Malformations and Syndromes |
Genes, Loci |
|---|
Hemimegalencephaly (HMEG) |
• |
HMEG, isolated |
None known |
• |
Epidermal nevus syndrome (9,10) |
None known |
• |
Hypomelanosis of Ito (11) |
None known |
• |
Klippel-Trenaunay syndrome |
None known |
• |
Neuromelanosis (12) |
None known |
• |
Proteus syndrome (13) |
None known |
Tuberous sclerosis (14, 15, 16, 17) |
TSC1, TSC2 |
Focal cortical dysplasia (FCD) with balloon cells (18, 19, 20) |
None known |
Focal transmantle dysplasia |
None known |
Megalencephaly (MEG) |
• |
MEG, isolated (21) |
None known |
• |
Macrocephaly-CMTC syndrome (22,23) |
None known |
• |
MEG with mega-corpus callosum (24) |
None known |
• |
MEG-PMG-polydactyly-hydrocephalus (unpublished data) (200) |
None known |
Microcephaly (MIC), moderate phenotype |
• |
MIC group 1 (25, 26, 27, 28, 29, 30, 31, 32, 33, 34) |
ASPM, MCPH1, 9q34, 15q, 19q13 |
MIC, severe phenotype |
• |
Amish lethal MIC (35,36) |
SLC25A19 |
• |
MIC with heterotopia (37,38) |
ARFGEF2 |
• |
MIC group 2, other types (39, 40, 41, 42) |
None known |
• |
Seckel syndrome (43) |
ATR |
Microlissencephaly (MLIS) |
• |
MLIS group a, a=p (44, 45, 46) |
None known |
• |
Barth MLIS syndrome (group b), a=p (45,47,48) |
None known |
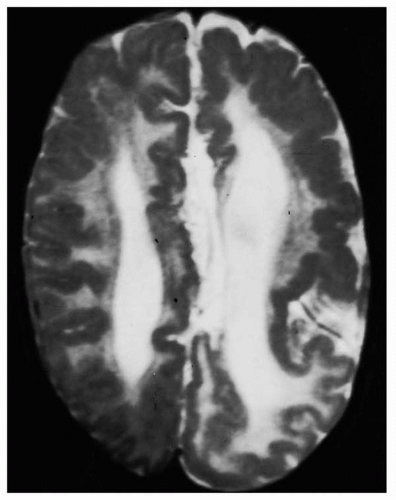
Periventricular nodular heterotopia (PNH) |
• |
X-linked PNH (females) (49, 50, 51) |
FLN1 |
• |
PNH with agenesis corpus callosum (males) (52,53) |
None known |
• |
PNH with Ehlers-Danlos syndrome (females) (54,55) |
None known |
• |
PNH with frontonasal malformation (males) (56,57) |
None known |
• |
PNH with mental retardation (males) (58,59) |
None known |
• |
PNH with nephrosis (males) (60) |
None known |
• |
PNH with short gut syndrome (males) (2,61) |
Xq28 (?) |
• |
PNH with frontoperisylvian PMG (unpublished data) |
None known |
• |
PNH with posterior-inferior PMG (unpublished data) |
None known |
• |
PNH with mental retardation and duplication 5p (62) |
5p15.1, 5p15.33 |
Heterotopia, other types |
• |
Periventricular laminar heterotopia (unpublished data) |
None known |
• |
Subcortical nodular heterotopia (63) |
None known |
Classic lissencephaly |
• |
Baraitser-Winter syndrome, a>p (64, 65, 66, 67) |
None known |
• |
Miller-Dieker syndrome a=p (44,68,69) |
LIS1, 14-3-3ε |
• |
Isolated LIS sequence, a=p, a>p (70,71) |
DCX |
• |
Isolated LIS sequence, a=p, p>a (70, 71, 72, 73, 74, 75) |
LIS1 |
• |
Subcortical band heterotopia a=p, a>p (76, 77, 78, 79, 80) |
DCX |
• |
Subcortical band heterotopia, p>a (66,68,70,71,79) |
LIS1 |
LIS with cerebellar hypoplasia (LCH) |
• |
LCH group a, a=p, a>p, p>a (81) |
LIS1, DCX |
• |
LCH group b, a>p (81, 82, 83) |
RELN |
• |
LCH group d, a=p (81) |
None known |
LIS with agenesis of the corpus callosum (ACC) |
• |
X-linked LIS with abnormal genitalia (XLAG), p>a (84, 85, 86) |
ARX |
• |
LIS with ACC, other types, a=p (87, unpublished data) |
None known |
Cobblestone malformations |
• |
Fukuyama congenital muscular dystrophy (88, 89, 90, 91) |
FCMD |
• |
Muscle-eye-brain disease, a>p (92, 93, 94, 95, 96) |
POMGnT1, FKRP, LARGE |
• |
Walker-Warburg syndrome, a=p (97, 98, 99) |
POMT1, FCMD |
Excessive neurons in white matter (100,101) |
None known |
Polymicrogyria (PMG), regional |
• |
Frontal PMG (102) |
None known |
• |
Frontoparietal PMG (103, 104, 105) |
GPR56 |
• |
Parasagittal PMG (unpublished data) |
None known |
• |
Perisylvian PMG (106, 107, 108, 109, 110, 111, 112, 113) |
1p36, 1q44, 22q11, Xq28 |
• |
Medial parietooccipital PMG (114) |
None known |
• |
Generalized PMG (115) |
None known |
Polymicrogyria (PMG), others |
• |
PMG with abnormal white matter (unpublished data) |
None known |
• |
Schizencephaly (116) |
None known |
• |
Septooptic dysplasia-schizencephaly (117, 118, 119) |
None known |
FCD and related |
• |
FCD without balloon cells (20) |
None known |
• |
Microdysgenesis (4) |
None known |
a=p, Anterior equals posterior gradient; a>p, anterior more severe than posterior gradient; p>a, posterior more severe than anterior gradient; CMTC, cutis marmorata telangiectatica congenita. |
|