Building on Goffman’s initial conceptualization, Jones et al. (1984) have identified six dimensions of stigma namely concealability, course, disruptiveness, peril, origin, and aesthetics. Concealability is the extent to which the condition can be seen by others or can be hidden; course is the severity and pattern of the condition over time, and disruptiveness is the degree of interference with the usual patterns of social interaction. The term ‘aesthetic qualities’ is how much the condition upsets others by way of the five senses; origin is the perceived cause and degree of responsibility of a person in contracting the illness (or condition). Finally, peril is the amount of fear and danger associated with a person’s illness (Feldman and Crandall 2007; Jones et al. 1984; Quinn and Chaudoir 2009).
Goffman (1964) and Scambler and Hopkins (1990) have developed two key concepts to distinguish between “enacted” and “felt” stigma. Enacted stigma refers to acts or instances of discrimination against people with a stigmatizing condition on grounds of their perceived unacceptability or inferiority by members of the society. This could include overt discrimination in the workplace or educational institution, neglect, hostility, abuse or what is termed “fair and legitimate” discrimination, such as banning, driving or operating heavy machinery for epilepsy. Felt stigma is the anticipation or fear (on the part of persons with a stigmatizing trait) of enacted stigma, or negative reactions to the disclosure of the stigmatizing condition, and this also encompasses feelings of “difference” and shame. Felt stigma does not need to be based on personal experiences of enacted stigma, but is often built upon perceived social responses to the given stigmatizing condition, and is as debilitating as enacted stigma itself. These concepts are known as “Scambler’s hidden distress model of stigma”, extended by Weiss (2008) to include the concepts of “internalized, endorsed, anticipated and accepted stigma” (Fig. 2). In particular:
Internalized stigma is a process through which a person with a stigmatized condition accepts perceived exclusionary views of the society and self-stigmatizes himself or herself.
Anticipated stigma is fear of enacted stigma on behalf of a person with a stigmatizing condition.
Endorsed stigma is a situation whereby some members of the society support and encourage acts of discrimination or exclusion against persons with a stigmatized condition although they do not actively engage in those acts themselves.
Accepted stigma is the attitude of some members of the society who completely disagree with acts of discrimination or exclusion of persons with a stigmatized condition, but do nothing to stop it.
Since Goffman’s seminal treatise on stigma in 1964, the number of publications on social stigma has increased sharply in recent years (from 458 articles in 2006 to 1,109 in 2011).
In 2006, Weiss and collaborators proposed a new formulation to facilitate action-oriented research on health-related stigma:
Stigma is typically a social process, experienced or anticipated, characterized by exclusion, rejection, blame, or devaluation that results from experience or reasonable anticipation of an adverse social judgment about a person or group. This judgment is based on an enduring feature of identity conferred by a health problem or health-related condition, and the judgment is in some essential way medically unwarranted. In addition to its application to persons or a group, the discriminatory social judgment may also be applied to the disease or designated health problem itself with repercussions in social and health policy. Other forms of stigma, which result from adverse social judgments about enduring features of identity apart from health-related conditions (e.g., race, ethnicity, sexual preferences), may also affect health; these are also matters of interest that concern questions of health-related stigma.
1.2 Stigma and Neglected Tropical Diseases
The concept of neglected tropical diseases (NTDs) emanated from the meetings convened in Berlin by the World Health Organization (WHO) and Deutsche Gesellschaft für Technische, now Internationale Zusammenarbeit in 2003 and 2004 (WHO 2004). Following these developments, Weiss (2008) and Hotez (2008) recently reviewed the issues of stigma in NTDs. Historically leprosy has been a major focus of stigma studies and literature. Other NTDs that generate stigma overtones include onchocerciasis, lymphatic filariasis, plague, Buruli ulcer, leishmaniasis, African trypanosomiasis and Chagas’ disease. The numbers of existing cases of selected NTDs estimated by WHO (2010) and which cause stigma and disablement have increased sharply (Table 1).
Table 1
Estimated numbers of existing cases of selected NTDs which cause stigma and disablement globally (reproduced from WHO 2010)
Specific NTD | Disabilities resulting from disease | Numbers of cases/year or with permanent chronic symptoms |
|---|---|---|
Buruli ulcer | Disfigurement | 5,000/year |
Onchocercosis/mucocutaneous leishmaniasis | Disfigurement | 1.5 million/year |
Onchocerciasis | Blindness; severe itching | 265,000 existing cases |
746,000 existing cases | ||
Lymphatic filariasis | Lymphoedema | 15 million existing cases |
Hydrocele | 25 million existing cases | |
Trachoma | Trichiasis | 8.2 million existing cases |
Yaws | Disfigurement | 2.5 million (global prevalence estimate 1995) |
Leprosy | Disfigurement | 213,000/year |
Human African trypanosomiasis | Neuropsychiatric disorders | Circa 10,000 new cases/year |
In many NTDs stigma results from external deformations such as scars, physical manifestations of leprosy, or physical disabilities (Table 1). Furthermore, the impact of the meaning of the name of the disease may be as great, or even greater, source of suffering as symptoms of the disease. For example, paucibacillary leprosy may present at an early stage as a painless depigmented or anaesthetic patch. Receiving the announcement of the diagnosis is likely to be far more troubling than these symptoms per se (Weiss et al. 2006; Corrigan 2007). The emotional impact of the social and cultural meanings of illness indicates another way by which stigma operates. For example, in settings where arranged marriages are a major concern of families for their children, the impact of a health problem on the ability to marry is troubling. For example, men with hydrocele suffer from embarrassment, ridicule and frustration due to their inability to perform sexual intercourse (Ahorlu et al. 2001).
1.3 Neuroscience of Stigma Behaviour
We are, by nature, a highly affiliative species craving social contact. When social experience becomes a source of anxiety rather than a source of comfort, we have lost something fundamental – whatever we call it. (Insel 2002).
Thomas R. Insel, Editor of Biological Psychiatry, concluded that findings from various neuroscience disciplines appear to suggest that the brain has a special way of processing social behavioral information (Yizhar et al. 2011; Greimel et al. 2012; Tate et al. 2006). It would even appear that special genes determine whether some animals that do not have brains exhibit solitary or social behavior (Dreller and Page 1999). We have attempted to summarize the current data in trying to answer the following questions:
1.
What happens in the brain of a person who stigmatizes another individual or a group of persons?
2.
What happens in the brain of an individual who feels stigmatised or who is simply afraid of being stigmatised?
Is there any such neural network as a stigma centre in the brain? How does the brain develop social norms and are these ‘programmes’ fixed in time and space and if not, what modulates them? These questions are clearly very difficult to answer. The young growing discipline of behavioural or social neuroscience is going to hopefully enable us to gain a better understanding of these issues. Derks et al. (2008) have reviewed data obtained with electroencephalography, event-related potentials, or functional magnetic resonance imaging (fMRI) methods to examine neural correlates of stereotype and social identity threat. The findings that brain activation is related to the experience of being stereotyped have shed light on the cognitive processes underlying the social identity processes (Derks et al. 2008). Stereotype threat is a situational predicament in which individuals are at risk, by dint of their actions or behaviours, of confirming negative stereotypes about their group (Steele and Aronson 1995). For example, data obtained using fMRI suggest that stereotype threat affects women’s mathematics performance in two ways: first, it disrupts normal recruitment of cognitive areas required for high math performance (the inferior prefrontal cortex, left inferior parietal cortex, and bilateral angular gyrus) and, second, it increases the recruitment of areas which allow for the processing and regulation of emotions (ventral anterior cingulate cortex). This implicates that women perform more poorly under stereotype threat because valuable cognitive resources are spent on emotional regulation instead of on the task at hand (Derks et al. 2008). Although this approach has limitations, it has the merit of providing some leads to the understanding of the complex phenomenon of stigma, which may in future contribute to its reduction in the targeted populations.
With regards to the second question, social neuroscience research has focused more on people who stereotype others rather than on the stigmatized individuals (see Dickter and Bartholow 2007; Ito et al. 2006). Brain imaging and electrophysiology have been applied to research on stereotyping from the perpetrator’s perspective and this approach has yielded some insights into the processes that underlie prejudice and racial bias. For example, race effects have been observed in two brain areas traditionally associated with face perception, the fusiform gyrus and the posterior cingulate cortex. While these brain areas are considered to be responsible for face encoding and person knowledge respectively, evaluation and behaviour regulation appears to occur in the amygdala and anterior cingulate cortex, respectively (Ito and Bartholow 2009). This model, however, still has many unanswered questions such as the brain mechanisms of stereotype activation and regulation of stereotypic responses, and the psychological mechanisms involved.
2 Neurological Diseases Associated with Stigma and Its Determinants in the Tropics
2.1 Neurological Diseases Associated with Stigma in the Tropics
Stigma is more likely to be associated with chronic, rather than acute neurological conditions and is one of the major limitations of care provision and control of these diseases. Among chronic neurological diseases we shall discuss leprosy, epilepsy, onchocerciasis, human African trypanosomiasis (HAT) and schistosomiasis.
In the available published literature, amoebiasis, rabies, neurocysticercosis are only vaguely associated with stigma.
2.1.1 Leprosy (Hansen’s Disease)
Leprosy, also known as Hansen’s disease or neurodermatitis, is arguably the most extraordinary and misunderstood of diseases. Leprosy is a dreaded disease caused by Mycobacterium leprae akin to causative agent of tuberculosis, affecting the skin, the nerves in and close to the skin, the anterior third of the eyes, the upper respiratory tract, and the testicles (Sabin and Swift 1996). Although there is only one kind of leprosy bacillus, there are several varieties of leprosy because of the patient’s immunological reaction to the infection. Three major forms have been described: tuberculoid or paucibacillary form in patients with high immune resistance, borderline form, and lepromatous form in patients with little or no immune resistance leading to progressive debilitation and gross mutilation. Patients with borderline leprosy have less skin involvement than those with lepromatous disease and may have more circumscribed skin lesions. In these patients, skin lesions are more severe than in patients with tuberculoid disease. In the spectrum of borderline leprosy, immunity may change, with patients worsening and their disease resembling lepromatous disease (downgrading reaction), or evolving toward the tuberculoid form (reversal reaction). Such shifts in the spectrum of disease may occur spontaneously or in response to drug treatment or inter-current medical conditions, such as underlying neoplasms or secondary infections (Sabin and Swift 2008).
Leprosy has been a major interest of health-related stigma studies from the outset. As cited by Hotez (2008), Berton Roueche observed that an ancient Egyptian pharaoh was known to banish people with leprosy to the edges of the Sahara desert. He coined the term lepraphobia to describe how, at the peak of the leprosy epidemic in Europe in the twelfth to fourteenth century, affected individuals were often subjected to their own mock funeral prior to banishment from their families and communities. In some cases, they endured torture and execution. Social constructions of leprosy are commonly guided by cultural, traditional and religious beliefs or myths about disease and illness (Wong 2004; Waxler 1981; Van den Broek et al. 1998; Nsagha et al. 2011; Opala and Boillot 1996). Biblical teachings perpetuated by missionaries associated leprosy with sin and uncleanliness, and leprosy patients came to be considered outcasts as a consequence (Edmond 2006). Leprosy-infected people are frequently considered cursed or victims of witchcraft, or blameworthy or immoral, and their disease well deserved (Nsagha et al. 2011). In many countries, treatment policies require incarceration of people affected by leprosy at various leprosaria, sometimes due to the high rates of illiteracy and misinformation about the disease (Kazeem and Adegun 2011). While people with enigmatic physical disfigurement (lepromatous form), and the distinctive ulcers consequent to untreated leprosy will face ridicule and rejection from society (Fig. 3), the diagnosis of the tuberculoid or paucibacillary form will induce fear and ultimately anticipated stigma.
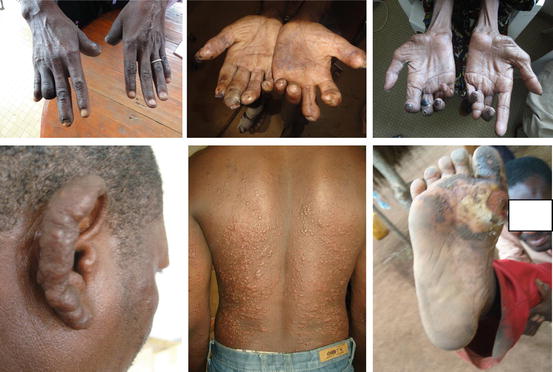
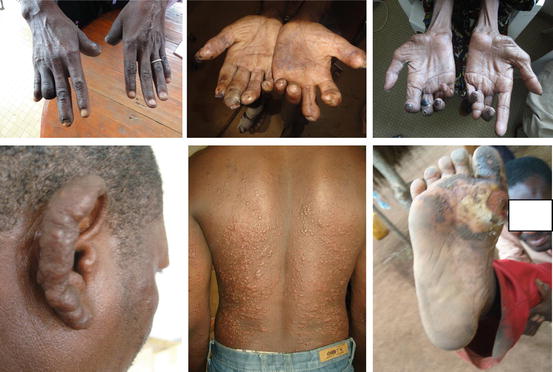
Fig. 3
Clawed and amputated fingers; muscle atrophy of the thenar and hypothenar hand regions in leprosy. Lepromatous lesions on earlobe and back in same patient, foot ulceration (Courtesy: EN Tabah). These severe disfigurements cause fear of contagion and lead to rejection of people with leprosy
2.1.2 Epilepsy
Although epilepsy is not a neglected disease, a chapter on stigma has to discuss the issue. According to the definition of the International League against Epilepsy (ILAE), epilepsy is a transient occurrence of signs and/or symptoms due to abnormal, excessive, or synchronous neuronal activity in the brain (Engel and Pedley 2008). More than 60 million people worldwide suffer from epilepsy (Ngugi et al. 2010) and it is estimated that 80 % of the burden of epilepsy worldwide is borne by resource poor countries (WHO 2004; Birbeck and Kalichi 2004; Kaiser et al. 1998; Longe and Osuntokun 1989; Osuntokun et al. 1987; Jilek-Aall and Rwiza 1992). Due to the treatment gap, the number of people with active epilepsy who have not accessed biomedical services or who are not on treatment or are on inadequate treatment is between 62 and 75 % in sub-Saharan Africa (Mbuba et al. 2012a; Meyer et al. 2010). Traditional belief systems attribute epilepsy to demon possession, witchcraft, and/or seek to blame the victim (Baskind and Birbeck 2005; Njamnshi et al. 2010). All these provide the ideal environment for stigma to flourish. Besides these beliefs, body disfigurement resulting from falls, burns or drug adverse effects also contribute to stigma development in epilepsy. For example, a Cameroonian suffering from sustained severe burns on the face and upper limbs, leading to the loss of her left hand. As a result of the discrimination associated with epilepsy in this part of Cameroon, she was sent on exile from the city to live far away in a farmhouse, to avoid her associating with other people (Fig. 4).


Fig. 4
Stigmatizing burn deformities in a Cameroonian epilepsy patient (courtesy: Pastor JTN Njamnshi, Cameroon Baptist Seminary, Kumba)
2.1.3 Onchocerciasis (River Blindness)
Onchocerciasis results from infection with the nematode Onchocerca volvulus, for which man is the only reservoir. Adult worms live in sub-cutaneous nodules and have a reproductive life-span of 9–11 years (Plaisier et al. 1991). The adult female worm produces microfilaria in millions, which migrate to the skin of the human host.
The microfilaria are responsible for the clinical manifestations of the disease which include dermatitis, with concurrent pruritus; lychenified skin lesions; skin depigmentation and atrophy; and lymphadenitis, which results in the hanging groin and elephantiasis (Murdoch et al. 1993, cited in: Okoye and Onwuliri 2007). The most severe complication of onchocerciasis infection is irreversible and often stigmatizing blindness due to ocular lesions of both the anterior and the posterior chambers of the eye.
