Injuries to C1 and C2 (Excluding Odontoid Fractures)
Marcel F. Dvorak
John T. Street
Brian J. Lenehan
FRACTURES OF THE ATLAS
INTRODUCTION
Fractures of the atlas account for approximately 25% of all injuries to the atlantoaxial complex, 10% to13% of all injuries of the cervical spine, and 1% to 2% of all spinal injuries. First described by Cooper in 1822 (1), atlas fractures have been the subject of numerous historical reports. Jefferson in 1920 characterized a burst fracture of the atlas ring—the “Jefferson fracture” (2).
Multiple contiguous fractures involving both the atlas and axis occur relatively frequently. A higher incidence of neurologic deficit is associated with multiple fractures of the C1-C2 complex than occurs with either C1 or C2 fractures in isolation (3). Greene, in a report of 340 C1 fractures, found that there were multiple fractures in 14% of cases. The most commonly reported combination of fractures includes fractures of the atlas in association with type II odontoid fractures, which are found in 24% to 50% of C1-C2 fractures (Fig. 46.1). Likely, the mechanism of forceful hyperextension, which is common to many of these atlas-axis combined injuries, is responsible for the frequency and pattern of combined injuries. The next most common combination is an atlas fracture in association with hangman’s fracture of the axis found in 6% to 26%.
CLASSIFICATION
Levine and Edwards in 1991 classified fractures of the atlas into three types (6). Fractures of the dorsal arch, unilateral or bilateral, occurring at the junction of the dorsal arch and the lateral masses, where the vertebral artery passes over the arch of the first cervical vertebra (Fig. 46.2).
Lateral mass fractures that involved the lateral mass on only one side, with the fractures passing just ventral and just dorsal to the articular surface. The fracture around the lateral mass on one side may be accompanied by a fracture through the dorsal arch on the other side (Fig. 46.3).
Jefferson fracture or burst, fracture characterized by either three or four fractures involving both the ventral and dorsal portions of the ring (Fig. 46.4).
This anatomical classification system does not, however, correlate with injury severity, nor does it offer a treatment rationale/algorithm. It does not allow for prognostication with regard to outcome.
“STABLE” JEFFERSON FRACTURES
Almost all isolated fractures of the atlas are amenable to nonoperative treatment.
Most authors agree with conservative treatment of stable atlas burst fractures with only minor displacement of the lateral masses and an intact transverse ligament. Historically, immobilization options for stable Jefferson fractures have varied from a simple external cervical orthosis to a halo thoracic vest (3,6, 7, 8, 9, 10 and 11). Given the additional morbidity of the more invasive halo thoracic vest, and the lack of reported improved outcomes with its use, we cannot recommended the use of the halo over a Minerva brace or other similar orthosis for the majority of these injuries. A number of authors have reported satisfactory long-term results with nonsurgical treatment of these injuries (3,6, 7 and 8,10). Others have suggested substantial long-term pain and stiffness (5,9,11,12). There are no comparative reports that provide evidence to recommend one form of treatment over another for these fractures.
“UNSTABLE” JEFFERSON FRACTURES
The identification of outcomes and treatment of unstable atlas burst fractures is still controversial. Unstable atlas burst fractures have historically been distinguished from stable fractures by an identifying injury to the transverse ligament, which has been inferred indirectly from measurements of wide displacement of the lateral masses of C1 on the open-mouth odontoid view. Cadaveric, clinical, and biomechanical studies found that combined lateral mass displacement of 6.9 mm implies a rupture of the transverse
ligament (13,14). Allowing for x-ray magnification on open-mouth odontoid radiographs, rupture of the transverse ligament can be assumed at a radiographic measured displacement of 8.1 mm (15).
ligament (13,14). Allowing for x-ray magnification on open-mouth odontoid radiographs, rupture of the transverse ligament can be assumed at a radiographic measured displacement of 8.1 mm (15).
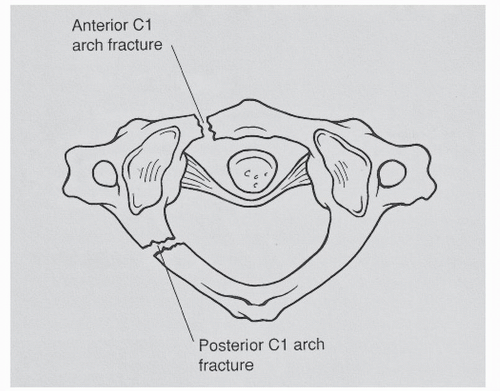 Figure 46.2. Axial view of the C1 ring with typical lateral mass fractures on one side only. Lateral displacement of the C1 lateral mass occurs only on the fractures side. |
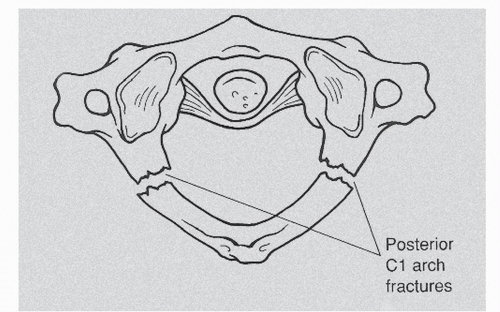 Figure 46.3. Axial view of the C1 ring with two dorsal arch fractures. The TAL remains intact, and the lateral masses of C1 do not spread. |
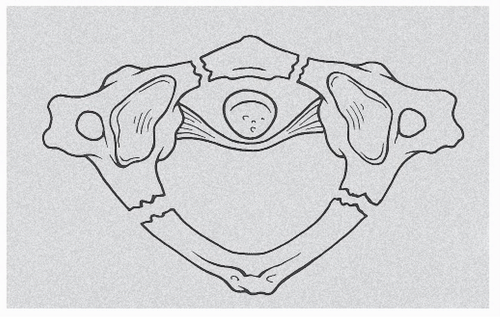 Figure 46.4. Axial view of the C1 ring with a burst fracture. Both lateral masses of C1 will spread and displace laterally. |
Cadaveric experiments by Oda et al. found that the burst-type fractures were associated with postinjury hypermobility at C1-C2 (16). They described a 42% increase in flexion-extension motion, a 24% increase in lateral bending, and a 5% increase in axial rotation. They found that in all instances of transverse atlantal ligament (TAL) disruption, the atlantodental interval was greater than 3 mm. They concluded that the atlantodental interval was the most reliable predictor of transverse ligament disruption in adults following acute C1 fracture.
The concept of instability in relation to Jefferson fractures is based on cadaveric and biomechanical evidence but is lacking clinical validation. There are surprisingly few reports of documented horizontal atlantoaxial instability (increase in the atlantodental interval on flexion) following nonsurgical treatment of Jefferson fractures (17,18). In our experience, the more common outcome
of nonsurgical treatment of widely displaced fractures is painful stiffness, not instability (5,7,9,11,12). Dvorak has shown that patients with “unstable” Jefferson fractures have poor long-term outcomes in terms of health-related quality of life, pain, and stiffness. In the young patient with widely displaced Jefferson fracture, this may be a rationale for early surgical fixation; however, currently, there is no evidence that surgery will lead to improved outcomes over nonsurgical treatment even in these widely displaced injuries. Several authors have recommended halo traction for up to 6 weeks followed by halo thoracic vest immobilization for radiographically “unstable” fractures (5, 6 and 7). There is no evidence that even prolonged traction will maintain the reduced position of the lateral masses of the atlas. Others have recommended surgical stabilization of “unstable” atlas burst fractures (19, 20 and 21).
of nonsurgical treatment of widely displaced fractures is painful stiffness, not instability (5,7,9,11,12). Dvorak has shown that patients with “unstable” Jefferson fractures have poor long-term outcomes in terms of health-related quality of life, pain, and stiffness. In the young patient with widely displaced Jefferson fracture, this may be a rationale for early surgical fixation; however, currently, there is no evidence that surgery will lead to improved outcomes over nonsurgical treatment even in these widely displaced injuries. Several authors have recommended halo traction for up to 6 weeks followed by halo thoracic vest immobilization for radiographically “unstable” fractures (5, 6 and 7). There is no evidence that even prolonged traction will maintain the reduced position of the lateral masses of the atlas. Others have recommended surgical stabilization of “unstable” atlas burst fractures (19, 20 and 21).
SURGICAL OPTIONS INCLUDE
1. Dorsal fusion C1-C2.
The difficulty of performing a fusion of C1-C2 relates to the fact that the lateral displacement of the lateral masses of the atlas affects the congruence of not only the C1-C2 articulation but also the articulation between the occipital condyles and the superior articular processes of the atlas. Tessitore has described a technique to achieve an atlantoaxial arthrodesis while reducing the lateral displacement of the atlas lateral masses. In the absence of comparative outcome data, or even a substantial case series, it is difficult to recommend this or other dorsal fixation techniques for Jefferson fractures.
2. Occiput to C2 fusion.
OSTEOSYNTHESIS OF C1 IN ISOLATED UNSTABLE JEFFERSON FRACTURES
Osteosynthesis of the atlas by a transoral approach is an innovative option in the treatment of unstable Jefferson fractures, especially in young patients with widely displaced fractures that are likely to develop late pain and stiffness. Described by Harms in 2004, it allows anatomic reconstruction of the atlas and provides reliable bony fusion of the fragments (22). The congruence of the atlantooccipital and atlantoaxial joints is restored, and the important rotation of the C1-C2 joint is theoretically preserved, although objective evidence of preserved motion following this procedure is lacking.
The transoral approach is performed by the technique described by Schmelzle and Harms (23). The ventral arch of C1 and the ventral aspect of the lateral masses are exposed. The entry point for the screws, the lower margin, and the medial edge of the lateral mass of C1 are palpated either through the C1-C2 joint or, depending on the type of fracture of the ventral arch, through the fracture line. The entry point should be in the center of the lateral mass. Reduction is performed by traction at the head via a Crutchfield clamp and by direct manipulation at the lateral masses. Osteosynthesis of C1 can be achieved with compression plates or using a screw-rod instrumentation. Screw-rod instrumentation facilitates the reduction, which is achieved by applying compression forces at the screws before fixing the nut. We are concerned about the bulkiness of the instrumentation in the retropharyngeal space, and we believe that the same goals of reduction and direct stabilization can be achieved through a dorsal approach with lateral mass screws. Patients are mobilized within the first postoperative week. A collar is recommended for 6 to 10 weeks after surgery. In Harms series, there was a case of partial redislocation of the lateral masses occurring because of loosening of the screw-rod connection of the implant, resulting in incongruence of the atlantooccipital and atlantoaxial joints.
In summary, the majority of Jefferson fractures can be treated in an external orthosis such as the Minerva brace, without use of the more invasive halo thoracic vest and without long periods of bed rest and traction. In the young patient with a widely displaced fracture, newer techniques of lateral mass screw fixation and reduction through traction and compression makes the possibility of safe dorsal fixation with or without atlantoaxial arthrodesis an option. There is no evidence at present that this form of surgical treatment will lead to improved results over nonsurgical treatment. Although patients with more displaced fractures are more prone to late pain and stiffness, there is little evidence that instability is a frequent complication of the treatment of these injuries.
ATLANTOAXIAL ROTATORY INSTABILITY
Rotatory deformities of the atlantoaxial joint are usually short-lived and easily correctable. Rarely they persist, resulting in torticollis, which is resistant to treatment. Such persistent rotation was termed rotatory fixation of the atlantoaxial joint by Wortzman and Dewar in 1968 (24).
A variety of ethologic factors have been implicated in the development of atlantoaxial rotatory fixation:
Flexion-extension type injury with associated rotational force
C1-C2 ligamentous laxity secondary to effusion within C1-C2 joint
Rupture of one or both alar ligaments and the transverse ligament
C1-C2 lateral mass articular fractures
Patients present with signs and symptoms ranging from neck pain to torticollis typically adopting a “cock robin” head position with the head tilted to the opposite side to which it is rotated. Atlantoaxial rotatory fixation may be associated with suboccipital or upper cervical pain in a proportion of patients.
Determination of the flexible or fixed nature of the deformity is paramount in the management of atlantoaxial rotatory fixation as is the duration from the onset of deformity or injury to the moment of initial treatment. Dynamic computer tomography (CT) with the head in a neutrally rotated position and rotated 15 degrees in both right and left directions allows for both characterization of the abnormality and anatomical classification.
Although rotator atlantoaxial injury is much more common in children, it has been reported to occur in young adults. It is rare in older adults. Once a rotator fixation
has been present for greater than 4 weeks, it becomes very difficult to achieve a closed or even an open reduction. Early treatment, initially with skeletal traction, sedation, and even rotator manipulation under general anesthesia is the first stage of treatment. If successful in reducing the deformity, immobilization in a halo or orthosis may allow the ligamentous anatomy to heal. In the presence of a long-standing or irreducible deformity or one that cannot be maintained in a reduced position, dorsal atlantoaxial arthrodesis is appropriate treatment.
has been present for greater than 4 weeks, it becomes very difficult to achieve a closed or even an open reduction. Early treatment, initially with skeletal traction, sedation, and even rotator manipulation under general anesthesia is the first stage of treatment. If successful in reducing the deformity, immobilization in a halo or orthosis may allow the ligamentous anatomy to heal. In the presence of a long-standing or irreducible deformity or one that cannot be maintained in a reduced position, dorsal atlantoaxial arthrodesis is appropriate treatment.
TABLE 46.1 Summary of the Fielding and Hawkins Classification of atlanto-axial Rotatory Fixation | ||||
|---|---|---|---|---|
|
CLASSIFICATION
Fielding and Hawkins in 1977 classified atlantoaxial rotatory fixation based on a series of 17 patients (25). They classified rotatory fixation into four types (Table 46.1). This anatomical classification system does correlate with injury severity. It does not however offer a treatment rationale/algorithm, nor does it allow for prognostication with regard to outcome. Type I injury is the most benign as the transverse ligament remains intact. These patients usually respond to conservative measures. Type II, with a deficient transverse ligament, is unstable. Types III and IV are rare but are associated with adverse outcomes. In Fielding and Hawkins series, the latter two types had catastrophic results. A type III fixation caused the only fatality in the reported series, where as a type IV lesion accounted for pyramidal tract abnormalities.
INDICATIONS AND CONTRAINDICATIONS TO SURGICAL TREATMENT
Initial treatment of a patient presenting with fixed atlantoaxial rotatory fixation includes halter traction, muscle relaxants, and adequate analgesia. If the deformity fails to resolve, skeletal traction through Gardner Wells Tongs is recommended. Fielding and Hawkins recommended up to 6.8 to 9.1 kg in the adult patient (14). If this resulted in reduction of the deformity, they recommended maintenance of traction for a further 2 weeks followed by halo application.
Patients with type III and IV injury patterns should be considered for early operative intervention. Surgical treatment is indicated where a fixed atlantoaxial rotatory deformity fails to correct following skeletal traction, patients with symptomatic instability, chronic deformity (fixed rotatory fixation for >3 months) by means of a dorsal C1-C2 arthrodesis (Fig. 46.5).
TRAUMATIC SPONDYLOLISTHESIS OF THE AXIS
INTRODUCTION, INCIDENCE AND ASSOCIATED INJURIES
Fractures of the dorsal elements of the C2 vertebra, or axis, are typically due to hyperextension with concomitant compression, a result of high-energy injury, such as motor vehicle accidents, diving, and falls from height. Thus, the incidence of associated injury, in particular head injury, is high with traumatic spondylolisthesis of the axis (TSA). These injuries were initially thought to be reminiscent of that caused by judicial hanging, though this mechanism is one primarily of distraction and subsequent hyperextension, and so were termed (1) “hangman’s fracture.” Much has been written on differences in the mechanism of injury and on the wide range of neurologic deficits that accompany them. Consequently, classification systems unique to TSA have been diverse and have been based on the usual categorizations of anatomic/radiologic, mechanistic, and residual instability.
TSA is the second most common fracture of the second cervical vertebra (C2) accounting for 20% to 23% of fractures and accounting for 4% to 20% of all cervical spine injuries. In a series of 1,820 cervical fractures (2), 19% were fractures of the axis and 4% were TSA type. TSA has been reported as associated with other fractures of the cervical vertebra in 8% to 26% of cases, with about half of the associated fractures involving the atlas; 15% of patients have two or more fractures of the upper cervical spine, while up to 30% of patients have been shown to have noncontiguous spinal fractures. In a small series of complex combined atlantoaxial fractures, only 10% were a TSA. Although the incidence of spinal cord and nerve root injury as a result of a TSA is reportedly low, unstable and atypical hangman’s injuries do occur with some frequency. Combination atlantoaxial injuries seem to have a higher incidence of associated neurologic deficit, likely because of increased instability and reflective of a more severe traumatic injury pattern.
CLASSIFICATION OF TRAUMATIC SPONDYLOLISTHESIS OF THE AXIS
This table describes the most commonly referenced classification systems for TSA (Table 46.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








