedescribed patterns resulting from a combination of lateral bending with simultaneous axial compression. This results in an isolated C2 lateral body fracture. Rarely does this occur in isolation. Therefore, other fractures must be looked for including ipsilateral occipital condyle, ipsilateral C1 lateral mass, or subaxial pathology. One must be sure to rule out impaction of the C2 component of the atlantoaxial articulation or asymmetry of the C2 lateral body height.
Atlantoaxial dislocation can occur in traumatic events and is more common in individuals predisposed to laxity of the spinal ligaments such as the transverse ligament associated with Down’s syndrome. Subluxation or even complete dislocation of the lateral atlantoaxial articulations can occur. A component or rotation is usually involved. Neurologic symptoms can arise and should be investigated with MRI. Investigation may begin with plain films, but these are often difficult to interpret. We therefore recommend that patients suspected of atlantoaxial dislocation injury be investigated with CT. Axial images demonstrate the rotated position of the atlas on the axis; if pathology is present, this rotation exceeds the normal limit of 45 degrees (19). Displacement of the atlas, either anterior or posterior, may also be seen. Coronal reconstructions may reveal distraction of the lateral masses of
C1 on C2, and when greater than 7 mm, rupture of the transverse ligament is indicated. Similarly, disruption of the transverse ligament may be noted by an anterior atlantodental interval greater than 3 mm.
C1 on C2, and when greater than 7 mm, rupture of the transverse ligament is indicated. Similarly, disruption of the transverse ligament may be noted by an anterior atlantodental interval greater than 3 mm.
EVALUATION OF THE SUBAXIAL (C3-C7) REGION
Bony abnormalities following subaxial injury are best visualized with either plain films or CT. If neurologic deficit is also present or intervention is planned to treat the bony injury, MRI imaging is also warranted to delineate the precise nature of the pathology. Information obtained from MRI may include evidence of disk herniation (which could alter the surgical management of certain fracture types), signal change within the spinal cord (which may yield prognostic information for the patient), or evidence of epidural hematoma. The pulse sequences used to evaluate injuries are discussed later in this chapter, but each of T1-, T2-, and fat-suppressed images are necessary to investigate traumatic injury. When examining the bony images of the subaxial cervical spine, whether it is plain films or CT, it is important to keep in mind the mechanism of injury. This information provides important clues that should draw attention to the presence of associated occult injuries. The following discussion therefore focuses on five force vectors that can result in cervical spine injury: vertical compression injury, flexion injuries, flexion-rotation injuries, extension injuries, and extension-rotation injuries.
Vertical compression injuries (burst fractures) are relatively rare in the subaxial cervical spine in isolation, as the forces have been transmitted through many other structures that have been fractured. In the axial plain, one should closely examine for comminuted fractures of the vertebral body and examine the relationship between retropulsed fragments and the spinal cord. A laminar fracture is almost always present. Additional fractures are also likely. Sagittal images show several hallmark features including biconcave vertebral bodies as a result of end plate fractures and fragments displaced both anteriorly and posteriorly. The prevertebral soft tissues show evidence of swelling. The alignment of the cervical spine is usually maintained. Coronal reconstructions may show a fracture line extending through the midportion of the vertebral body. Aside from the bony abnormalities, an MRI should be obtained as axial compression forces are transmitted to the intervertebral disk resulting in nucleus pulposus herniation through the inferior end plate into the vertebral body below or into the spinal canal if the annulus fibrosis fails to contain the pressurized disk. This pressure on the vertebral body results in exploding fragments that may impinge on the spinal canal.
Flexion Injuries
With a flexion force to the cervical spine, the resultant injuries are compression of the anterior column and distraction of the posterior column. These forces can impact the bones, ligaments, or both and result in numerous injury patterns. Here we describe some of the more common injuries and highlight the radiographic features.
The clay shoveler’s fracture (20) is a term used to describe sudden flexion against tensed ligaments of the posterior cervical spine—this results in an avulsion injury of the spinous process of (usually) C6, C7, or T1. Rarely is this fracture pattern unstable, but one must watch for extension of the fracture line into the lamina.
Anterior subluxation refers to the disruption of the posterior ligamentous complex and often a tear in the posterior annulus fibrosis. The anterior longitudinal ligament remains intact. There is usually no bony injury detected (although anterior corner fracture of the vertebral body can occur), which can make initial evaluation on plain films or CT difficult, but one must be cautious so as not to miss ligamentous damage. This is often subtle on x-ray imaging but may manifest as a kyphotic deformity at the level of ligamentous damage or widening of the interspinous distance at one level. Other radiographic clues are distraction of the facets or prevertebral soft tissue swelling. Delayed morbidity may result should the ligaments fail to heal (21); one must therefore look carefully at initial images given the mechanism and have a low threshold for performing an MRI study if suspecting ligament damage.
Simple wedge compression fractures result from compression on the anterior aspect of the vertebral body. The fracture usually involves the superior end plate of a mid to lower cervical body with less than 25% compression and no disruption to the posterior ligamentous complex. MRI may be helpful to rule out ligamentous injury.
Continuing along the spectrum of increasing force, bilateral facet dislocation represents anterior subluxation at its extreme. In this case, the inferior articular facets from one vertebral body are dislocated anteriorly with respect to the superior facets of the adjacent vertebra. Usually occurring in the lower cervical spine, this injury pattern typically involves disruption of the anterior, middle, and posterior columns along with the ligamentous joint capsules. Bony fractures are usually subtle, if present at all, and can easily be missed if either the plain films or CT are not reviewed carefully. Compromise of the spinal canal and also the spinal cord is common. MRI is essential to investigate the degree of neural element involvement and the degree of ligamentous compromise. Treatment of this injury usually begins with reduction of the facet dislocation; whether or not one investigates the cervical spine with MRI prior to this maneuver is a controversial issue. A recent review has highlighted the evidence for early reduction in the setting of worsening neurologic function (22), and others have pointed out the safety of performing this maneuver without prior MRI (23), provided that the patient is awake and cooperative and that serial physical examinations are carried out. A postreduction MRI should be obtained to rule out disk herniation.
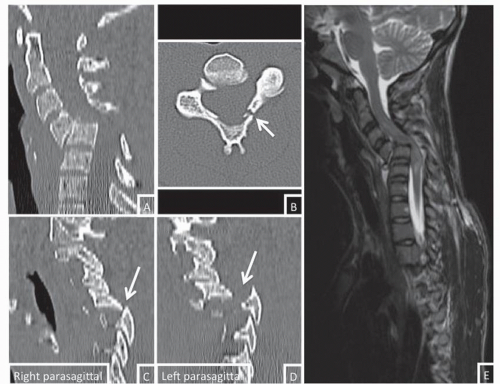
Flexion teardrop fracture describes the most severe flexion injury of the cervical spine and involves disruption of ligaments in each of the anterior, middle, and posterior columns in addition to disk rupture and fracture of the anterior-inferior portion of the vertebral body in a “teardrop” pattern. In some cases, this fracture is accompanied by a sagittal vertebral body fracture and a fracture of the posterior neural arch. This additional fracture pattern gives an indication of the incredible forces that caused the injury and is nearly always associated with severe neurologic compromise. Both CT and MRI are
advised to gain a complete understanding of the injury pattern and plan treatment, as this is a very unstable injury. A case example of a severe flexion injury is illustrated in Figure 43.2.
advised to gain a complete understanding of the injury pattern and plan treatment, as this is a very unstable injury. A case example of a severe flexion injury is illustrated in Figure 43.2.
Flexion-Rotation Injuries
Flexion-rotation injuries occur when a combination of each of these forces is applied to the cervical spine. The resultant injury is usually a unilateral facet dislocation. Briefly, this injury can be described as the inferior articular process of the dislocated facet sitting in front of the superior articular process of the adjacent vertebra. It can be inferred that the posterior ligaments are torn in this region. There is usually a fracture with a vertical orientation through the articular pillar that may extend into the ipsilateral pedicle and/or lamina (24). MRI may be warranted if there are neurologic symptoms to assess for cord injury or epidural compression from hematoma or disk herniation. In addition, CT angiogram or an equivalent may be warranted to investigate the vertebral arteries, which are prone to injury in flexion-rotation injuries (25). However, performing this investigation is controversial as arterial dissections are usually not treated unless symptomatic, making a detailed clinical exam more important.
Extension Injuries
Extension injuries tend to occur in the lower cervical spine and are more common in persons with ankylosing spondylitis (AS) and DISH (26,27). This can be explained by the fact that as multilevel bony fusion occurs, levers are created across the remaining mobile segments. During trauma, forces act on these levers across the mobile segment, resulting in fracture (28). This injury pattern results in distraction of the anterior and middle columns (and
subsequent avulsion injury) and compression of the posterior column (and subsequent impaction injury). One must be cautious when interpreting plain x-rays or CT imaging, as bony abnormalities may be absent. If the injury resulted in a dislocation, spontaneous reduction may have occurred immediately after the injury. Despite absence of bony abnormalities, significant muscle and ligament damage may have occurred and instability may be present. While AP x-rays are of limited value, the lateral view may show evidence of soft tissue injury (29) such as thickness of prevertebral soft tissues or a vacuum defect in the intervertebral disk. The lateral view is also useful in showing anterior vertebral body avulsion fractures. CT is necessary to properly investigate extension injuries, especially those with underlying disease as described above. Axial images will reveal subtle fractures, especially of the posterior bony elements, that may not be detected on plain films. Sagittal reformats usually reveal normal vertebral body alignment with evidence of soft tissue. If fracture dislocation has occurred, one will see evidence of loading fractures on the posterior elements: spinous process, lamina, articular pillars, pedicles, or posterior vertebral body. The intervertebral disk space may be widened anteriorly and compressed posteriorly. The facet joints may be disrupted. Neurologic deficit is common in this type of injury, especially those with an underlying disease. MRI is essential to investigate the precise pathology affecting the neural elements and aiding in surgical planning. MRI enables assessment of the longus colli and longus capitis muscles, the anterior longitudinal ligament, the annulus fibrosis, potential avulsion of the intervertebral disk from the superior vertebral body, and the posterior ligamentous complex.
subsequent avulsion injury) and compression of the posterior column (and subsequent impaction injury). One must be cautious when interpreting plain x-rays or CT imaging, as bony abnormalities may be absent. If the injury resulted in a dislocation, spontaneous reduction may have occurred immediately after the injury. Despite absence of bony abnormalities, significant muscle and ligament damage may have occurred and instability may be present. While AP x-rays are of limited value, the lateral view may show evidence of soft tissue injury (29) such as thickness of prevertebral soft tissues or a vacuum defect in the intervertebral disk. The lateral view is also useful in showing anterior vertebral body avulsion fractures. CT is necessary to properly investigate extension injuries, especially those with underlying disease as described above. Axial images will reveal subtle fractures, especially of the posterior bony elements, that may not be detected on plain films. Sagittal reformats usually reveal normal vertebral body alignment with evidence of soft tissue. If fracture dislocation has occurred, one will see evidence of loading fractures on the posterior elements: spinous process, lamina, articular pillars, pedicles, or posterior vertebral body. The intervertebral disk space may be widened anteriorly and compressed posteriorly. The facet joints may be disrupted. Neurologic deficit is common in this type of injury, especially those with an underlying disease. MRI is essential to investigate the precise pathology affecting the neural elements and aiding in surgical planning. MRI enables assessment of the longus colli and longus capitis muscles, the anterior longitudinal ligament, the annulus fibrosis, potential avulsion of the intervertebral disk from the superior vertebral body, and the posterior ligamentous complex.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree