Chapter 3 Medications used for disturbances of cognition and perception
The information in this chapter will assist you to:
5-HT2 receptors serotonin receptors
D1–5 receptors dopamine receptor types1–5
EPSE extra-pyramidal side effect
NMDA receptor N-methyl-Daspartate receptor
Introduction
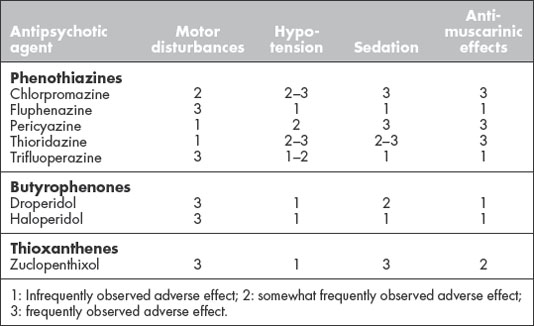
Normal cognition and perception are dependent on interplay between the cortical areas and other brain regions including the thalamus, amygdala, hypothalamus, brain stem and corpus striatum. The roles of each brain region involved are summarised in Figure 3.1. Major disturbances of cognition and perception in a mental health context include dementia, delirium, psychosis and attention deficit/hyperactivity disorders. In this chapter, we focus on dementia and psychosis. Attention deficit/hyperactivity is discussed in Chapter 7.
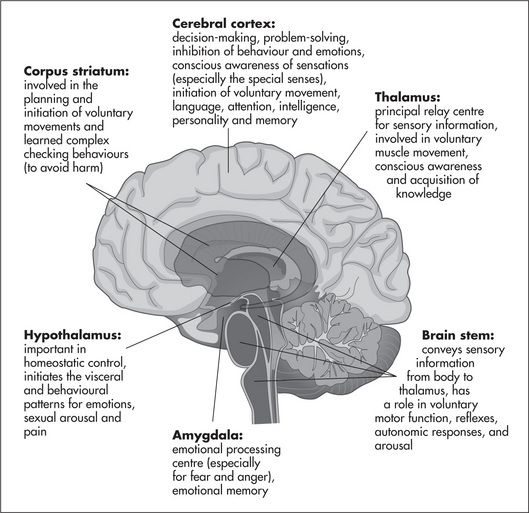
Figure. 3.1 Roles of selected brain regions in cognition and perception.
Adapted from Human Anatomy and Physiology (7th edn), 2007, by E N Marieb and K Hoehn, Pearson-Benjamin Cummings, Fig 12.12, p 445, with permission.
Disturbances in cognition and perception occur as a result of poor or inappropriate interplay between these key brain regions and are associated with a combination of genetic and environmental factors. The environmental factors include systemic metabolic disruptions, brain infections, substance misuse, changes in nerve membrane thresholds, the formation of scar tissue in the brain, as well as the degeneration or remodelling of nerve pathways.
Section 1: Medications used to manage schizophrenia and psychosis
Overview of psychosis
Psychosis can be associated with a number of disorders and produces symptoms that lead to the person’s loss of contact with reality. In psychosis, the perceptual disturbance of hallucinations, along with disorganised thought processes and/or the thought disturbance of delusions, can lead to bizarre or unusual behaviours. In fact, it is often these that signal to others that the person may be experiencing an alteration in their mental health. As indicated by their name, antipsychotic medications are used to manage and treat the symptoms of psychotic mental disorders.
Antipsychotic medications are used primarily for the psychotic disorders schizophrenia and schizoaffective disorder. They are used to a lesser extent in bipolar disorder and major depression, but are also used to treat a wide variety of disorders including those from primarily physical causes such as delirium and substance-induced psychosis. See Box 3.1 for an overview of the types of mental health problems where psychosis is a major feature. Other uses for antipsychotics include sedation and management of agitation and aggression, reduction of anxiety and as antiemetics (some older/first generation agents such as chlorpromazine and trifluoperazine).
Schizophrenia
The term schizophrenia refers to a group of psychotic disorders characterised by disordered and disorganised thought. Schizophrenia affects a person’s perceptions, speech, emotions and behaviours and can be associated with significant difficulty in psychosocial and occupational functioning. The course of the disorder can vary, but is generally chronic with acute exacerbations of varying intensity and frequency, some of which may necessitate hospitalisation. Schizophrenia is observed in 1% of the population across all cultures and affects men and women equally. Treatment and management of schizophrenia focus on reducing symptoms, preventing relapse, enhancing recovery and maintaining remission of symptoms over the long term (Burton 2006). The clinical manifestations of schizophrenia are listed in Table 3.1.
Table 3.1 The common clinical features of schizophrenia
| Positive symptoms – the presence of unusual symptoms not present in others in the population (most common in the acute phase) | Negative symptoms – normal thoughts/behaviours absent or diminished in people with schizophrenia (seen in the chronic phase) |
Psychotropic medications have an important but not exclusive role in the treatment and management of schizophrenia, with atypical or second generation antipsychotics being the treatment of choice (RANZCP Clinical Practice Guidelines Team for the Treatment of Schizophrenia and Related Disorders 2005). Psychosocial strategies and therapies such as cognitive behaviour therapy, social skills training, occupational support and retraining, and family psychoeducation and support also play a significant role in successful management and outcomes of the disorder.
Pathophysiology of schizophrenia
The pathophysiology of schizophrenia remains poorly understood. Susan Greenfield (2000) has proposed that the mind of a person with schizophrenia is overwhelmed by sensory inputs so that the boundaries between reality and illusion become blurred. She suggests that the pattern of neural communication controlling brain functions such as attention, behaviour, perception and cognition is sparse, superficial and rapidly changing.
Two pathophysiological processes associated with schizophrenia appear to dominate the literature – a dysfunction in neurotransmission and abnormal brain structure. The dysfunction in neurotransmission is thought to involve an increase in dopaminergic activation associated with the mesocorticolimbic pathway. The mesocorticolimbic pathway has its origins in the midbrain, a part of the mesencephalon. It projects to brain regions (i.e., cortex and limbic system) involved in the control of behaviour and emotions: amygdala, hippocampus, prefrontal cortex, anterior caudate nucleus and cingulate gyrus (see Fig 3.1). The excess of dopaminergic activity in this pathway in affected individuals is called the dopamine hypothesis of schizophrenia.
Altered brain structure has also been reported in the brains of people who have schizophrenia. Medial percentage regional volume reductions have been reported affecting the whole brain, amygdala and hippocampal regions, as well as the frontal and temporal lobes and their thalamic relays (Halliday 2001, Lawrie & Abukmeil 1998). Moreover, these reviews report ventricular enlargement as a common structural change in schizophrenia. Mitchell and Crow (2005) reviewed the evidence that a decreased level of normal brain lateralisation also plays a role in the pathophysiology of schizophrenia. They argued that there is reduced lateralisation of language to the left hemisphere and possibly even a trans-lateralisation of this function to the right hemisphere in schizophrenia. Language deficits are considered to be important characteristics of the symptomatology of schizophrenia. Hand preference, another characteristic of brain lateralisation, is also altered in schizophrenia as more people with schizophrenia are lefthanded and mixed-handed compared to ‘healthy’ people or mental health consumers without schizophrenia (Sommers et al 2001).
Genetics definitely plays a major part in the development of schizophrenia as a family history is considered an important risk factor. It appears that genetic make-up predisposes a person to schizophrenia, but does not determine its onset. There is interplay between genetics, environmental and developmental factors. Factors that have been implicated include gestational brain injury induced by infection (particularly viral infections like influenza), birth complications and malnutrition. Some researchers have posited seasonal effects (a higher risk associated with babies born in winter) as well as poor exposure to sunlight and deficient vitamin D levels as risk factors for schizophrenia (see van Os et al (2005) for a review). However, these hypothesised risk factors remain controversial and subject to keen debate.
A link has also been established between drug use and psychosis. The current view is that, in general, drug use is not causal in psychosis, but that there is a high rate of co-morbidity between the two. However, cannabis use remains a significant risk factor for psychosis (van Os et al 2005). Furthermore, there are poorer outcomes associated when a person with psychosis engages in substance misuse (Gregg et al 2007).
The pharmacology of antipsychotic agents
The evidence supporting the dopamine hypothesis of schizophrenia is drawn largely from empirical observations that drugs that reduce the synaptic action of dopamine in the brain attenuate the symptoms of schizophrenia, while drugs that enhance the action of dopamine (such as L-dopa or dopamine receptor agonists used in the treatment of Parkinson’s disease) can induce the symptoms of psychosis. However, although the hypothesis has been further validated through the use of imaging studies, it does fall short of explaining the complexity of the disorder (Toda & Abi-Dargham 2007).
Classic/typical or first generation antipsychotics
Centrally acting dopamine receptor antagonists have been the mainstay of antipsychotic drug therapy for decades, since the introduction of chlorpromazine in 1952. At that time, the discovery of drugs with psychotropic effects created a dramatic change in the treatment of psychosis and led to a new era in psychiatry.
At least five sub-types of central dopamine receptor have been identified. They are represented by the nomenclature D1–D5 receptors (see Table 3.2). The efficacy of the first generation or typical antipsychotic agents is strongly linked to their affinity for D2 receptors: the greater the affinity, the more potent the drug. The first generation medications are more effective in treating the positive symptoms of schizophrenia than the negative symptoms. Moreover, direct imaging studies demonstrate that the first generation antipsychotic agents do alter brain structure in schizophrenia, inducing increases in basal ganglia volumes and decreases in the volumes of different cortical regions (Scherk & Falkai 2006).
Table 3.2 Distribution and functions of dopamine receptor sub-types in the brain
| Receptor sub-type | Distribution | Functions* |
| D1 | Most widespread sub-type in the brain: striatum, limbic system, cerebral cortex, hypothalamus and thalamus | Arousal, mood, emotions and behaviour; motor function; reward and reinforcement; learning and memory |
| D2 | Mainly striatum, limbic system, cortex, hypothalamus, thalamus, pituitary and midbrain | Reward and reinforcement; arousal, mood, emotions and behaviour; learning and memory; prolactin secretion |
| D3 | Relatively specific to limbic system; also found in midbrain, cerebellum, hippocampus, temporal lobe and hypothalamus | Inhibits locomotion; emotions and cognition; prolactin secretion |
| D4 | Frontal cortex, amygdala, hippocampus, hypothalamus, midbrain and basal ganglia | Emotions, cognition and behaviour; arousal and mood |
| D5 | Hippocampus, thalamus, cerebral cortex, striatum and midbrain | Emotions and behaviour |
* A number of functions occur as a result of synergism between receptor sub-types.
A major problem with these medications, however, is that there are other dopaminergic pathways in the brain that are disrupted by this treatment. The pathways affected are an extrapyramidal system tract that modulates voluntary muscle movements and a hypothalamic–pituitary connection that regulates hormone secretion.
The motor disturbances or extrapyramidal side effects (EPSEs) that can be induced by antipsychotic medication are of four types (see Table 3.3 for an outline of EPSE symptoms and treatment):
Table 3.3 Motor disturbances associated (primarily) with first generation antipsychotic agents
| Motor disturbance | Description | Treatment |
| Dystonia | Involves the face, neck, back and upper limbs. Altered muscle tone leads to wry neck (torticollis), spasming of the eye muscles (oculogyric spasm), facial grimacing, arched back and limb spasticity. Reversible with treatment | Responds to antimuscarinic drug therapy (e.g. benztropine) and by reducing/stopping antipsychotic treatment |
| Pseudoparkinsonism | Comprises drug-induced parkinsonian symptoms of tremor, cogwheel and limb rigidity and hypokinesia. Can include slowness of thinking (bradyphrenia) and mental ‘clouding’. Reversible with treatment | Responds to antimuscarinic drug therapy and by reducing/stopping antipsychotic treatment |
| Akathisia | Marked motor restlessness where the person is fidgety, may make rocking motions, walk on the spot and/or pace rapidly. Also includes subjective feelings of restlessness, unease and/or dysphoria. Reversible with treatment | Responds to antimuscarinic drug therapy and by reducing/stopping antipsychotic treatment |
| Tardive dyskinesia | Involuntary movements of the face, tongue and limbs. Can include lip smacking, tongue writhing, chewing and/or sucking mouth movements, tic-like movements of the eyes and lips, and choreoathetoid (aimless, involuntary) movements of limbs. Often irreversible | If detected early and medication reduced or ceased, may be fully reversible. But usually does not respond to drug treatment and may not respond to reducing/stopping antipsychotic treatment. Prevention is most effective |
In general, the greater an antipsychotic medication’s affinity for the D2 receptor, the greater the likelihood of EPSEs (Therapeutic Guidelines: Psychotropic 2003). The more acute EPSEs (i.e. dystonia, akathisia and pseudoparkinsonism) can present anywhere between 24–48 hours (dystonia) and a few days–weeks (pseudoparkinsonism) following commencement of medication (Gray & Gournay 2000). Tardive dyskinesia, a chronic and often irreversible EPSE, usually presents over a longer period of time, months–years after the commencement of medication (Therapeutic Guidelines: Psychotropic 2003). EPSEs can be some of the most frightening and potentially debilitating and stigmatising side effects of the antipsychotics. As tardive dyskinesia in particular can be irreversible, it is vitally important that clinicians closely attend to early detection and management of these side effects. Refer to Box 3.2 for guidelines on detection and management.
Box 3.2 Guidelines for detection and management of epses
Gray & Gournay 2000 Therapeutic Guidelines: Psychotropics 2003
The first generations also interact with and block other receptor types including central histaminic and adrenergic receptors, as well as peripheral muscarinic cholinergic receptors. Common adverse effects of these types of interactions include sedation, weight gain, postural hypotension and atropine-like antimuscarinic reactions (such as blurred vision, tachycardia, urinary retention, constipation and facial flushing). Each of the antipsychotic agents will produce a different profile of adverse effects, which may influence the choice of medication for a particular client (see Table 3.4). There are a number of assessment tools that can be useful in identifying the side effects of antipsychotic medications, particularly EPSEs (see Box 3.3).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree