18
CHAPTER
![]()
Intracranial EEG Monitoring
Saurabh R. Sinha
In spite of an ever-increasing number of available antiepileptic drugs (AEDs), a substantial portion of patients with epilepsy are intractable to treatment, due to either lack of efficacy or severe side effects. For patients with focal-onset seizures who are intractable to medications (continued seizures in spite of adequate doses of at least two appropriate AEDs), trial of additional medications and medication combinations offer little chance of achieving seizure freedom. In these patients, surgical resection of the seizure focus may offer the best chance for achieving seizure control. The basic requirement for resective surgery for intractable seizures is the ability to localize the “epileptogenic zone” (EZ), the region of the brain that is presumably initiating the seizures (1). More practically speaking, the EZ is the region whose resection/removal will fully control the seizures. Different aspects of the epilepsy surgery evaluation lead to identification of related areas. For example, imaging studies may identify an “epileptogenic lesion” that is the presumed etiology of the seizures; however, the EZ can be within the lesion, near the lesion, or even distant from the lesion. Interictal EEG may identify epileptiform discharges, which identify the “irritative zone”; this zone often includes the EZ but may be larger than, smaller than, or even remote from the EZ. Clinical semiology can help to define regions of the brain involved in the seizure, the “ictal symptomatogenic zone”; however, many brain regions are clinically silent or have nonspecific semiologies. Thus, the ictal semiology may just reflect areas to which the seizure spreads after starting in the EZ. The region of ictal EEG onset (“seizure onset zone”, SOZ) is thought to most closely approximate the EZ in most cases. However, even the SOZ is limited due to the inability to record EEG from the entire cortex and the potential for rapid spread of seizure activity. In some cases, when the SOZ, clinical semiology, “irritative zone,” and “epileptogenic lesion” are concordant, the EZ can be adequately identified by noninvasive means.
A second requirement for resective surgery is being able to assess the risk of the planned resection to eloquent cortex, those regions whose removal would lead to significant functional deficits. This can sometimes be done or presumed based on neuropsychological testing, functional MRI, Wada testing, and the presumed typical function of certain brain regions. However, in many cases, brain mapping is necessary to truly assess the risk of resecting a brain region. When the EZ cannot be adequately localized and/or the risk to eloquent cortex cannot be adequately determined based on noninvasive testing, intracranial recordings are needed to evaluate for epilepsy surgery.
NONINVASIVE EVALUATION FOR EPILEPSY SURGERY
The initial evaluation of a patient for potential epilepsy surgery starts with establishing that the patient has intractable epilepsy (Figure 18.1). It is important to confirm that the patient actually has epileptic seizures and that all the events in question are epileptic. A significant proportion of patients referred to epilepsy centers for evaluation end up having nonepileptic events (most commonly psychogenic nonepileptic seizures), in part or in whole. If the events in question are epileptic, it is important to establish that they are truly intractable. Too often, reported medication failures are actually related to side effects, inadequate dosing, noncompliance, or inappropriate choice of medications. The history should also provide a detailed description of the semiology of all seizure types in a given patient. This can not only provide important hints about the location of the EZ, but can also raise warnings about the potential for multiple foci. Most commonly, however, multiple seizure types described by a patient are actually variable expressions of a single seizure focus; for example, seizures with or without secondary generalization.
It is also important to review any prior evaluation the patient may have had. Routine EEGs can provide hints about areas of neuronal dysfunction (focal slowing) and epileptogenic potential (interictal epileptiform discharges) that may be part of the EZ. Although these should also occur in the video EEG (vEEG) that is an essential part of the evaluation, prior recordings may offer additional information about multiple foci. A high-quality MRI of the brain can also provide important clues about the location of the “epileptogenic lesion.” The MRI should be performed on at least a 1.5T (ideally a 3.0T) scanner with high-resolution T1-weighted images of the entire brain and, in patients with any concern for a temporal lobe focus, thin-cut T2-weighted coronal images through the temporal lobes. Personal review of the MRI is essential as subtle findings like mild cortical dysplasia, early mesial temporal sclerosis, and subtle asymmetries are often not reported in routine MRI reports.

FIGURE 18.1 Flow chart for evaluation of patient with seizures that have not responded to treatment.
Abbreviations: RNS: responsive neurostimulator; VNS: vagus nerve stimulator
![]()
The next step in most evaluations is a vEEG. The primary goal of the vEEG is to record the actual epileptic seizures to better characterize the EZ. It is important to capture the patient’s stereotypical seizures, including different types, if they exist. The vEEG is useful to confirm the semiology of the seizures as well as their EEG features. Patient- and family-reported seizure semiology is often inaccurate or incomplete. The EEG features will ideally lateralize and localize the seizure focus; however, this is sometimes limited due to seizures onset in regions far from the scalp (eg, mesial temporal, orbitofrontal, or midline cortical regions) or in small regions with rapid spread to other, even contralateral regions.
The need for additional testing, like PET and SPECT scans, is usually based on the results of the initial evaluation. For patients with a presumed epileptogenic lesion, if all the data are concordant with the lesion and the lesion is far from eloquent cortex, it may be possible to proceed straight to resection (Table 18.1). However, if the data are discordant or there are other red flags (Table 18.2), intracranial recording is often needed.
CANDIDATE SELECTION FOR INVASIVE MONITORING
As discussed earlier, only when the various pieces of data are concordant and the presumed lesion is far from eloquent cortex can one proceed straight to resection of the presumed epileptogenic lesion. In most other circumstances, including nonlesional cases (Figure 18.2), invasive monitoring is needed in order to localize the EZ and resect it safely. For lesional cases (Figure 18.3), intracranial recording may still be required if the various pieces of data are not concordant, if the lesion/etiology is one commonly associated with multifocality, or if the lesion is close to eloquent cortex. If the data still localize to a single hemisphere or a region of a single hemisphere, unilateral electrode implantation may be adequate (Phase IIB monitoring, see definition later). However, if the discordant data raises the concerns for both the hemispheres or widespread regions within a single hemisphere, a multistep surgical process may be needed: first implanting electrodes through burr holes to cover both the hemispheres or widespread regions (Phase IIA, see later) followed by Phase IIB over the region found in Phase IIA monitoring.
TABLE 18.1 Requirements for Epilepsy Surgery Without Invasive Recording
1. Well-localized ictal-EEG 2. Semiology consistent with presumed seizure focus 3. Lesion on structural or functional imaging studies consistent with seizure focus 4. Absence of other potentially epileptogenic lesions on imaging or EEG 5. Seizure focus remote from know/presumed eloquent cortex 6. Presumed etiology of epilepsy does not predispose to diffuse or multiple foci: tumor, vascular malformation, mesial temporal sclerosis |
TABLE 18.2 Red Flags From Noninvasive Epilepsy Surgery Evaluations
1. Discordant data: interictal EEG, ictal EEG, semiology, imaging studies 2. Nonlesional cases 3. Ictal-EEG pattern significantly delayed compared to clinical onset 4. Proximity of presumed seizure focus to eloquent cortex 5. Presumed etiology of epilepsy predisposes to diffuse or multiple foci: cortical dysplasia, h/o encephalitis, h/o trauma |
TYPES OF INVASIVE MONITORING
Invasive monitoring can be done both acutely (in the operating room only) and “chronically” (for days to weeks using implanted electrodes). In the acute situation, electrodes are placed by the surgeon during the operation. These can be used to identify interictal discharges and map brain function. Ictal recordings are usually not possible; however, in some circumstances, the interictal data and brain mapping results may be enough to proceed to resection. Much of early epilepsy surgery was performed using only acute recordings.
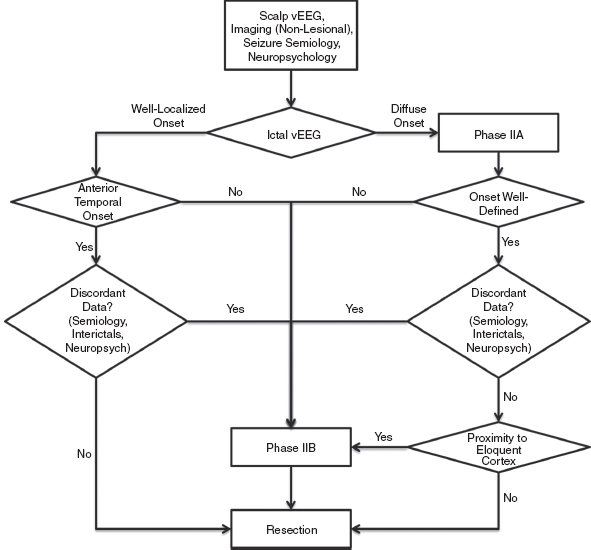
FIGURE 18.2 Flow chart for evaluation of patient with intractable focal-onset seizures without a potentially epileptogenic lesion on imaging.
![]()
FIGURE 18.3 Flow chart for evaluation of a patient with intractable focal-onset seizures with potentially epileptogenic lesion on imaging.
![]()
However, most invasive monitoring now involves the chronic implantation of electrodes. This is referred to as Phase II monitoring. As mentioned previously, Phase II can be further subdivided into IIA and IIB. The key distinction is that at end of Phase IIB, the intention is to have collected all the data needed to resect the epileptogenic focus at the time of electrode removal. Phase IIA usually involves a more widespread sampling of the brain using electrodes implanted over a wide region, often bilaterally. The goal of Phase IIA is usually to lateralize the epileptogenic focus and possibly roughly localize it to a specific lobe or region; at the end of monitoring, the electrodes are removed without a resection being performed. In most cases, phase IIB monitoring is subsequently performed prior to actual resection of the focus (see Figure 18.4). A subset of phase IIA patients may be able to proceed to resection without additional intracranial monitoring—usually those where seizures are ultimately localized to the anterior or mesial temporal lobe. Another subset may be found not to be candidates for respective surgery—for example, if phase IIA reveals clearly multifocal seizures.
PLANNING OF INVASIVE MONITORING
Although invasive monitoring provides significant advantages for localizing the focus and mapping brain function, there are some important limitations to keep in mind. The most important is the potential for sampling error. Signals are only obtained from tissue immediately underlying/surrounding the electrode. Thus, any brain regions not covered by electrodes will not be recorded. Invasive monitoring must be approached as a hypothesis-driven exercise. Based on the results of the noninvasive evaluation (EEG, semiology, imaging), one should identify candidate regions for the EZ. Special attention should be paid to structures that are not well recorded by scalp EEG or that produce nonspecific or subtle semiologies. Electrode coverage must be planned to allow for both identifying the EZ and ruling out other candidate areas (Table 18.3). It may also be important to cover areas to insure that eloquent cortex can be confidently identified using brain mapping. Based on these requirements, one can very quickly formulate a plan involving numerous electrodes. This has to be tempered by the higher risks for infection, herniation, patient discomfort, and other complications posed by larger numbers of electrodes (2).
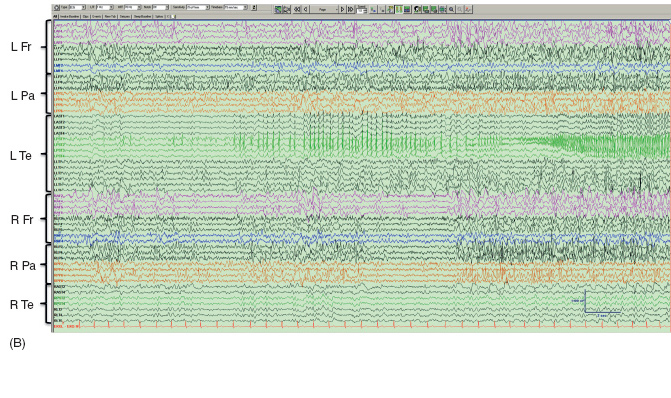
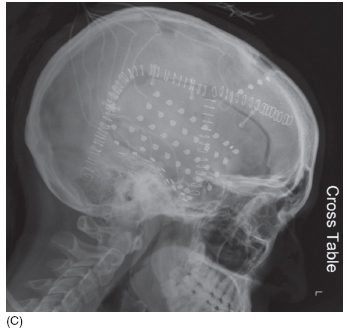
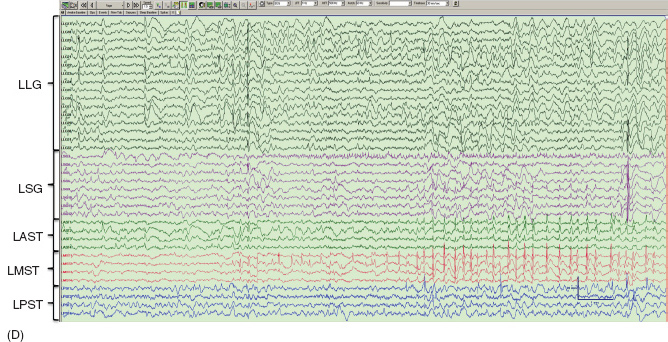
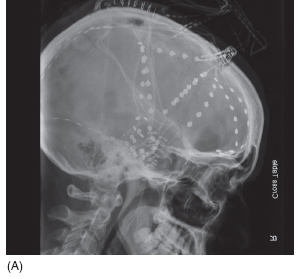
FIGURE 18.4 ECoG of clinical seizures in an adult patient who underwent multistage evaluation for intractable seizures since childhood and nonlesional imaging. Scalp recording was nonlateralizing. (A) Lateral skull x-ray showing electrode placement for Phase IIA. Electrodes were inserted through three burr holes on both sides of the head. (B) Habitual clinical seizure showing onset in the L temporal region (LPST1-2) with spikes. Electrodes are grouped by brain region. Every other contact is shown. (C) Lateral skull x-ray showing electrode placement for Phase IIB. A 4 × 8 grid (LLG) was placed over the left lateral temporal lobe. A 2 × 6 grid (LSG) was placed in the subtemporal/suboccipital region. Three strips (LAST, LMST, and LPST) were placed over the subtemporal surface. (D) Habitual clinical seizure showing onset in the anterior portion of the subtemporal grid (LSG3) with slowing/sharp waves, followed by alpha frequency activity. The pattern spreads rapidly to nearby LMST. The patient underwent a left temporal resection (mainly inferior).
Abbreviations: Fr: frontal; L: left; Pa: parietal; R: right; Te: temporal.
![]()