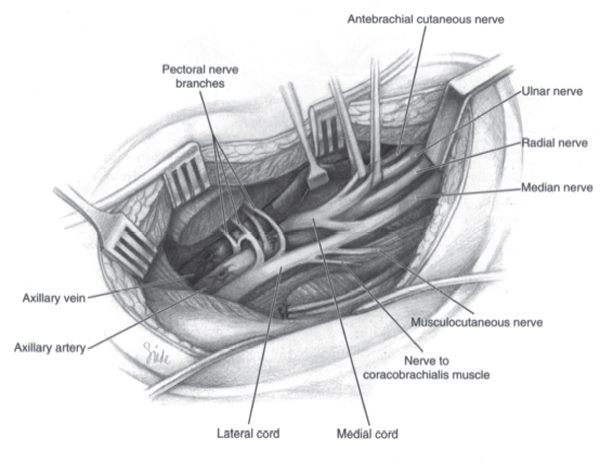
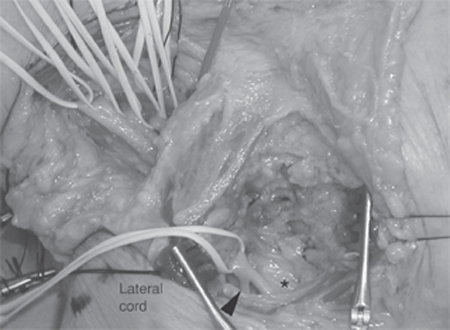
5 Lateral Cord Injury An 18-year-old man was seen in a local emergency room due to an accidental, self-inflicted gunshot wound. The history provided was that he had loaded an SKS rifle in the dark and did not realize that a 0.76 caliber bullet was in the chamber when the magazine clip was inserted into the rifle. The rifle discharged directly into the middle of his right pectoralis major muscle a half-inch below the clavicle, and the bullet exited posteriorly in the axilla. On examination in the emergency room, there was a thready distal radial pulse and initially no motor or sensory function of the distal arm or hand. An arteriogram was performed, which revealed no vascular injury. No major intervention was deemed to be necessary at that time. The patient was seen in clinic 1 month after his gunshot wound. The arm was in a sling and the patient was protective of the arm and forearm. He was able to abduct the arm with 5/5 strength with evidence of good deltoid contraction. External rotation strength was decreased at 4/5 but with give away weakness felt to be related to his shoulder pain. Elbow flexion was limited to 10 degrees passive flexion and extension from the arm in 90 degrees of flexion. No biceps contraction was palpable. The brachioradialis muscle contracted and was felt to be responsible for the 3/5 elbow flexion observed. Pronation and supination could not be evaluated due to the relatively frozen elbow. The triceps function was at least 3/5. Distal function of the hand revealed 4/5 strength of the flexor digitorum superficialis and profundus. The intrinsic hand muscles were all 4/5 in function. Sensory examination revealed a defect in pin perception in the distributions of the lateral antebrachial cutaneous nerve and the median nerve. Sensation was relatively preserved in the axillary, ulnar, radial, and medial antebrachial cutaneous distributions. A good radial pulse was palpable. Gunshot (rifle) injury to the brachial plexus Figure 5–1 The right infraclavicular brachial plexus has been exposed via an incision through the deltopectoral groove. The lateral cord is identified most superficially, lateral to the axillary artery. The branches from the lateral cord are seen from proximal to distal: lateral pectoral, coracobrachialis, musculocutaneous, and lateral cord contribution to the median nerve. (From Kline DG, Hudson AH, Kim DK. Atlas of Peripheral Nerve Surgery. Philadelphia: WB Saunders; 2001:26, Fig 3.8. Reprinted with permission.) The lateral cord is the most anterior of the cords in routine dissection and is most often the first revealed in anterior exposure of the infraclavicular brachial plexus (Fig. 5–1). Its correct identification is crucial, particularly when function is absent and anatomy must be relied upon for proper identification of all the plexus elements. The lateral cord starts its existence as a discrete neural element just distal to the clavicle with the union of the anterior divisions of the middle and upper trunks under cover of the pectoralis minor muscle. It then courses in fatty tissue under a thin fascial plane, which inserts upon the pectoralis minor muscle. One or occasionally two lateral pectoral nerves are given off at this level, although sometimes they arise just proximal to the junction of the anterior divisions of the middle and upper trunks. As the lateral cord continues distally, a lateral branch to the coracobrachialis muscle is usually given off after the nerve leaves the underside of the pectoralis minor muscle. Distal to this branch the nerve usually splits into its final derivatives. The lateral branch becomes the musculocutaneous nerve and the medial branch joins the contribution from the medial cord to become the median nerve. At this point the axillary artery has assumed a more anterior position and is just medial to the lateral cord (Fig. 5–2). It is important to realize that this final branching pattern of the lateral cord is one of the most variable with respect to brachial plexus anatomy. Not infrequently the lateral cord will give off more than one branch, which joins with a branch from the medial cord to give rise to a smaller caliber median nerve. Another variation is to have no proximal branches and to give branches to the median nerve more distally in the arm. The combination of biceps paralysis and sensory loss in the median nerve distribution localizes the injury to the lateral cord. Neurapraxic lateral cord injury Axonotmetic lateral cord injury Neurotmetic lateral cord injury Electromyographic examination revealed no motor unit potentials in the biceps brachii and the pronator teres muscles with profuse fibrillation potentials. No sensory potentials were elicitable from digits 1 through 3 in the hand or from the lateral antebrachial cutaneous nerve. Shoulder x-ray confirmed that there were no retained bullet fragments. The initial treatment in this man was to maintain full range of motion of all joints. He had been put into a sling and continued to use this device without regard for the flexion contracture it generated. Because a high proportion of gunshot wounds recover spontaneously, expectant management is the proper initial course. If no recovery is evidenced by 3 to 6 months, operative exploration with nerve action potential recordings and repair of damaged neural elements will be in order.
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Anatomy
Anatomy
 Characteristic Clinical Presentation
Characteristic Clinical Presentation
 Differential Diagnosis
Differential Diagnosis
 Diagnostic Tests
Diagnostic Tests
Management Options
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



