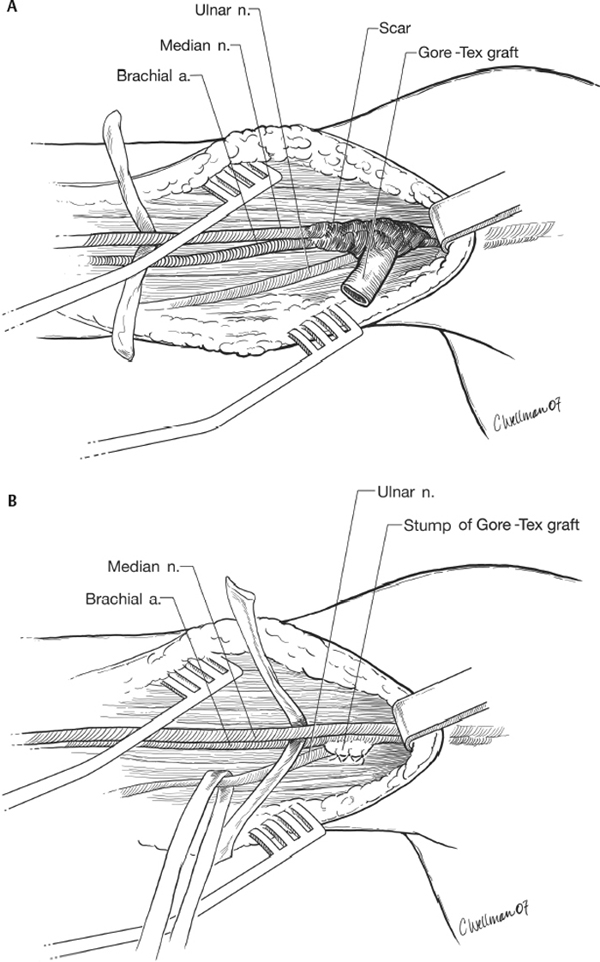
19 Injury to the Median Nerve above the Elbow A 49-year-old female with end-stage renal disease (ESRD) had an arteriovenous (AV) graft placed in the left upper arm. Before the procedure she had complained of some pain and numbness in the left arm and pain in the left hand. She had been told she had carpal tunnel syndrome. After the AV graft procedure she immediately developed numbness and pain in the left arm, elbow, forearm, and hand. It was maximal in the second, third, and fourth digits and extended into the axilla. The graft thrombosed within a short time. The pain became progressively worse and with time extended more to the fifth digit and the axilla. Any movement of the hand was painful. After several visits to the emergency room (ER), the neurosurgery service was consulted. On examination 3 weeks after the AV graft procedure, atrophy of the thenar eminence was noted, with severe limitation of all hand movements due to pain. Although the examination was limited by pain, pronation was weak (grade 1/5), as were flexion of all fingers (2/5), opponens pollicis (1/5), and flexor pollicis longus (1/5). There was possible weakness in the abductor digiti minimi and the interossei (3/5), but examination was limited due to pain. There was decreased sensation to pinprick and touch in the second through fourth digits of the left hand. Electromyographic (EMG) and nerve conduction study revealed low amplitudes of the left median compound action potentials, and the motor nerve conduction velocity was mildly slowed in the forearm. Upper arm study was unreliable and had to be stopped due to patient discomfort. Median sensory action potential was slowed, more in the left middle finger than in the index finger. The ulnar motor and sensory nerve conduction studies showed decreased velocities on the left, but still within normal range. Needle EMG revealed active denervation in the left flexor carpi radialis, flexor digitorum profundus medialis, and abductor pollicis brevis. The ulnar-innervated muscles had normal EMG morphology, but assessment of recruitment was limited by pain. Overall, the impression was of a moderately severe left median neuropathy proximal to the innervation of the flexor carpi radialis, with evidence of active denervation. Operative exposure of the median and ulnar nerves from the elbow up to the axilla and the cord level of the brachial plexus revealed a thrombosed Gore-Tex graft (W. L. Gore and Associates, Inc., Flagstaff, AZ), with a hematoma and scar formation at the anastomosis site with the upper brachial artery. The scar incorporated the median and ulnar nerves in the upper arm. The graft was resected except for a small remnant at the anastomosis site, which was sutured. The scar was removed and neurolysis of both the median and ulnar nerves performed (Fig. 19–1). At 3-month follow-up, the patient had markedly less pain with less guarding. Strength improved to 3/5 in finger flexion, opponens pollicis, forearm pronation, and abductor pollicis brevis. She had better range of motion of the elbow and the wrist. There was no significant change in the sensory examination. Median nerve compression in the upper arm and entrapment by hematoma, mass of the AV graft, and scar The median nerve is formed from lateral and medial cord inputs in the axilla, and usually travels superficial to the brachial artery in the upper arm. Lower in the arm it tends to lie deep and medial to the brachial artery. In the upper arm, the ulnar nerve courses close to the median nerve but on the medial side of the brachial artery. Thus, in the upper arm an injury to the brachial artery or a procedure involving it may result in injury to both the median and the ulnar nerves. The radial nerve lies deeper in the upper arm, penetrating the subscapularis and the long head of the triceps and eventually reaching the lateral side of the arm. High median nerve palsy may occur after injuries such as knife or gunshot wounds, after vascular graft procedures such as in our case, or by blunt compression. Although it occurs more commonly with the radial nerve, the median nerve can also be injured by use of crutches or after the patient’s or the patient’s partner’s head rests for a prolonged period on the medial arm (the so-called Saturday night palsy).
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Anatomy
Anatomy
 Characteristic Clinical Presentation
Characteristic Clinical Presentation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



