and Thomas Hierl2
(1)
Department of Otorhinolaryngology Head and Neck Surgery, Asklepios Clinic Harburg, Eissendorfer Pferdeweg 52, 21075 Hamburg, Germany
(2)
Department of Oral and Maxillofacial Plastic Surgery, University of Leipzig, Leipzig, Germany
Abstract
The genioglossus advancement (GA) is used in combination with other surgical techniques for treatment of severe OSA. The surgical principle consists in mobilizing the whole area of this muscle insertion by incorporating the genial tubercle on the inner cortex via an osteotomy of the chin, and then moving it toward anterior. An isolated efficiency verification according to the principles of evidence-based medicine (EBM) is not available. In a meta-analysis of 80 patients who received a combination of GA and adjunctive procedures (e.g., hyoidsuspension), a success rate of 66% was reported.
8.1 Genioglossus Advancement (GA)
Core Features
The genioglossus advancement (GA) is used in combination with other surgical techniques for treatment of severe OSA. The surgical principle consists in mobilizing the whole area of this muscle insertion by incorporating the genial tubercle on the inner cortex via an osteotomy of the chin, and then moving it toward anterior.
An isolated efficiency verification according to the principles of evidence-based medicine (EBM) is not available. In a meta-analysis of 80 patients who received a combination of GA and adjunctive procedures (e.g., hyoidsuspension), a success rate of 66% was reported.
In 1986, the inferior sagittal osteotomy of the mandible was used for the first time in the treatment of obstructive sleep apnea (OSA) by the Stanford research group [604]. The authors used this technique in combination with a hyoid suspension (HS) (Sect. 7.2 in Chap. 7) in patients with severe OSA. Since then the so-called mandibular osteotomy with genioglossus advancement (MO) has become part of several surgical protocols. Interestingly, the technique has until now only been used in combination with other techniques and not as an isolated procedure for treating OSA.
8.1.1 Surgical Technique
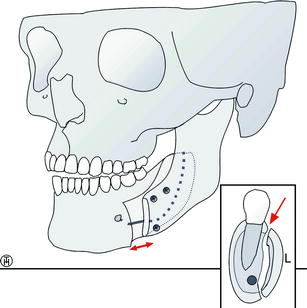
The genioglossus muscle has its origin at the oral side of the mandible. The surgical principle consists in mobilizing the whole area of this muscle insertion by incorporating the genial tubercle on the inner cortex via an osteotomy of the chin, and then moving it toward anterior (Fig. 8.1.1). In this new position, the bone segment is fixated osteosynthetically, either with a 24-gauge stainless steel wire or a screw. External cortex and cancellous bone are removed in order to prevent a cosmetically disagreeable protrusion of the chin.
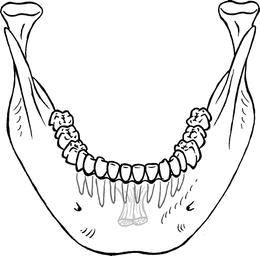
Fig. 8.1.1
Origin of the genioglossus muscle at the genial tubercle on the inner cortex of the mandible
The surgical approach is completely intraoral. The mucosal incision is made approximately 10-15 mm below the mucogingival junction and a subperiostal flap is developed to expose the symphysis. Exposure and identification of the mental nerves are unnecessary. In order to reduce the extent of the dissection, entailing a reduction of potential complications, Riley et al. have twice revised their technique of inferior sagittal osteotomy. Figure 8.1.2 shows the most recent technique [410] which we have adopted in our center. Miller et al. [467] recently recommended the use of the Genial Bone Advancement Trephine system (Stryker leibinger Corp.; Kalamazoo) and reported good results.
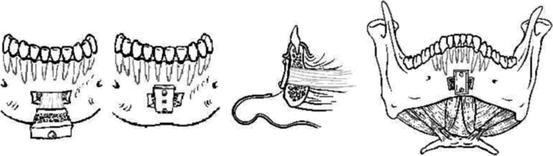
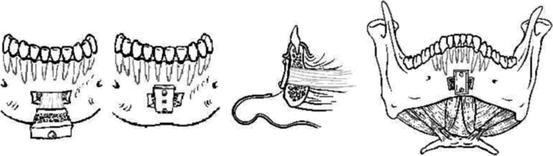
Fig. 8.1.2
Inferior sagittal osteotomy of the mandible. Left: bony segment pulled forward after rectangular osteotomy. Center and right: postoperative situation
A rectangular osteotomy encompassing the estimated location of the genial tubercle/genioglossus muscle complex is performed under copious irrigation. The superior horizontal bone is cut approximately 5 mm below the root apices to prevent incisor root injury and the inferior horizontal bone is cut approximately 10 mm above the inferior border (Fig. 8.1.2). Occasionally, the superior horizontal bone cut has to be made 1-2 mm above the incisor root apices because of the vertical position of the genial tubercle/genioglossus muscle complex [469]. Due to the elongated canine tooth roots that are often present, the vertical bone cuts are made just medial to the canine roots to avoid root injury. Before completing the osteotomy, a titanium screw is placed in the outer cortex to control and manipulate the bone flap. The amount of advancement depends on the thickness of the mandible. The bone flap is advanced and rotated about 30-45°, just sufficient to create bone overlap for a fixation screw.
Li et al. [410] control bleeding with electrocautery and a hemostatic agent such as Gelfoam R (Pharmacia and Upjohn Co, Kalamazoo). Bone wax is not recommended due to extrusion problems. These authors do not use surgical drains. In their hands, the procedure is routinely completed within 30-40 min.
In treating the hypopharyngeal site of obstruction, most authors combine the GA with a HS [499, 587, 608]. Fibbi et al. [196] recommend the combination of GA with a tongue suspension suture (ReposeR) (Sect. 7.4 in Chap. 7). Furthermore, the GA is part of some multilevel surgery protocols as discussed in Chap. 10.
8.1.1.1 Effectiveness for OSA
The GA is a therapy for OSA, but not for primary snoring. As mentioned above we have not been able to find any studies using polysomnographies in investigating the effectiveness of GA as an isolated procedure. Therefore, we have decided to summarize in Table 8.1.1 only the current data of studies performing combined procedures for tongue base obstruction.
Table 8.1.1
Effectiveness of GA for OSA
Author | N | Adjunctive procedure | Follow-up (months) | AHI pre | AHI post | Success rate (%) | EBM |
|---|---|---|---|---|---|---|---|
Riley et al. [606] | 5 | HS | 6 | 73.6 | 21 | 80 | 4 |
Riley et al. [605] | 55 | HS, UPPP | 6 | 58.7 | 11.8 | 66.7 | 4 |
Riley et al. [608] | 15 | HS | 3 | 44.7 | 12.8 | 53.3 | 3b |
Johnson and Chinn [334] | 9 | UPPP | 39 | 58.7 | 14.5 | 77.8 | 3b |
Ramirez and Loube [587] | 12 | HS, UPPP | 6 | 49 | 23 | 42 | 3b |
Lee et al. [390] | 33 | UPPP | 4-6 | 55.2 | 21.7 | 66.7 | 4 |
Fibbi et al. [196] | 4 | TBS | 6 | 22.0 | No data | 75.0 | 4 |
Neruntarat [499] | 46 | HS, Flap | 39.4 | 47.9 | 18.6 | 65.2 | 4 |
Miller et al. [467] | 24 | UPPP | 4.7 | 52.9 | 15.9 | 66.7 | 4 |
Foltan et al. [205] | 31 | HM | 7.3 | 20.9 | 10.3 | 74.0 | 3b |
All | 234 | 48.78 | 15.51 | 66.10 | B |
Since most of these are noncontrolled data, and since all but two of them are also short-term data, a verification of the effectiveness according to the principles of evidence-based medicine (EBM) is still difficult. In addition, all authors performed additional procedures. This is why the effect of an isolated GA remains unclear.
In this context, the study by Neruntarat [499], who compares short- and long-term results, is of interest. All patients had received an uvulopalatal flap, an HS, and a GA in the framework of a multilevel surgery concept. In his retrospective analysis of 46 patients, a therapy success (Sher’s criteria) of 78.3% after 6 months and of 65.2% after on average 39 months was found. Obviously this points to a decrease of the therapy effect over time. Unfortunately, it cannot be deduced which partial effect can be ascribed to the GA.
8.1.2 Postoperative Care and Complications
The GA is performed under general anesthesia on an inpatient basis. In cases where no further procedures involving the upper airway have been performed, a hospital stay of about 2 or 3 days is sufficient. We administer an intraoperative single-shot antibiosis with, e.g., 1 × 2 g cephazoline. The administration of corticoids is not necessary.
As GA is a used in severe OSA, some authors generally protect the upper airway with the routine use of nasal continuous positive airway pressure (CPAP) during the postoperative phase. We observe our patients in the recovery room for some hours and apply CPAP only in cases that show repeated apneas. If a CPAP therapy is necessary, the auto-CPAP mode is used. Observation in an intensive care unit is usually not necessary after MO.
As minor complication a wound dehiscence has been observed intraorally. It usually heals spontaneously without sequela. Furthermore, transient numbness of the lower lip and lower central incisors for several weeks [467], dysphagia for up to 1 week, and self-limiting aspiration have been reported [499]. In general, tooth root injuries, mental nerve injuries, and mandibular fracture as potential complications have been reported only very rarely [410]. In our own group of patients one subject developed a severe wound infection several days after surgery requiring surgical intervention. Similar cases have been reported by other authors as well [395, 605]. Speech or swallowing problems have neither been reported nor have they been seen in our own patients.
8.1.3 Indications and Contraindications
Like HS, GA is an invasive surgical method with potential complications. For the tongue base, a minimally invasive alternative exists in the form of radiofrequency treatment (RFT). We therefore see no primary indication for the HS for primary snoring, and mild OSA.
In the case of moderate and severe sleep apnea with tongue base obstruction, the GA is a surgical treatment option. In our center, we have completely ceased to perform this technique as we encountered several complications. We have had better experiences with HS. The latter can be performed more rapidly, is the only procedure which can be performed under local anesthesia, uses less osteosynthesis material, and is at least in our hands less prone to complications. Nevertheless, in the hands of an experienced surgeon GA may be a viable alternative in the treatment of moderate to severe OSA.
Take-Home Pearls
The GA is used in combination with other surgical techniques for treatment of moderate and severe OSA. In our center we do not perform it anymore. Treatment options like hyoid suspension or laser-assisted excision of the tonsillar tissue at the tongue base are preferred.
8.2 Maxillomandibular Advancement (MMA)
Thomas Hierl
Core Features
Maxillomandibular advancement (MMA) in severe sleep apneics is done as a secondary procedure after failure of a conservative (continuous positive airway pressure, CPAP) or multilevel surgery therapy. A simultaneous expansion of the naso, oro-, and hypopharyngeal airways is achieved.
MMA is an invasive surgical technique with corresponding morbidity and complication rates.
In high-selected patient groups, studies report a short-term success rate of 97% after 6 months and a success rate of 90% after 51 months.
Complications after MMA are temporomandibular joint dysfunction, hypopharyngeal edema, velopharyngeal incompetence, and hypesthesia of the lower lip.
Maxillofacial surgery for the correction of malpostion of the upper and lower jaw was first suggested by Kuo et al. [378] as an alternative to tracheotomy in the treatment of obstructive sleep apnea (OSA). Today, MMA can be seen as the most successful surgical procedure after tracheotomy. On the other side, it must be said that it is an invasive surgical technique with corresponding morbidity and complication rates. Therefore, it is used as primary therapy in patients with relevant deformities of the face and the skull in most instances. For sleep apneics without a jaw anomaly, the Stanford 2 phase concept has become the standard treatment. In phase 1, it offers a multilevel surgery of the soft palate and tongue base, and if necessary of the nose in accordance with the procedures provided in Chap. 10; only in the case of therapy failure does it offer MMA as a secondary procedure.
The rationale of MMA is the simultaneous expansion of the naso-, oro-, and hypopharyngeal airways as soft palate, tongue, and lateral pharyngeal walls are advanced or stretched (Fig. 8.2.1).
Fig. 8.2.1
Left: preoperative situation. Retropositioned maxilla and mandible with narrow pharyngeal airway space. Right: after MMA the widened pharynx, an anterior positioned tongue and soft palate can be seen. SNA° and SNB° which determine the sagittal position increase
8.2.1 Surgical Technique
Although MMA is a routine procedure in maxillofacial surgery, it is technically demanding and performed by a team of surgeons in a hospital environment under general anesthesia [581].
8.2.1.1 Surgery on the Upper Jaw
In order to advance the upper jaw it has to be freed from the upper parts of the midface and the cranial base, moved forward (and if necessary simultaneously up- respectively downward), and stabilized in the new position. The usual method consists in a transverse osteotomy of the maxilla (so-called Le Fort I osteotomy) [518]. The osteotomy lines (Fig. 8.2.2) resemble more or less the fracture lines analogous to the Le Fort I fracture.
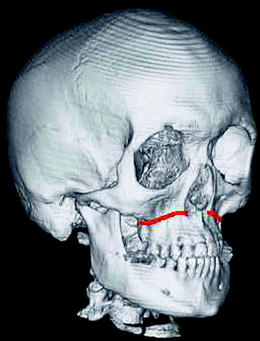
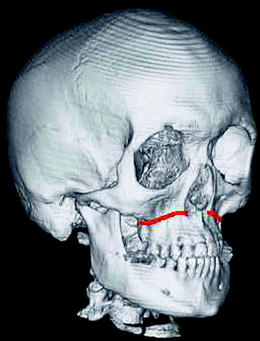
Fig. 8.2.2
Le Fort I osteotomy (red line). The nasal septum and the pterygomaxillary junction are detached with a chisel; the paranasal and zygomatic buttresses are cut with a reciprocating saw
While in 1970s-1980s, wire osteosyntheses, zygomatico-maxillary suspensions, and intermaxillary fixation (for approximately 6 weeks) were used, now miniplate osteosynthesis has become the standard procedure to hold the maxilla in its new position until bony union has occurred (Fig. 8.2.3). The extent of the maxillary advancement is determined individually depending on the amount judged necessary for relief of OSA, the new position of the mandible and the nutrition status during operation as excessive soft tissue stretching in the soft palate region may compromise vascularity. In most studies, 10 mm are suggested as some relapse (backward movement of the maxilla) has to be expected.
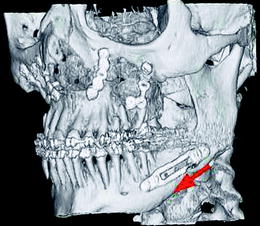
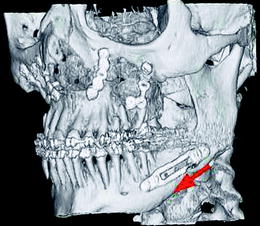
Fig. 8.2.3
Osteosynthesis technique using titanium miniplates in orthognathic surgery. Maxillary advancement in the Le Fort-I level stabilized by way of four miniplates on the paranasal and zygomatic buttresses. Simultaneous mandibular advancement (see red arrow) utilizing adjustable split-fix miniplates (all Synthes®, Paoli, PA)
In case of stabilization with miniplates, intermaxillary fixation is not necessary in most instances; this is especially of relevance in the immediate postoperative phase in OSA patients. Furthermore, the amount of relapse will be minimized.
8.2.1.2 Surgery on the Lower Jaw
In principle, the advancement of the lower jaw can be performed almost anywhere in the mandible ranging from an osteotomy in the mandibular body to the ascending ramus [574, 604]. The most common method is the bilateral sagittal split osteotomy (BSSO) according to Obwegeser [519] with lateral corticotomy anterior to the mandibular angle [603, 604] (Fig. 8.2.4).
In this procedure, the lingual bone separation proceeds horizontally between lingula and incisura semilunaris. The osteotomy line on the buccal side proceeds vertically from the molar region to the inferior border. The sagittal split is then performed using a chisel (Fig. 8.2.4). It is crucial to take care that the inferior alveolar nerve remains lingual of the chisel in order to prevent lesions. After aligning the mandible to a correct occlusion, osteosynthesis is performed. Here wire sutures, or preferably position screws or miniplates can be used (Fig. 8.2.4).
In all cases of MMA surgery, some skeletal relapse has to be accepted. Factors determining the amount of relapse include osteosynthesis technique and the amount of advancement. In the maxilla and mandible 10-30% can be reckoned with. Thus in a 10 mm advancement a net forward movement of 7-9 mm will persist which is judged sufficient for OSA relief.
8.2.2 Efficiency of Maxillomandibular Advancement for OSA
MMA can be considered the most successful surgical procedure for the treatment of OSA after tracheotomy with respect to treatment outcome. Several controlled studies have demonstrated a comparable reduction of the Apnea Hypopnea Index (AHI) after MMA to continuous positive airway pressure (CPAP) therapy [284, 582, 607] (Table 8.2.1). Furthermore, an equivalent optimization of the sleep architecture compared to CPAP has been reported after MMA [123].
Table 8.2.1
Multilevel surgery for OSA
Author | N | Adjunctive procedure | Follow-up (months) | AHI pre | AHI post | Success rate (%) | EBM |
|---|---|---|---|---|---|---|---|
Waite et al. [788] | 23 | UPPP, GA, MLP | 1.5 | 62.8 | 15.2 | 65.2 | 4 |
Riley et al. [607] | 30 | HS | 6 | 72.0 | 8.8 | 96.7 | 3b |
Hochban et al. [284] | 38 | 2 | 44.4 | 2.5 | 97.4 | 3b | |
Prinsell [582] | 50 | HS | 5.2 | 59.2 | 4.7 | 100 | 3b |
Li et al. [405] | 40 | 50.7 | 69.6 | 8.9 | 90 | 4 | |
Bettega et al. [51] | 20 | Prior phase I | 6 | 59.3 | 11.1 | 75 | 4 |
Goh and Lim [234] | 11 | 7.7 | 70.7 | 11.4 | 81.8 | 4 | |
Dattilo and Drooger [136] | 15 | Prior phase I | 1.5 | 76.2 | 12.6 | 86.7 | 4 |
All | 227 | 12.4 | 62.3 | 8.1 | 89.9 | B |
The successful results seem to be maintained for long follow-up periods. The Stanford studies report a short-term success rate of 97% after 6 months [607], and a success rate of 90% after 51 months [405].
Furthermore, Li et al. [402] were able to show by way of radiocephalometry and nasopharyngoscopic examinations that pharyngeal depth increased by 48% of the amount of the maxillary advancement and that pharyngeal length increased by 53% of the maxillary advancement in 5 patients after MMA.
8.2.3 Postoperative Care and Complications
For patients suffering from severe OSA, it is recommended to start nasal CPAP at least 1 month before surgery to stabilize the cardiovascular system and reduce upper airway edema [51].
After surgery, extubation should be performed by the operating room staff with the patient being fully awake. MMA patients require careful monitoring, including continuous pulse oximetry, in an ICU environment [581]. Minor desaturations do not call for a CPAP therapy; yet frequent desaturations or apneas require CPAP ventilation therapy. When feasible, nonopioid drugs are used for postoperative analgesia (see Chap. 13).
Nutritional counseling emphasizing clear liquids during the first week, followed by a soft diet for 2 months, is recommended. Today, most authors do not favor prolonged intermaxillary fixation and use modern titanium plate systems for osteosynthesis. The usual hospital stay for MMA lies between 2 days [581, 607] and 1 week [51]. On average, patients return to their normal activities after 2-4 weeks. Patients should be asked to continue nasal CPAP until a follow-up polysomnography has confirmed the surgical success. Nasal decongestants should be administered for the first postoperative week as maxillary osteotomies lead to tearing of the nasal mucosa and edema with impaired nasal respiration.
Temporomandibular joint dysfunction is a potential complication after maxillomandibular surgery. Kerstens et al. [353] reported that 11.5% of the 480 patients who underwent surgery for dentofacial deformity developed temporomandibular joint symptoms after surgery. Similar data were given by White and Dolwick [814] (7.9%). However, temporomandibular joint problems can be often found in patients suffering from dentofacial deformities and the vast majority of the patients presenting preoperative temporomandibular joint symptoms reported improvement after surgery [409]. Here two patient groups have to be distinguished: firstly, patients with normal occlusion who undergo MMA for OSA treatment only and secondly, patients with marked maxillary/mandibular retrusion where MMA is intended for relief of OSA and to improve occlusal relationship.
Further complications are temporary mild-to-moderate hypopharyngeal edema (20%) and hypopharyngeal hematoma (5.7%), partly obstructing the airway [411]. In large maxillary advancements patients frequently develop velopharyngeal incompetence of a temporary nature. Predominantly velopharyngeal incompetence is a phonetic deficit without liquid regurgitation. But there are also singular prolonged cases of velopharyngeal incompetence with regurgitation up to a duration of maximally 12 months [412].
Hypesthesia of the lower lip is the typical complication of BSSO (anesthesia <1%; hypesthesia <5%) [51, 607]. A high percentage of resolution within the first months after surgery is reported. Recovery of full mandibular function (maximum mouth opening; bite force) will take some time and will not be gained in all instances. A further frequent complication is occlusion disturbances in up to 50% of the cases, requiring minor occlusial equilibration by way of orthodontics or prosthodontics [788].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree