, Thomas Verse2, Nico de Vries3 and Joachim T. Maurer4
(1)
Department of Otorhinolaryngology Head and Neck Surgery, University Hospital Mannheim, 68135 Mannheim, Germany
(2)
Department of Otorhinolaryngology Head and Neck Surgery, Asklepios Clinic Harburg, Eissendorfer Pferdeweg 52, 21075 Hamburg, Germany
(3)
Department of Otolaryngology, Saint Lucas Andreas Hospital, 9243, 1006, AE, Amsterdam, The Netherlands
(4)
Department of Otorhinolaryngology Head and Neck Surgery, Sleep Disorders Center University Hospital Mannheim, 68135 Mannheim, Germany
Abstract
Radiofrequency surgery of the tongue base is the only minimally invasive surgical treatment for retro-lingual obstruction in obstructive sleep apnea. Radiofrequency surgery may be performed as an insolate approach or in a multilevel surgical concept. The feasibility of interstitial radiofrequency treatment (RFT) of the tongue base was first investigated in a porcine model [576] using the Somnus unit. The authors found a mild initial edematous response that tapered off 24 h after surgery. Ten days after RFT, a volume reduction was documented at the treatment site. The procedure turned out to be safe and was transferred to use in patients suffering from obstructive sleep apnea.
7.1 Interstitial Radiofrequency Treatment (RFT)
Core Features
Radiofrequency surgery of the tongue base is the only minimally invasive surgical treatment for retro-lingual obstruction in obstructive sleep apnea.
Radiofrequency surgery may be performed as an insolate approach or in a multilevel surgical concept.
The feasibility of interstitial radiofrequency treatment (RFT) of the tongue base was first investigated in a porcine model [576] using the Somnus unit. The authors found a mild initial edematous response that tapered off 24 h after surgery. Ten days after RFT, a volume reduction was documented at the treatment site. The procedure turned out to be safe and was transferred to use in patients suffering from obstructive sleep apnea.
7.1.1 Surgical Technique
We prefer performing RFT of the tongue base under local anesthesia. In upright position, the patient is comfortably seated either in the clinical chair or on a surgical table. As perioperative monitoring, we initiate an ECG and a pulse oximetry. In contrast to the application at the nasal concha and the soft palate, sedation is recommended in this case. We administer sedation intravenously with Midazolam, by titrating the drug up to the desired level of sedation. Also, in contrast to the application of the RFT on the soft palate, we consider a perioperative antibiotics prophylaxis as essential in the application of RFT on the tongue base. We administer 2 g Cephazolin intraoperatively and perform a postoperative prophylaxis for 5 days with 500 mg Cefuroxim two times daily per os. In terms of cost-efficiency, a different antibiotic management, e.g., with an oral penicillin, can certainly be envisioned. Yet, a general omission of an antibiotic prophylaxis is not recommended.
Following an optional surface disinfection with Hexetidine 0.1%, an infiltration anesthesia is performed. We use 2% Prilocain with adrenalin additive (1:200,000). We do not perform a surface anesthesia because some patients develop a discomforting hypersalivation, which can impede the patient’s cooperation. Between 5 and 10 mL, local anesthetic is applied.
We employ different RFT systems. Among others, we use the Celon system (Celon AG Medical Instruments, Teltow, Germany) and the instruments provided by Sutter (Sutter Medizintechnik, Freiburg, Germany), both being bipolar-controlled systems (for more information, see Sect. 6.1.2). The vast majority of study was performed with the Somnus device (Somnus, Gyrus ENT, Bartlett, USA), a monopolar system which necessitates the attaching of a neutral electrode to the patient. Using this system, we were able to realize a series of in vitro and MRI-based in vivo studies regarding lesion sizes and optimal energy application. A setting of 600 J with a target temperature of 85°C creates optimal lesions [716, 717]. Therefore, we have substantial evidence to recommend this setting. Nevertheless, due to practical considerations, especially the time needed for energy application and the declining distribution of the system in Europe, we have discontinued its use. When using the Celon system, we set the generator to an output of 6-7 W (Fig. 7.1.1). With the Sutter system, 14 W in the autostop mode appears to be the optimal setting. In general, the lower the output is set, the larger the lesions in the tissue will become.


Fig. 7.1.1
Radiofrequency generator Celon with foot switch
Given the high number of lesions, it is difficult to maintain a fixed application pattern for repeated treatment sessions. Nevertheless, one should attempt to avoid placing the application needle twice on the same location. The idea of multiple treatment session goes back to the initial publications using the Somnus unit, where lesion formation takes significant amount of time. Due to the limited experiences, only 2-4 lesions were applied in the beginning. With the more rapid bipolar systems, up to 10 or 12 lesions or more may be created in one session depending on the system used without increasing the associated morbidity in a relevant way. We now consider radiofrequency surgery of the tongue base as a single-step procedure.
It is much more difficult to penetrate the tongue surface than the surface of the soft palate. Therefore, special device needles are necessary for the application at the base of tongue. Together with Celon, we have developed a special faceted tongue base applicator, the so-called Celon Pro Sleep Plus (Fig. 7.1.2). The applicator is covered in a synthetic coat. Only the tip of the probe with the active electrode is exposed. The coat prevents the applicator from being inserted too far into the tissue. This reliably protects deeper lying structures, as for example the neurovascular bundle of the tongue. Substantial additional force would be needed in order to push the probe beyond the coat into the tongue. A radiofrequency energy application accidentally going too deep is made all but impossible. Comparable protection systems are realized with the majority of radiofrequency systems used to date. Nevertheless, special care for correct needle placement should be taken at any time. In Fig. 7.1.3, needle placement during surgery is demonstrated. The lesions should be as posterior as possible at the base of tongue in an area around or posterior to the wall papilla (see Fig. 7.1.4). The needle has to be inserted in an angle as close to 90° as possible to avoid superficial lesions with associated ulceration (see morbidity and complications).
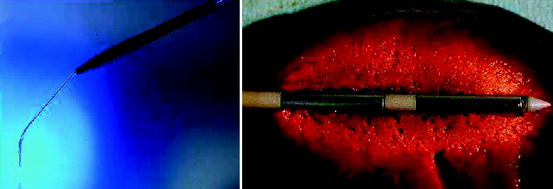

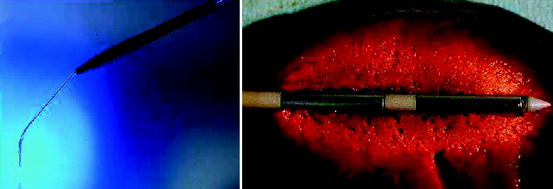
Fig. 7.1.2
(Left) Faceted radiofrequence probe Pro Sleep Plus with coat. (Right) Detailed view of the active electrodes
Fig. 7.1.3
(Left) Outline of the RFT of the tongue base. (Right) Intraoperative situation

Fig. 7.1.4
Correct area of treatment at the tongue base
7.1.2 Effectiveness for Simple Snoring
A recently published trial by Welt and coworkers has investigated the effect of isolated tongue base RFT in the treatment of simple snoring [808]. While in obstructive sleep apnea RFT of the tongue base does indeed improve snoring [720]; this trial has clearly shown that RFT of the tongue base alone is not an effective treatment of primary snoring – not even in patients where palatal snoring was excluded and tongue base hypertrophy was the only clinical finding [808]. In another trial the effects of RFT on the tongue base was also assessed in cases of primary snoring [144]. Nevertheless, in this trial the study group (n = 22) consists of only a subgroup patients with simple snoring (n = 9) and a larger subgroup with obstructive sleep apnea. The results with regard to snoring reduction are not given for the different groups but only for the entire (mixed) group of patients. Therefore, the specific effect in snoring patients cannot be assessed in this trial.
No data exist with regard to a combined approach, but based on recent data we cannot recommend isolated RFT of the tongue base in the treatment of simple snoring (Table 7.1.1).
Table 7.1.1
Effectiveness of RFT of the tongue base for treatment of simple snoring
Author | N | Device | Les/treat | Method | Snore pre | Snore post | Success (%) | ESS pre | ESS post | EBM |
|---|---|---|---|---|---|---|---|---|---|---|
Welt et al. [808] | 20 | Celon | 12 (7 W) | VAS | 7.5 | 6.1 | 15.0 (VAS <3) | 6.0 | 6.1 | 4 |
7.1.3 Effectiveness for OSA
A literature search in Pubmed (National Library of Medicine) was performed for the terms “radiofrequency,” “tongue,” and “sleep apnea.” Original studies published in English up to March 2008 were included if they addressed interstitial radiofrequency surgery of the tongue in patients with diagnosed obstructive sleep apnoea. In addition, a recent review was evaluated regarding potential additional publications [354]. For the analysis of clinical outcome, only studies using interstitial, transoral radiofrequency surgery as an isolated approach were analyzed. Studies using combined approaches in terms of multilevel surgery were only selected with regard to morbidity and complications. Data regarding a transcervical radiofrequency approach are limited to two pilot studies only with different techniques [54, 615]. In addition, it is regarded as a substantially different technique, so the data were not included in the analysis. One study was excluded due to the high number of dropouts and the inhomogeneous mixed patient sample (snoring and obstructive sleep apnea) [144]. The comparison of the cited studies is facilitated by the fact that all study groups but one worked with the same system. The total energy applied varies from 7,915 [575, 404] to 13,394 J [826]; yet no clear correlation between the energy applied and the surgery result can be deduced.
An analysis of the success rates given in Table 7.1.2 produces the following result: for altogether 118 patients (excluding the study of Li et al. [404], as the patient pool is partly identical with Powell et al. [575]) a surgical short-term success rate employing Sher’s criteria of 33.2% for RFT of the tongue base was achieved for (on average) moderate OSA. This seems to indicate that the efficacy of this technique is almost equal to invasive tongue base resections (Sect. 7.3). Nevertheless, in our opinion the data from Table 7.1.2 need to be cautiously interpreted. This is due to the fact that the study design of the RFT studies is a very different one. In all of the other procedures, a sleep lab evaluation is performed before and after surgery. But in the case of the RFT surgery which is based on subsequent treatment sessions, therapy continues until the polysomnography produces a satisfactory result. This is the issue at stake: the polysomnography exhibits a high night-to-night variance, which in this case only becomes evident in a positive manner for the surgical result [459, 462]. In other words: we doubt that the presented results would be corroborated by a therapy design delineated from the start by a defined number of sessions, lesions, and a defined amount of energy input. In addition to that, controlled studies are not available for tongue base RFT to date.
Table 7.1.2
Effectiveness of RFT of the tongue base for treatment of OSA
Author | N | Device | Follow-up | AHI pre | AHI post | ESS pre | ESS post | Success (%) | EBM |
|---|---|---|---|---|---|---|---|---|---|
Powell et al.a [575] | 15 | Somnus | 4.0 | 47.0 | 20.7 | 10.4 | 4.1 | 46.7 | 4 |
Woodson et al. [826] | 56 | Somnus | 1.5 | 40.5 | 32.8 | 11.1 | 7.4 | 20 | 2b |
Stuck et al. [720] | 18 | Somnus | 1.0 | 32.1 | 24.9 | 7.9 | 4.9 | 33 | 4 |
Li et al.a [404] | 16 | Somnus | 28.0 | 39.5 | 28.7 | 10.4 | 4,5 | No data | 4 |
Riley et al. [611] | 19 | Somnus | 3.0 | 35.1 | 15.1 | 12.4 | 7.3 | 63.2 | 4 |
den Herder et al. [144] | 9 | Celon | 12.0 | 12.9 | 10.6 | 5.1 | 4.4 | 30 | 4 |
All | 117 | 5.8 | 37.4 | 25.8 | 10.3 | 6.1 | 33.2 | C |
The best results are described by Riley and colleagues [611]. This study is distinguished from the other studies by the fact that besides two lesions at the tongue base it also applies a lesion on the anterior part of the tongue. Possibly this procedure contains a potential for an improvement of the objective results of RFT on the tongue base. Steward et al. performed an extended follow-up study [707] on a subgroup of patients published previously [708] and came to the conclusion that the improvements achieved with treatment remain stable over time (mean follow-up was 23 months).
A number of additional studies exist investigating the effects of RFT of the tongue base in the treatment of OSA. Nevertheless, these studies used this treatment as an adjunctive method together with, e.g., uvulopalatoplasty [212] or nasal surgery and palatal implants [214]. These studies basically document the feasibility of a combined approach; a reliable assessment of the specific effects of RFT of the tongue base cannot be performed with these studies. This is also true for those studies investigating the effects of combined RFT approaches at the tongue base and the soft palate [201, 708, 722]. Nevertheless, these data are specifically interesting, as a combination of the two RFT applications combines numerous advantages: the minimal invasiveness of both treatments and the fact that the application needles can often be used for both treatment sites without additional costs. The addition of a soft palate RFT, e.g., does not increase postoperative morbidity compared to tongue base RFT only. In this context, Steward et al. documented a significant symptomatic improvement of OSA after three RFT treatments at the tongue base with further improvement after additional two treatment sessions together with two soft palate treatments [706].
We are also of the basic opinion that the RFT therapy of the tongue base has been proven to have an effect in the treatment of OSA; but in terms of objective results it cannot compete primarily with the standard therapy CPAP. Yet the subjective results are absolutely equivalent with regard to daytime condition and quality of life [826]. Altogether, a careful reading of the raw data in the cited studies indicates that mainly mild forms of OSA are suitable for a therapy with RFT at the tongue base.
A series of trials has been published regarding combined radiofrequency surgery at the tongue base and the soft palate. This issue will be discussed in Chap. 10 multilevel surgery.
7.1.4 Postoperative Care and Complications
In the beginning of our RFTs at the base of tongue all patients were kept overnight for clinical monitoring after every treatment session. Over the last 100 treatments we have observed virtually no complications; therefore, this requirement can no longer be upheld as a general rule. Yet it is necessary to observe the patients until the sedation has sufficiently worn off. Due to the short half-life we solely use Midazolam. In our experience nothing is to be said against performing RFT at the tongue base on an outpatient basis.
The patient requires a perioperative and postoperative antibiotics prophylaxis [719]. We administer 2 g Cephazolin intraoperatively and 2 × 500 mg Cefuroxim per os postoperatively for 5 days. The administration of corticosteroids is not routinely necessary and we discourage its regular use.
In contrast to the application at the soft palate, postoperative pain is to be expected. In the case of our own patient pool, we have analyzed the level of pain with the help of a Visual Analogue Scale with the endpoints 0 = no pain and 10 = maximal pain [720]. The results, compared with the pain level after combined UPPP with tonsillectomy, are given in Fig. 7.1.5.
Fig. 7.1.5
Mean postoperative pain scores over 1 week after RFT of the tongue base
The patients require analgesics for approximately 4-5 days. We have achieved good results with retarded Dicflofenac (3 × 100 mg), if necessary in combination with also retarded Tramadol (2 × 200 mg). Nevertheless, an individualized pain management is necessary.
Apart from vasovagal reaction no intraoperative complications have been reported so far.
The postoperative complication rate is reported widely divergent, namely between 41 [551] and 0% [611]. But with its complication rate of 41%, the study by Pazos and Mair is an exception. All other studies report complication rates of below 5% [355, 720, 723, 724, 746]. We believe the most probable explanation for these divergent results lies in the perioperative management. In contrast to our own procedure, Pazos and Mair [551] recommend the general use of corticosteroids, whereas antibiotics were only administered in the case of inflammatory complications. The prophylactic administration of corticosteroids may predispose to infections. We therefore advise against their use.
A severe potential complication is the formation of an abscess of the tongue base, which has been reported by four study groups [551, 575, 724, 826]. We have taken our own case as an incentive to always perform a peri- and postoperative antibiotics prophylaxis. Since then, 6 years have passed, and we have not encountered a further abscess in over 1,000 treatments. A much more frequent complication is the occurrence of ulcerations at the tongue base (Fig. 7.1.6). They usually develop as a result of a too superficial positioning of the active electrode below the mucosa; in rare cases they are caused by a leak in the protective electrode sheath caused by excessive flexing of the electrode during treatment. These lesions at the tongue base cause a prolonged odynophagia of up to 3 weeks. Other complications are rare and consist in infection, edema, tongue pain well beyond 1 week, neuralgia up to 3 months, and thrush. A comparable safety profile has been documented for combined approaches with RFT at the tongue base and the soft palate [724]. Concerning functional parameters (swallowing, speech), no changes after RFT of the tongue base were observed in the majority of the trials [720, 723, 724, 826]. In a recent trial, high-energy single-session tongue base procedures were investigated by Nelson et al. [493]. The authors observed 2.8% superficial tongue ulcers and 1.7% persistent taste disturbances, but no serious complications. According to the statements made above regarding multiple and single treatment session, the authors came to the conclusion that high-energy single-session tongue base RFT is a safe procedure with low morbidity.


Fig. 7.1.6
Ulceration at the base of tongue after RFT treatment
For our own patient pool we have analyzed the complication of altogether 711 treatments of 477 patients with the Somnus system and the Celon system. All in all, the complication rate lay by 2.4%, with a slight advantage for the Somnus system. At the tongue base, one abscess, five ulcers, and seven prolonged odynophagia for maximally 3 weeks were registered. It is interesting to note that the complications diminish with an increase of treatment experience (Fig. 7.1.7) [724].
Fig. 7.1.7
Complication rate of RFT depending on the surgical experience
Apparently, a surgical learning effect exists. Today we have reached complication rates of below 1%. By observing the recommended perioperative management RFT surgery at the tongue base has established itself as a safe procedure with a low postoperative morbidity.
7.1.5 Indications and Contraindications
With RFT, for the first time, a minimally invasive and effective procedure for the tongue base is at our disposal. The postoperative morbidity and complication rate is strikingly low. Therefore, we regard RFT at the tongue base as a significant broadening of the surgical therapy spectrum. Accordingly high is the number of operations performed in our centers.
With regard to the most recent literature, RFT of the tongue base cannot be recommended in the treatment of primary snoring unless it is performed as combined procedures, e.g., together with RFT of the soft palate. From the data presented in Table 7.1.2 we infer an indication for RFT at the tongue base for mild OSA although a precise threshold cannot be given. In the case of more severe OSA, RFT at the tongue base is additionally an essential element of our multilevel surgical concept (see Chap. 10).
Contraindications are very limited. RFT of the tongue base should not be performed in patients with preexisting unilateral hyoglossal paralysis, although persistent paralysis of the hypoglossal nerve has not been documented in our centers.
Take Home Pearls
Radiofrequency surgery of the tongue base can successfully be applied in obstructive sleep apnea; as an isolated approach it is not recommended for primary snoring.
Radiofrequency surgery of the tongue base is associated with limited postoperative morbidity and low complication rates as long as an antibiotic prophylaxis is ensured.
The overall efficacy of the procedure is limited. When performed as an isolated approach, about one-third of well-selected patients may be treated successfully, although the underlying data are limited.
7.1.6 Hyoid Suspension
Nico de Vries and Thomas Verse
Core Features
In OSA, due to retrolingual obstruction, it is an option to employ hyoid suspension (HS) as isolated procedure, not combining it with other procedures.
Several modifications exist, with and without cutting of the strap muscles, with and without cutting of the tendon of the stylohyoid muscle, and with several forms of suture or steel wire.
Overall, the results of HS as isolated procedure in OSA with retrolingual obstruction are slightly above 50%, in small series and without long-term follow-up.
Success rates of HS in OSA due to retrolingual obstruction assessed by sleep endoscopy as only and as first procedure in a small series are above 70%.
Results of HS in OSA with retrolingual obstruction as salvage surgery in patients after UPPP failure are around 35%.
There is a trend to routinely combine HS with radiofrequency of the tongue base in OSA due to retrolingual obstruction.
HS is an integral part of multilevel surgery in severe OSA, CPAP failure, and multilevel obstruction.
Morbidity and complication rates of the procedure are acceptable.
7.1.7 Introduction: Hyoid Suspension Alone and As Part of Combined Treatment
While over the last 20 years gentle surgical procedures have been developed for the retropalatal obstruction site, much less techniques have been established for obstruction at retrolingual level. Series are small and long-term results are still lacking. Due to their invasive nature and their peri and postoperative morbidity, many of these procedures need to be critically evaluated.
As in all surgery, meticulous patient selection is crucial. In addition to polysomnography, topical diagnostic work-up is of paramount importance in this regard. We routinely perform sleep studies first. After this, in case surgery is considered, and in case of an AHI below 30, we schedule patients for sedated endoscopy (“sleep endoscopy”). In patients with an AHI >30, who refused nCPAP treatment upfront, or in patients who cannot accept nCPAP for whatever reason, sedated endoscopy is performed as well.
In case of retrolingual obstruction only, and simple snoring up to mild OSA (AHI <20), we either perform interstitial radiofrequency treatment of the tongue base (RFT TB) or we offer a mandibular advancement device if during sedated endoscopy the so-called chin lift (synonyms: mandible lift, chin thrust, Esmarch maneuvre) prevents tongue base collapse. Good candidates for a mandibular advancement device usually show a partial but not total tongue base collapse during sedated endoscopy.
In the period from March 2000 till June 2004 in case of retrolingual obstruction only, and moderate-to-severe OSA (AHI >20), we used to perform hyoidthyroidpexia (hyoid suspension, HS) as isolated procedure [145]. Usually in these patients the tongue base collapse during sedated endoscopy is more outspoken than in cases of mild OSA. Mandibular advancement devices have proven to be less effective in cases with a relatively higher AHI (moderate-to-severe OSA) and in cases that show total tongue base collapse and little effect of the chin lift within the sleep endoscopy.
Since 2005 till present, in case of retrolingual obstruction only, and moderate-to-severe OSA, we now more or less routinely combine hyoidthyroidpexia with RFT TB.
In case of combined retropalatal and retrolingual obstruction, moderate-to-severe OSA, we perform a form of multilevel surgery [600] (see Chap. 10). This, at our institute, is usually a combination of hyoidthyroidpexia, RFT TB, and UPPP with tonsillectomy. We have added genioglossal advancement (GA) to these three procedures in this period, but since we found that adding GA to the other three procedures did not lead to further improvement, we later abandoned this again.
7.1.8 Surgical Technique
7.1.8.1 Original Surgical Technique (1986), Historical Perspectives, and Nomenclature
The idea of preventing the collapse of the tongue musculature, which relaxes during sleep, toward dorsal into the upper airway with the help of a suspension of the hyoid bone is not new. Already at the beginning of the 1980s a widening of the upper airway after HS was demonstrated, first for the animal model [548, 762], and later for humans [348]. Initially it was attempted to fixate the hyoid on the chin.
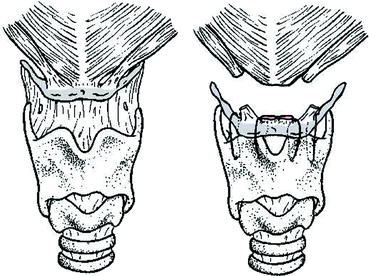
Based on the findings from radiocephalometric studies, that in sleep apneics the hyoid is positioned lower than in healthy subjects, in 1986 a new therapy concept was presented for the treatment of hypopharyngeal obstruction: the inferior sagittal osteotomy of the mandible with hyoid myotomy suspension [606]. The hyoid was moved upwards and forwards. This was achieved on the one hand with the help of a medial osteotomy at the chin with advancement of the origin of the M. genioglossus (see Sect. 8.1) and on the other hand with the help of a suspension of the hyoid at the chin with homologous fascia lata strands after myotomy of the intrahyoidal musculature (Fig. 7.2.1).
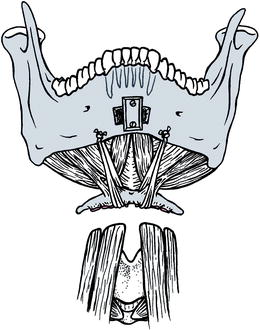
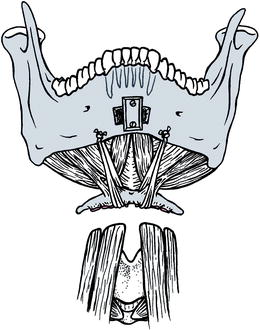
Fig. 7.2.1
Original technique of hyoid suspension (HS) with homologue fascia lata according to Riley et al. [606] here combined with genioglossus advancement
This original suspension technique of the hyoid to the chin with homologous fascia lata strands with myotomy of the intrahyoidal musculature has now more or less been abandoned by opinion leaders worldwide.
7.1.8.2 First Modification (1994)
Although this procedure was shown to be effective in improving OSA, it involved extensive surgical dissection of the submental region as well as the need of fascia lata harvest [413]. Other authors used, instead of the homologous fascia lata, other material, as for example nonresorbable suture material or special anchor systems [137, 368, 587, 641, 650]. In the meantime, the Stanford group modified its technique in reaction to these downsides. In this modification, originally presented by Riley and colleagues [608], the hyoid is no longer fixated on the mandible but on the upper edge of the thyroid cartilage. The resulting movement of the tongue base toward anterior and caudal increases and stiffens the upper airway.
Although in particular in the American literature the procedure is referred to as “Hyoid Suspension” this is in fact a misnomer and the correct term – albeit longer- is hyoidthyroidpexia. The reader has to make his own choice: the use of the short, easy term HS or the longer, more correct term hyoidthyroidpexia (HTP).
HTP involves stabilization of the hyoid bone inferiorly and anteriorly by attachment to the superior border of the thyroid cartilage. The underlying principle for altering the hyoid is that anatomically, the hyoid complex is an integral part of the hypopharynx. Anterior movement of the hyoid complex increases the posterior airway space (PAS) and neutralizes obstruction at the tongue base. In fact it is still not completely understood why it works. MRI studies have not shown an increase of PAS in wake, and possibly it is more a prevention of collapse during sleep only.
Under general anesthesia, with the head in slightly extended position, a horizontal incision of approximately 5 cm is made in a relaxed skin tension line at the level between hyoid and thyroid cartilage. Excessive fat tissue is excised, if useful for better visualization. Especially in case of a further posterior positioned hyoid, removal of fat is recommended as well, since otherwise the anterior placement of the hyoid will result in a somewhat turkey-like neck contour.
Secondly, the strap muscles are severed just below the attachment to the hyoid. Partial removal of the severed strap muscles at the level between hyoid and thyroid cartilage is sometimes also to be considered for the same cosmetic reasons while there is also little use to leave the nonfunctional cut strap muscles in situ.
The tendon of the stylohyoid muscle is cut only if after release of the strap muscles insufficient mobilization is gained. Otherwise the stylohyoid tendon is preserved. Gradually we ourselves have almost completely stopped cutting the stylohyoid tendon, as we feel that almost always the cutting of the strap muscles provides sufficient mobility.
By mobilizing the hyoid bone in an anterocaudal direction and fixing it to the thyroid with two permanent sutures per side (we use Mercilene 0) through the thyroid cartilage and around the hyoid bone, more space is created retrolingually. Although with increasing age ossification of the thyroid will take place, in more than 100 cases we have never needed to make drill holes. A sharp cutting needle has so far always been sufficient to pierce the thyroid cartilage.
Antibiotics are not routinely applied, in case HTP is the only procedure, but will be applied in case the procedure is combined with RFT TB. A surgical drain is placed and usually removed after 24-48 h postoperatively if drainage is less than 10 mL per 24 h. Nocturnal oximetry is monitored throughout the first postoperative night in the intensive care unit and nonopioid analgesics are used for pain relief, if necessary (Fig. 7.2.2).
Usually intubation anesthesia is used. The procedure can also be performed under local anesthesia [500], but then intravenous sedation with Midazolam of Propofol is recommended.
7.1.8.3 Hörmann’s Modification (2001)
In Mannheim, Hörmann and coworkers have modified the method rigorously [292, 294]. In order to be less invasive, the group does not cut the ligamenta stylohyoidea or the supra- and infrahyoidal musculature at all. Usually intubation anesthesia is used. The procedure can also be performed under local anesthesia [500], but then intravenous sedation with Midazolam of Propofol is recommended. The patient receives an intraoperative single shot with 2 g Cefazolin.
The patient is placed on the operating table with slightly reclined head. Initially it may be helpful to mark the position of the hyoid and the upper edge of the larynx. For cosmetic reasons, the skin incision is performed above the hyoid bone along the relaxed skin tension lines (Fig. 7.2.3).
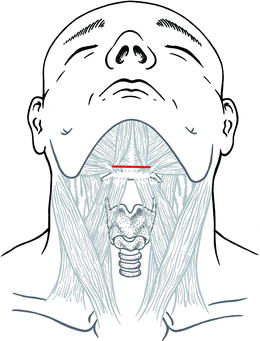
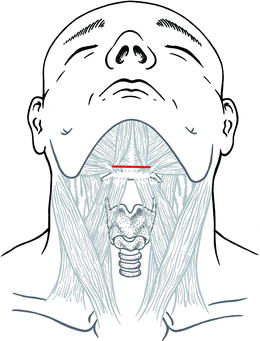
Fig. 7.2.3
Hörmann’s technique of HS. Dermal incision
One proceeds through the submental fat up to the floor of mouth musculature. Without damaging it, the muscles are sectioned down to the hyoid; then the thyroid cartilage is exposed. It is useful if the assistant or nurse pushes the larynx toward cranial with two fingers. For aesthetic reasons it is important to remove a sufficient amount of fat tissue (Fig. 7.2.4). Failure to do so will, as a result of the advancement of the hyoid, create an unattractive supralaryngeal wrinkle as a turkey-like appearance.
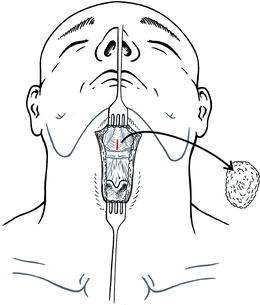
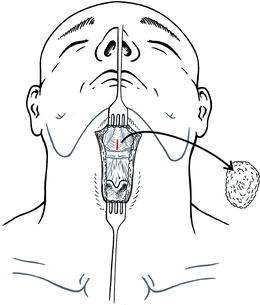
Fig. 7.2.4
Hörmann’s technique of HS. Exposure of the hyoid bone and thyroid cartilage. Resection of redundant fat
In contrast to the “standard method,” Hörmann’s modification needs only one triangular suture, which passes on both sides paramedial through the thyroid cartilage and medial around the hyoid. As suture, a monofilamentous grade 3 steel wire (Ethicon, Hamburg, Germany) is used. For this, first the suprahyoidal musculature is vertically separated precisely in median, until a Langenbeck retractor can be applied (Fig. 7.2.4, red line). The fascia in the midline between each sternohyoid muscle is incised with electrocautery until the plane of the thyroid cartilage is reached. The blood supply to the thyroid cartilage is provided by the blood vessels of the perichondrium. Unnecessary elevation of the perichondrium should, therefore, be avoided to reduce the risk of necrosis. The muscles on both sides are retracted to expose the lateral parts of the thyroid cartilage. Now, starting at caudal, a sharp needle is pierced through the cartilage without drilling. The steel wire is fixed at the end of the needle, which comes out on the contralateral side of the thyroid cartilage (Fig. 7.2.5, left side). Then the hyoid body is encircled with the wire ligature until the tip of the needle appears on the Langenbeck retractor (Fig. 7.2.5, center). In order to prevent accidental opening up of the laryngeal tube by the wire, the assistant elevates the hyoid with a Joseph retractor. In order to prevent tearing of the suture, the distance to the upper edge of the thyroid cartilage should be at least 5 mm. Especially in older men, ossification of the thyroid cartilage may make piercing of it with the ligature difficult, respectively impossible. A surgical drill system as used in ear surgery is of help here.
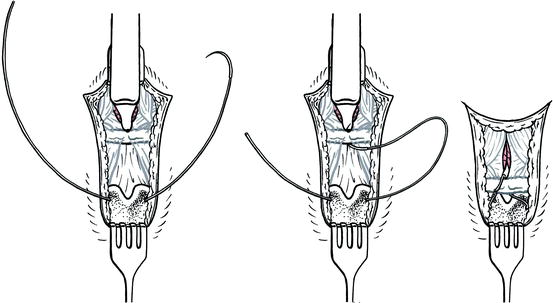
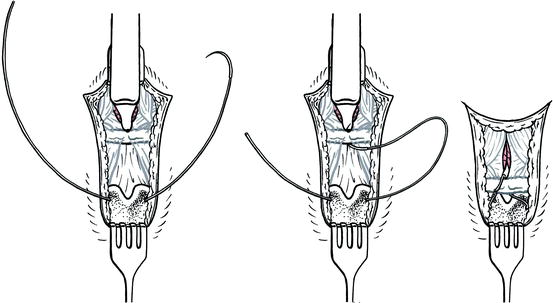
Fig. 7.2.5
Hörmann’s technique of HS. (Left) Transfixing the thyroid cartilage with the steel wire suspension. (Center) Undermining the hyoid bone. (Right) Completion of suspension
Now the actual suspension takes place (Fig. 7.2.5, right side). One more time the hyoid is undergirded with the Joseph retractor. With one hand the assistant pulls the hyoid with this retractor toward anterior and caudal, while pushing the larynx with the other hand toward cranial. The surgeon now fixates the hyoid in this position on the larynx with the ligature by intertwining the two wire ends. In order to achieve an optimal result, it is important not to make a kink in the wire ligature, as otherwise it cannot be tightened. Finally the wire ends are twisted inwards in order to prevent painful piercing of the skin. A Redon drainage with suction is applied, and the wound is closed in layers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree