Histology
No. of cases
Total
Subtotal
Paragangliomas
74
58a
16b
Schwannomas
19
19
00
Meningiomas
13
07
06
Aneur. bone cyst
02
02
00
Chondrosarcoma
07
01
06
Chordoma
07
00
07
Malignant tum.
06
00
06
Cholesteatoma
02
01
01
Chondroma
01
01
00
Lymphangioma
01
01
00
Inflam. granuloma
02
01
01
Total
134
91 (69 %)
43 (31 %)
Table 28.2
Jugular foramen meningiomas
Histology | No. of cases | Total | Subtotal |
|---|---|---|---|
Meningotheliomatous | 7 | 6 | 1 |
Anaplastic | 3 | 0 | 3 |
Papillary | 2 | 1 | 1 |
Microcystic | 1 | 0 | 1 |
28.1.2 Radiologic Diagnosis
A combination of contrast-enhanced computed tomography (CT) scanning, magnetic resonance imaging (MRI), and angiography is ideal for proper diagnosis and localization of the tumors. High-definition CT scan examination is useful to study the bone structures of the cranial base, bone erosion, tumor calcification, hyperostosis especially in cases of meningiomas, aneurysmatic bone cysts, and chondrosarcomas (Fig. 28.1). Preoperative MRI with gadolinium (Gd) is very useful to demonstrate the characteristics of tumor and its vascularization, extension, and relationship with neighboring structures. MR angiography is performed to study tumor vascularization, venous circulation, and occlusion of the sigmoid sinus. Paragangliomas are well-vascularized lesions, with heterogeneous Gd enhancement (Fig. 28.2). Vascular flow voids shown on MRI are characteristic of paraganglioma. Schwannomas enhance homogenously Gd, present a regular contour, gradually enlarge the JF by pressure erosion and give an expanded and scalloped but well-defined corticate margin to the JF, may be cystic, and in some cases present an extension into the high cervical region (Fig. 28.2). Meningiomas present Gd enhancement that may extend into the cervical region and present a “dura tail” (Fig. 28.3). Meningiomas arising primarily in the jugular foramen show diffuse skull base infiltration which differentiates primary jugular tumor from meningioma that involves the jugular foramen secondarily. Chordomas and chondrosarcomas are heterogeneous, presenting some areas with contrast enhancement. Digital subtraction angiography (DSA) is performed for diagnosis and to guide preoperative embolization in cases of highly vascularized lesions. DSA is routinely performed when the lesion is well vascularized. Branches of the external carotid artery (ascending pharyngeal artery) are usually feeders of JF paragangliomas. Invasion of the walls of the internal carotid artery may become visible in angiography. Patients harboring lesions surrounding or invading the ICA are submitted to balloon test occlusion. In these cases sacrifice of the ICA may be necessary. When the tumor is hypervascularized, feeders from the external carotid artery (ascending pharyngeal, internal maxillary, and occipital arteries), from the internal carotid (carotid tympanic branches), and from the vertebral artery (posterior inferior cerebellar artery) are embolized with Gelfoam®, Ivalon® particles, or Onyx® through super-selective catheterization, 3–5 days prior to surgery. The venous circulation, position, and patency of jugular bulb are better evaluated with the venous phase of DSA. A highly located and hypertrophic jugular bulb may cause symptoms of tinnitus and hearing loss. It is easily demonstrated by the venous phase of DSA.
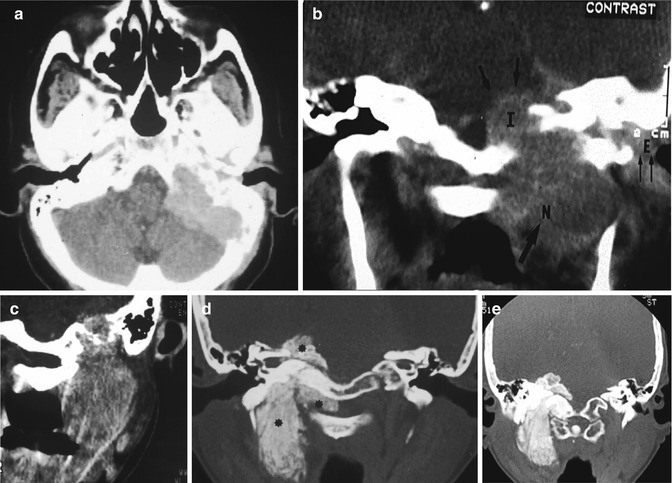
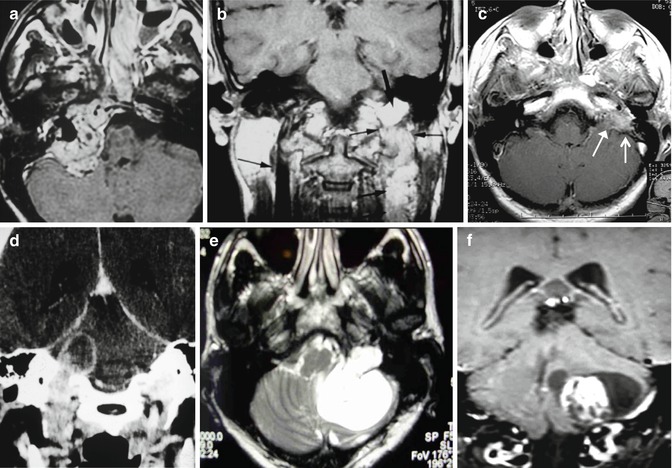
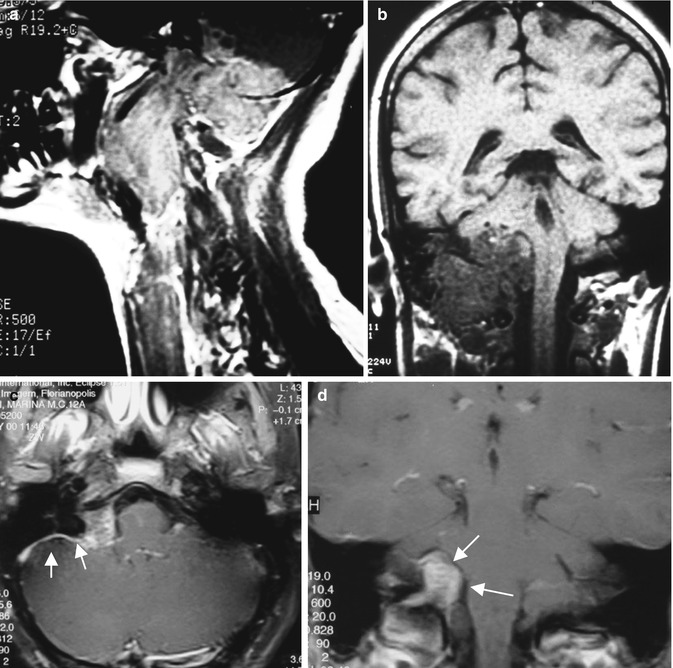
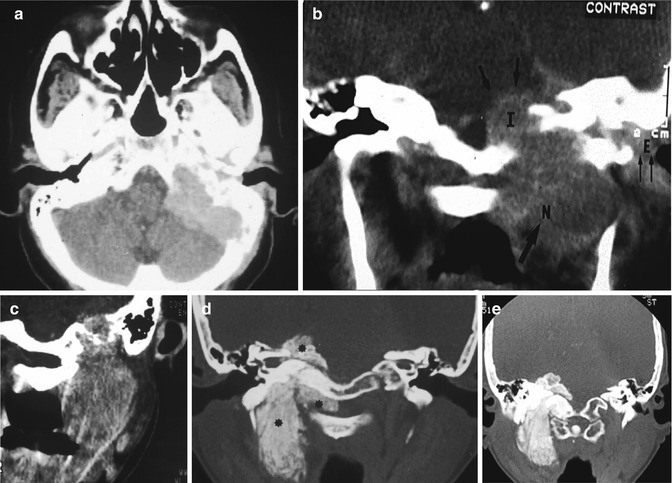
Fig. 28.1
CT scan examination of large paragangliomas (a–c) and a large calcified JF meningioma (d, e) involving the spinal canal
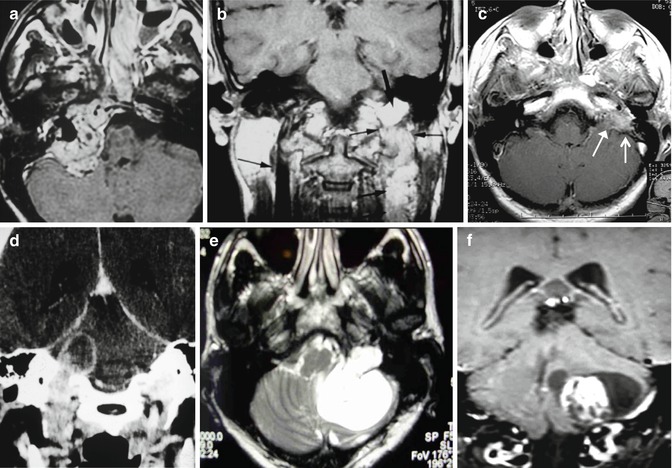
Fig. 28.2
MRI of JF paragangliomas (a–c) and cystic JF schwannomas (d–f)
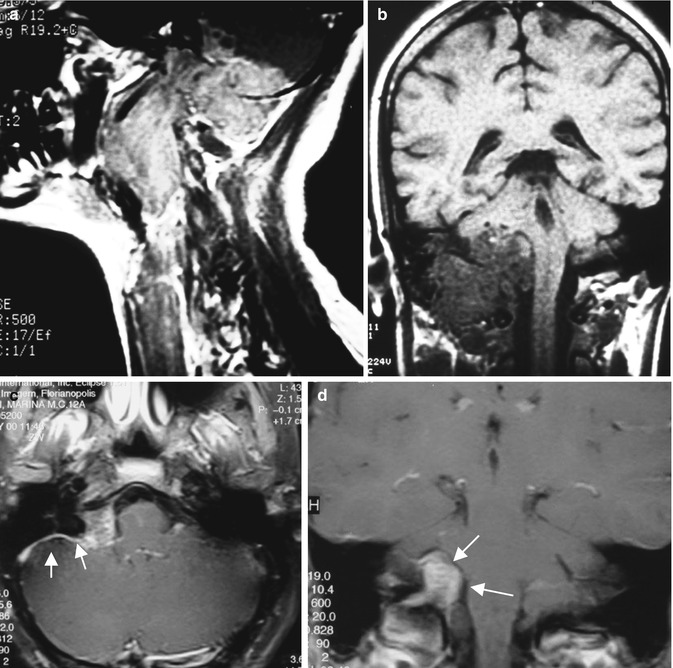
Fig. 28.3
MRI images of a large JF meningioma (a, b). (c, d) Small JF meningioma. (c) Arrows = “dura tail”
28.2 Surgical Technique
28.2.1 Surgical Anatomy
Anatomically the JF is described as having two portions, the nervous and the venous. The nervous portion contains the glossopharyngeal nerve, the inferior petrosal sinus, and the meningeal branches of ascending pharyngeal artery and the venous portion contains the sigmoid sinus, vagus, and accessory nerves. Other authors divide the JF in three portions [26]: two venous and one nervous (intrajugular). The nervous portion is localized between the two venous and contains the nerves IX, X, and XI. The cranial nerves are located anteromedial to the jugular bulb and maintain a multifascicular histoarchitecture (particularly the Xth cranial nerve) [57]. The vagus nerve is formed by multiple fascicles and the glossopharyngeal and accessory nerves by one and two fascicles, respectively. The tympanic branch of glossopharyngeal nerve (Jacobson’s nerve) and the auricular branch of vagus nerve (Arnold’s nerve) cross the JF. Intradurally the JF is related to the caudal cranial nerves IX, X, and XI (with its spinal portion); the nerves VII and VIII; the vertebral, posterior inferior, and anterior inferior cerebellar arteries; the lower brain stem; and the upper cervical cord. The anatomical parameters to expose the facial nerve at the stylomastoid foramen region are the following: the mastoid tip posteriorly, the “pointer” superiorly, and the posterior belly of the digastric muscle inferiorly. The structures of temporal bone related to the surgical approach to the JF are as follows: the sigmoid; the transverse, superior, and inferior petrosal sinuses; the mastoid cells and its antrum; the semicircular canals; the ossicles; the facial nerve canal; and the tympanic bone. The internal carotid artery runs medial to the tympanic bone and gives off the carotid-tympanicum branches. Anatomical structures related to neck dissection are the following: muscles (anterior border of the sternocleidomastoid muscle (SCM), the digastric, splenius capitis, obliquus capitis superior and inferior, splenius cervicis muscles), vessels (common carotid, external carotid artery with its branches and internal carotid arteries, vertebral artery at the cranial cervical junction, common facial vein, and external and internal jugular veins), and nerves (greater auricular nerve; cranial nerves X, XI, and XII; and the sympathetic trunk).
28.2.2 Position of Patient and Skin Incision
All patients are placed in the dorsal position with the head held in a Mayfield clamp and turned 45° to the opposite side. The contralateral internal jugular vein must be free. The facial, cochlear, and caudal cranial nerves are monitorized. All contact areas are protected for the long duration of the procedure. A nasogastric tube is inserted. Skin incision is C-shaped, starting in the temporal region going down circumscribing the ear as far as the anterior border of the SCM muscle (Fig. 28.4). After folding anteriorly the skin scalp, the great auricular nerve is identified. This nerve may be used as graft to reconstruct the facial nerve. The external auditory canal is exposed. If the patient has no hearing and there is tumor invasion with destruction of the ossicular chain, it is cut at the osteocartilaginous junction. The external auditory canal is closed in two layers to avoid CSF fistula.
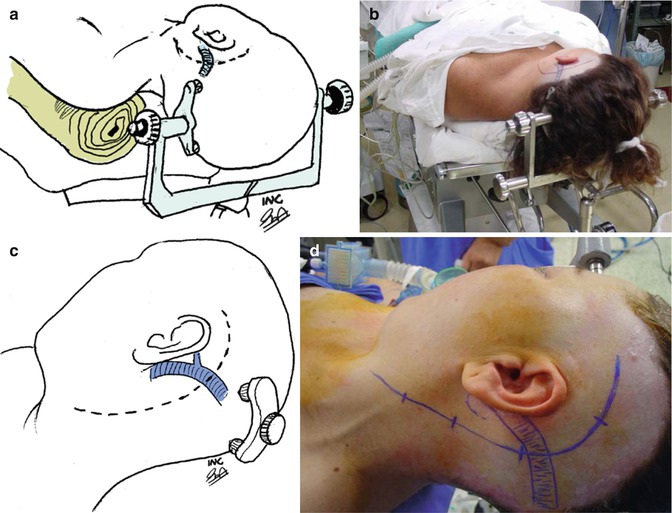
Fig. 28.4
(a, b) Patient’s position. (c, d) Skin incision
28.2.3 Reconstruction of the Cranial Base
The large surgical defect will be closed in three layers. This technique of skull base reconstruction using vascularized tissues and fascia muscle flaps was developed by our group to avoid postoperative CSF leaks and obtain good cosmetic results [46]. The first layer is watertight dura closure or use of a temporalis fascia graft with fibrin glue if resection of the infiltrated dura was performed and primarily dura closure was not possible. Use of abdominal fat graft is avoided. The second layer is a vascularized temporalis muscle flap (Fig. 28.5). The posterior half of the temporalis muscle is incised, dissected, turned down, and sutured to the cervical and parotid fasciae covering the dura mater at the end of surgery and filling the surgical defect in the mastoid cavity. The third layer is a myofascial flap formed by the temporalis muscle fascia, cervical fascia, and sternocleidomastoid muscle (STM) (Fig. 28.5). The temporalis muscle fascia is incised in the middle portion of the temporal region and dissected inferiorly as far as the temporal line. The cervical fascia is cut posterior to the external auditory canal, mastoid tip, and over the STM. The insertion of the STM is removed from the mastoid, and a vascularized myofascial flap formed by the temporalis muscle fascia, the cervical fascia, and the STM is turned posterior and inferiorly. This flap is secured with sutures in the temporalis fascia and in the parotid and cervical fascia. It is turned back to cover the temporalis muscle flap and the entire surgical field. After preparing these flaps we go on for the next surgical step, neck dissection.
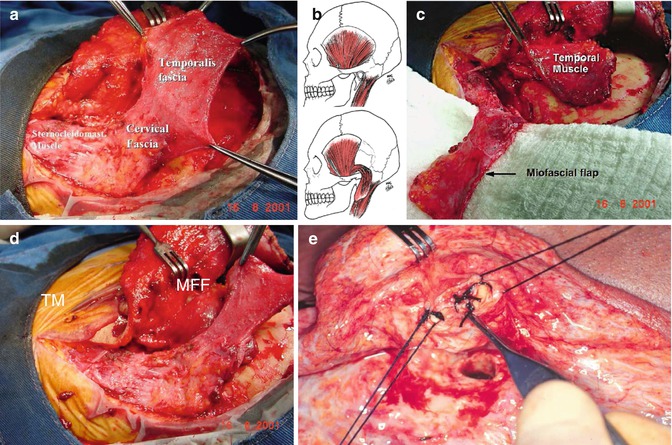
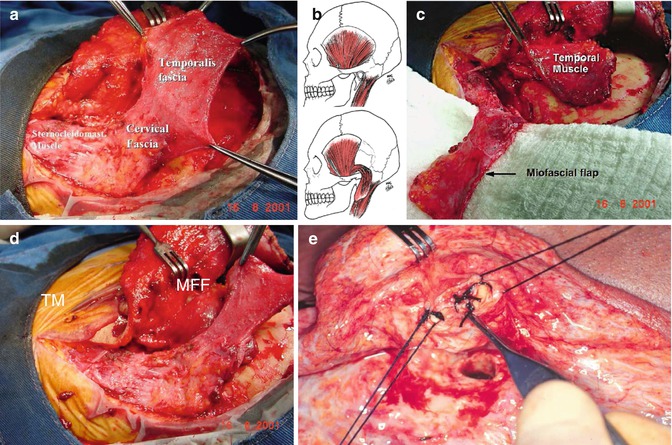
Fig. 28.5
Reconstruction technique. (a) Myofascial flap (MFF), (b, c) temporal muscle (TM) rotation, (d) rotation of myofascial flap, (e) suture of external auditory canal
28.2.4 Neck Dissection
The anterior border of the STM is identified and the major vessels of the neck (common CA, ICA, external CA and its branches, and IJV) are dissected (Fig. 28.6). The external jugular vein is ligated with suture/ligature and cut. A key muscle for neck dissection is the digastric muscle. The digastric muscle is used as a guide for dissection of the VII and XII cranial nerves. The cranial nerve XII crosses the external carotid artery inferior to the digastric muscle. In the majority of cases, the accessory nerve is located laterally to the internal jugular vein crossing the external carotid artery inferiorly to the digastric muscle. The X cranial nerve and the sympathetic trunk run latero-inferior to the common carotid artery (Fig. 28.7). The vertebral artery is dissected at the lateral process of C1. Proximal control of this vessel is important in infiltrative tumors of the posterior fossa.
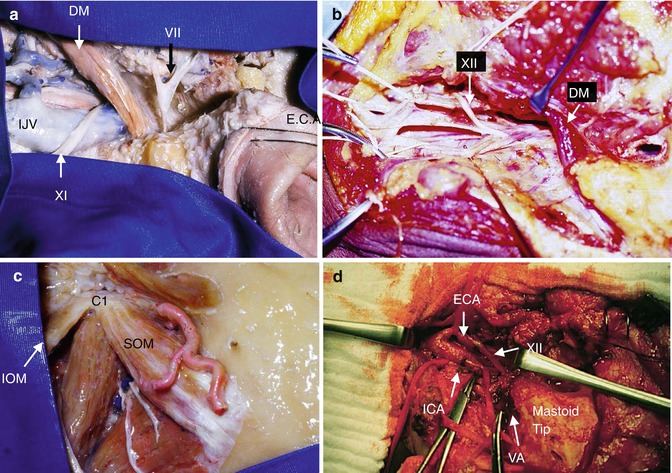
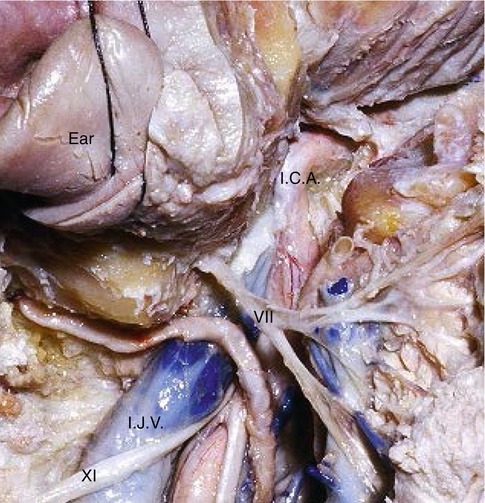
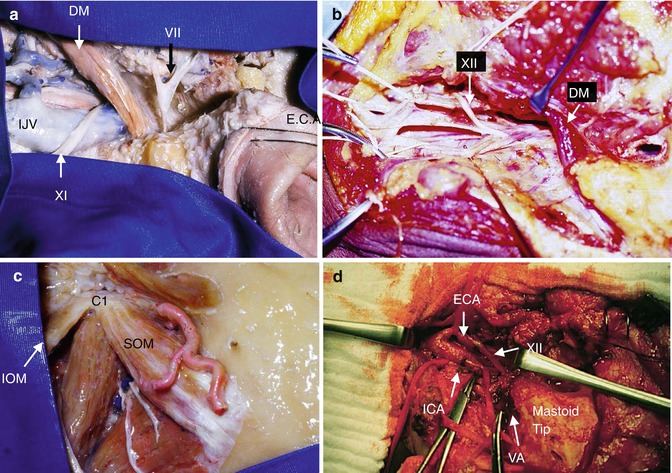
Fig. 28.6
(a–d) Anatomical specimen showing neck dissection. Digastric muscle (DM), cranial nerves VII, XI, and XII, internal jugular vein (IJV), external carotid artery (ECA), internal carotid artery (ICA), vertebral artery (VA), superior and inferior oblique muscles (SOM and IOM). (d) Neck dissection
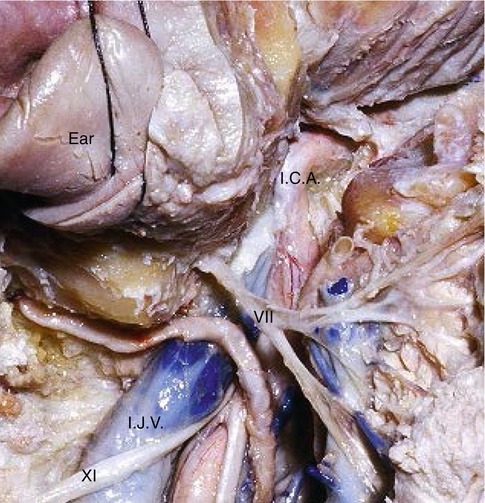
Fig. 28.7
Anatomical specimen: internal jugular vein (IJV), internal carotid artery (ICA), facial nerve (VII) and the XI cranial nerve
28.2.5 Facial Nerve Management
The facial nerve exits the stylomastoid foramen superiorly to the digastric muscle. This nerve is identified at the stylomastoid foramen using the following parameters: the mastoid tip, the posterior belly of the digastric muscle, the “pointer,” and the tympanomastoid suture (Fig. 28.8). If this nerve is not infiltrate by the tumor, it is not necessary to remove it from its bony canal. Tumor is resected anteriorly and posteriorly to the facial canal. This technique avoids postoperative facial paralysis by rerouting the seventh cranial nerve. Facial nerve reconstruction is accomplished with grafts from great auricular or sural nerves if the nerve is infiltrated and must be resected.
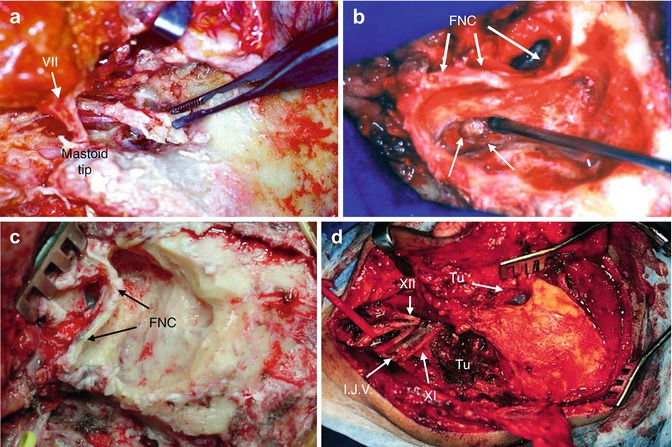
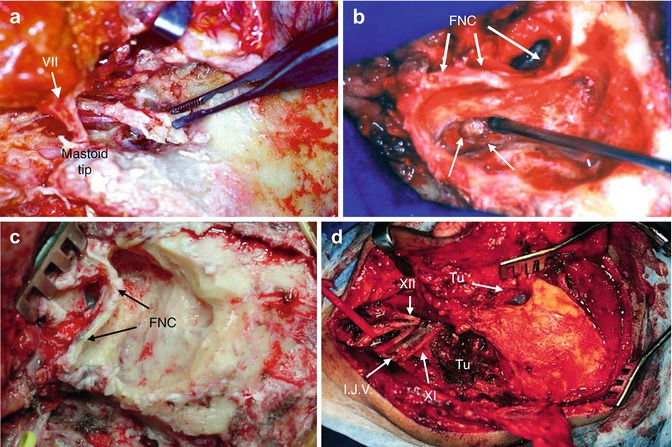
Fig. 28.8
(a) Facial nerve (VII) dissection. (b, c) Mastoidectomy, facial nerve canal (FNC), retrofacial mastoid cells (arrows). (d) Extradural tumor exposure
28.2.6 Temporal Bone Dissection
Temporal bone dissection and radical mastoidectomy is performed with identification of the facial nerve canal, the labyrinth, the mastoid antrum, the ossicles, and the sinodural angle (Fig. 28.8). The sigmoid sinus and the jugular bulb are completely skeletonized. The retrofacial mastoid cells are removed. The posterior and anterior walls of the external auditory meatus are drilled to better expose the tumor in the ear (Fig. 28.8). Tumor within the ear, eustachian tube, and mastoid cells is resected after removal of the tympanic membrane. Removal of the tympanic bone exposes the internal carotid artery (distal control) allowing bipolar coagulation of the carotid-tympanic branches (branches of ICA) that very often are tumor feeders.
28.2.7 Craniectomy and Opening of the Jugular Foramen
A small craniectomy (3 cm in diameter) exposing the posterior fossa dura and the posterior portion of the JF is the next surgical step (Fig. 28.9). The emissary mastoid vein is coagulated and cut. The sigmoid sinus is totally dissected. Tumor within the cervical region and jugular bulb is exposed by widely opening of the JF, communicating the cervical with the cranial portion of JF. The lateral process of C-1 and the posterior border of the JF are removed with a drill and a small Kerrison punch to enlarge JF exposition.
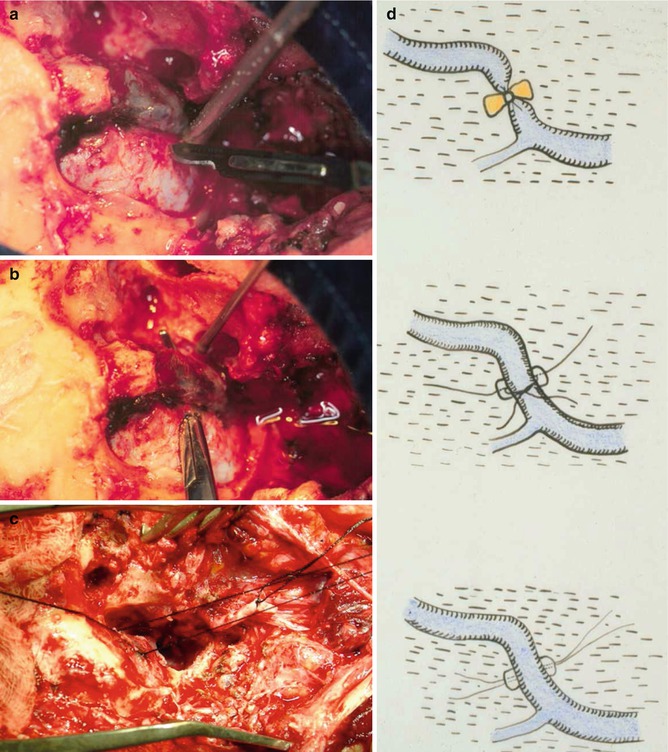
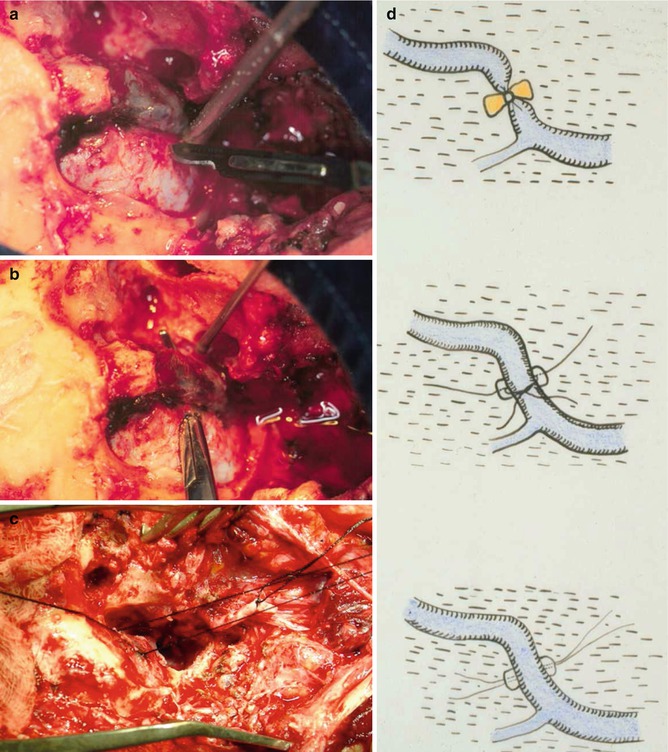
Fig. 28.9
(a) Craniectomy, dura incision posterior to the sigmoid sinus. (b) “Mosquito” clamp under the sigmoid sinus. (c) Sigmoid sinus ligature. (d) Drawing showing sigmoid sinus ligature technique
28.2.8 Extradural Tumor Removal
Small dura incisions are performed in front and behind the sigmoid sinus, below the superior petrosal sinus. The sigmoid sinus is ligated with two sutures (Fig. 28.9). The internal jugular vein is double ligated (suture/ligature). After all this surgical dissection removal of the extradural tumor is accomplished. The posterior wall of the sigmoid sinus is incised and the intraluminal portion of the lesion is dissected with microsurgical techniques from the anterior wall of the sigmoid sinus and jugular bulb. Bleeding from the inferior petrosal sinus may occur. This sinus is packed with Gelfoam® or Surgicel® after complete tumor removal from JF. Tumor extensions anteriorly compressing the internal carotid artery and infiltrating the tympanic bone are dissected and removed (Fig. 28.10). In case of tumors not invading the sigmoid sinus like the schwannomas, tumor removal may be accomplished without ligation of the sigmoid sinus.
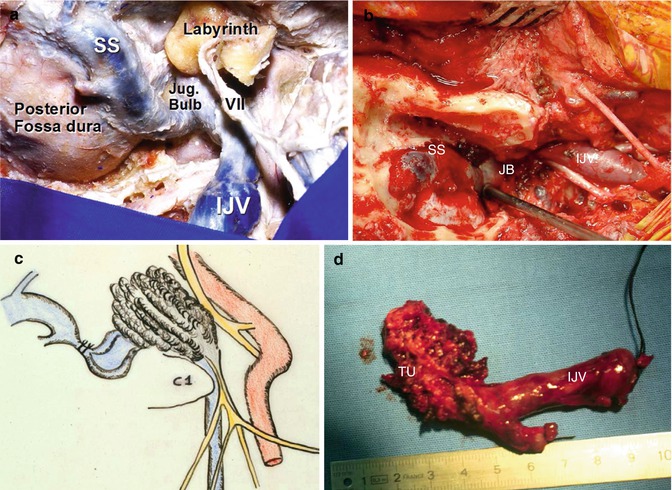
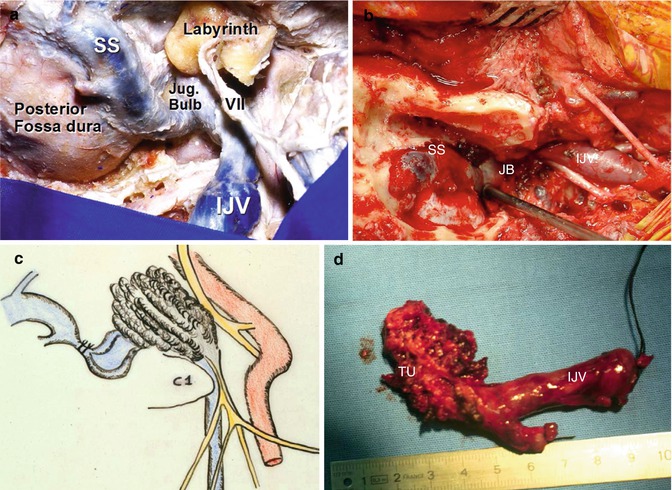
Fig. 28.10




(a) Anatomical specimen showing the internal jugular vein (IJV), jugular bulb (JB), and sigmoid sinus (SS). (b) Surgical picture. (c) Drawing showing SS ligation and extradural tumor removal. (d) Surgical specimen – paraganglioma. Tumor removed from the jugular foramen (TU)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