The severe itching, depigmentations as well as lichenification of the skin as a result of onchocercal infection have been a source of discrimination and stigma (Awedoba 2001). Skin nodules could also be a source of stigma depending on location (Fig. 5). Okoye and Onwuliri (2007) have found that the most worrisome consequence of onchocercal skin disease in Northeastern Nigeria included social isolation, feeling of shame and low esteem, skin blemish and marital problems. They recount the story of a 48 year-old female victim of onchocercal skin disease as follows: “I am always afraid (anxious) that an attack of itching in a private part (buttock and groin) could occur at a public gathering; I therefore kept off; in fact, I hated myself”. In the same community, relating to stereotypes held with respect to marriage, a 26 year-old man said, “When a lady’s body has been spoilt by mbiba (popular rashes), only elderly widowers and already married men would seek her hand in marriage”. These pejorative attitudes are held across most onchocerciasis afflicted areas in sub-Saharan Africa (Awedoba 2001; Tchounkeu et al. 2012).


Fig. 5
Stigmatising onchocerciasis lesions: skin nodule, chronic onchodermatitis, skin atrophy and skin depigmentation in onchocerciasis (courtesy: AC Zoung-Kanyi Bissek)
2.1.4 Human African Trypanosomiasis (Sleeping Sickness)
Stigma related to HAT is not clearly defined since the presenting symptoms resemble those of common conditions such as malaria in the early phase of the disease. However, in Malawi where transmission occurs around game reserves protected from human activity, individuals affected by HAT are stigmatized as deserving the condition, for having violated the band on infringing the game reserves (Chisi et al. 2011).
2.1.5 Schistosomiasis
Stigma in schistosomiasis is related to the post-micturation trickling of blood (Takoungang et al. 2004). The female genital schistosomiasis, which is an advanced form in women, is usually more stigmatizing due to symptom similarity (lower abdominal pain, bleeding after sexual intercourse) to sexually transmissible infections (Ahlberg et al. 2003). These symptoms bring about shame and guilt, resulting in concealment and delay in seeking help among young girls and women.
2.2 Measurement of Stigma
The full assessment of health-related stigma requires at least two levels of consideration that include: assessment in the community (general population as well as specific target groups void of the stigmatized condition in question) to determine enacted and felt stigma and assessment among the affected persons, to determine anticipated, internalized and experienced stigma. The impact of stigma assessment would also target the affected persons, and will seek to measure the level of participation, quality of life, self-esteem and self-efficacy (Van Brakel 2006; Rensen et al. 2010). These approaches are very important as the study of people with a stigmatized health problem provides an account of self-perceived, experienced stigma as well as their consequences. Meanwhile the study of people without the stigmatized health problem in the community clarifies the social context of stigma targeting that condition (Weiss and Ramakrishna 2006).
Different methods could be employed within each approach. The most commonly used methods include:
Questionnaires: These are usually closed or open or interview guides, containing items that allow the collection of data on knowledge, attitudes and reported practices (KAP). This method has been widely used in the assessment of epilepsy and leprosy related stigma (Njamnshi et al. 2009a–e, 2010; Atadzhanov et al. 2010; Babikar and Abbas 2011; Van Brakel 2003).
Qualitative methods: These are assessments based on such methods as key informant interviews, focus group discussions and observation by participants.
Indicators: These are often used in sets. They provide separate information for each indicator, and when pooled together, they may give a profile of stigma and discrimination. They cannot however be summarised in one measure, unless they have been developed as a scale.
Scales: These are quantitative instruments intended to give a numerical result that indicates the severity or extent of the phenomenon measured. Examples of such stigma scales have been developed and validated recently for epilepsy in Kenya (Mbuba et al. 2012a, b) and for use across various neurological conditions in the USA (Molina et al. 2013).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








