Chapter 18 Minimally Invasive Intradiscal Procedures for the Treatment of Discogenic Lower Back and Leg Pain
 Better selection criteria improve results of annuloplasty and disc decompression procedures for lower back and discogenic leg pain.
Better selection criteria improve results of annuloplasty and disc decompression procedures for lower back and discogenic leg pain. Patients with evidence of one or two levels of disc degeneration on MRI and one or two levels positive on provocative discography are desired candidates for annuloplasty.
Patients with evidence of one or two levels of disc degeneration on MRI and one or two levels positive on provocative discography are desired candidates for annuloplasty. Outcomes of the percutaneous disc decompression procedures were largely positive when used for the treatment of contained lumbar disc herniations. However, more randomized, prospective studies are needed to confirm their effectiveness.
Outcomes of the percutaneous disc decompression procedures were largely positive when used for the treatment of contained lumbar disc herniations. However, more randomized, prospective studies are needed to confirm their effectiveness. Optimal patient positioning, which includes correction of lumbar lordosis using either a soft roll or pillow placed under the mid-abdomen, will facilitate needle placement for any of the intradiscal procedures.
Optimal patient positioning, which includes correction of lumbar lordosis using either a soft roll or pillow placed under the mid-abdomen, will facilitate needle placement for any of the intradiscal procedures. During provocative discography, excessive amounts of local anesthetic injected deep, closer to the disc and foramina just prior to intradiscal needle placement, may decrease the ability of patient and operator to detect the nerve root impalement.
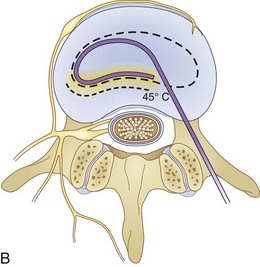
During provocative discography, excessive amounts of local anesthetic injected deep, closer to the disc and foramina just prior to intradiscal needle placement, may decrease the ability of patient and operator to detect the nerve root impalement. During intradiscal biacuplasty, although the temperature is set to 50° C on the radiofrequency generator, tissue temperature reaches about 70° C because of distal ionic heating. During this time, the patient should be awake and communicate with the physician.
During intradiscal biacuplasty, although the temperature is set to 50° C on the radiofrequency generator, tissue temperature reaches about 70° C because of distal ionic heating. During this time, the patient should be awake and communicate with the physician. Puncturing an intervertebral disc with a needle may potentially lead to progressive disc disruption. Greater progression of degenerative disc disease has been suggested in post-discography discs, and it seems to be worse in patients who had larger diameter needles inserted in their intervertebral discs.
Puncturing an intervertebral disc with a needle may potentially lead to progressive disc disruption. Greater progression of degenerative disc disease has been suggested in post-discography discs, and it seems to be worse in patients who had larger diameter needles inserted in their intervertebral discs.Introduction
Low back pain remains one of the biggest resource-consuming problems in medicine. At least 40% of the U.S. population at one time or another will use medical resources for the treatment of low back pain. Frequent sources of mechanical lower back pains are myofascial, discogenic, and facetogenic, from sacroiliac joint, compression fractures, and lumbar canal stenosis.1,2
Low back pain is the one of the most common causes of lost work time in the United States,1 and discogenic pain is one of the main causes of chronic lower back pain.3
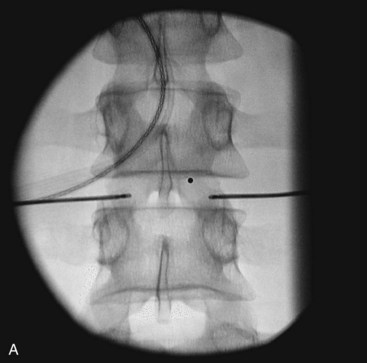
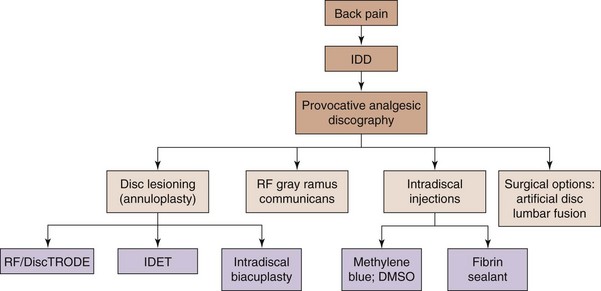
It is the aim of this chapter to briefly review new and developing interventional and minimally invasive spinal treatments for discogenic low back (Figs. 18-1 to 18-3) and leg pain caused by contained disc herniation. Also, a simple algorithm is offered in Fig. 18-4 adopted and modified for discogenic back pain4 and should only be used as a rough intervention guide. This chapter highlights some interesting, novel interventional therapeutic approaches and is not intended to be a complete guide for the treatment of patients with discogenic lower back pain. A comprehensive approach with involvement of multiple specialties and adjunct therapies, such as physical therapy and occupational interventions, are frequently required to produce significant improvement in functional capacity and pain scores of patients with chronic lower back pain.
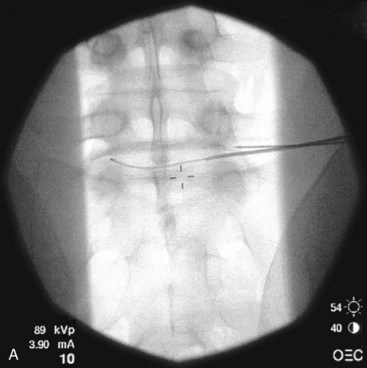
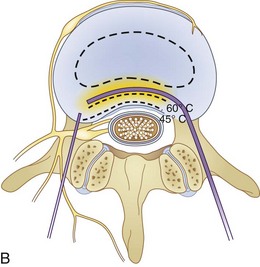
Fig. 18-1 Figs. 18-1 to 18-3 show fluoroscopic views of the final electrode positions during three different intervertebral disc heating procedures used for the treatment of discogenic pain head to head with schematic drawings of the ideal electrode placement. All three fluoroscopic views are anterior-posterior and the schematic drawings are illustrated transverse cuts through the targeted disc.
Discogenic Lower Back Pain
When evaluating patients with the main complaint of long-lasting low back pain, with or without leg pain, it is necessary to investigate the pain generator causing debilitation. More typical features of discogenic source of pain include unrelenting nociceptive low back discomfort or groin or leg pain that worsens with axial loading that improves with recumbency. These signs and reported symptoms alone are usually inadequate to confirm an accurate diagnosis.1–4 Although MRIs are helpful in visualizing such pathology as disc degeneration, desiccation, high intensity zones, and loss of disc height, these changes frequently correlate poorly with clinical findings and the presence of chronic pain, leaving open critical questions of causality.1–4 Many practitioners use provocative or analgesic diagnostic discography as a way to substantiate their clinical diagnosis of discogenic pain. Provocative or analgesic discography is the only available method to relate anatomical abnormalities seen on MRIs of the lumbar spine with clinically observed lower back pain. However, the predictive value of this test is repeatedly questioned, mainly as a consequence of potentially high false-positive rates.5–7
After provisional diagnosis of discogenic pain is introduced, an effective treatment is desired. Several commonly used minimally invasive intradiscal therapies involve careful heating of the annulus fibrosus (so-called annuloplasty procedures) (Fig. 18-4). Historically, such therapeutic modalities have been used regardless of the unclear relationship between positive therapeutic effects and absence of the histological changes expected within the annulus of the disc after heat is used.8–12 Currently, denervation of the annulus by heat destruction of the nociceptors is a plausible mechanism of pain relief. There is no evidence that collagen fibers in the annulus are significantly affected by denaturation and coalescence, possibly suggesting that the collagen alteration is an additional therapeutic mechanism for pain relief.9–12 The minimally invasive approach, low cost, and relative simplicity of these procedures are the key advantages compared with surgical procedures such as lumbar fusion and disc replacement. IDET (Smith and Nephews, London, UK), DiscTRODE (Valleylab, Boulder, CO), and intradiscal biacuplasty (Baylis Medical, Montreal, Canada) (Figs. 18-1 to 18-3) are several annuloplasty methods using heat to treat discogenic pain.
Mechanisms of Pain Relief by Annuloplasty
Dehydration of the intervertebral disc and loss of nuclear material with increasing age are associated with disc degeneration. Consequent delamination and tearing of the lamellar layers are just physical changes that can be associated with biochemical and cellular changes within the disc. Inside the degenerating disc, production of inflammatory cytokines, including tumor necrosis factor-α (TNF-α), nitric oxide, and matrix metalloproteinases are greatly altered.13,14 Neural elements that are normally limited to the outer third of the annulus penetrate farther into the degenerated disc along the vasculature and fissures.15–18 Immunohistochemical studies have shown that such nerves in growth is of nociceptive origin (C- and A-δ fibers) and likely responsible for transmitting pain responses.14,17 Elimination of these nociceptors may disrupt the transmission of pain signals.
During the application of RF, alternating flow of electrical current causes ions in the tissue to move back and forth. This alternating movement by the ions causes molecular vibration within the tissue and results in frictional heating.19,20 This effect is called ionic heating, and it can lead to thermal injury of the cells when tissue temperature reaches greater than 42° C.21 The extent of cellular damage usually depends on the amount of temperature and duration of heating.22 Increase in tissue temperature is a function of current density, or the amount of current per unit area. Current density is greatest at the proximity of the electrode and decreases with increasing distance from the electrode. However, by increasing the power output, current density around the electrode is increased, and thus the lesion size produced by ionic heating is limited by the current density.
One method of increasing lesion size or volume is by cooling the RF electrode internally. This technique was initially developed for tumor and cardiac ablation23–25 and is currently used in intradiscal biacuplasty procedure.26–28 Cooled RF probes have hollow lumens that extend to the tip of the electrode. The cooling fluid circulates in a closed loop through the hollow lumens to the tip of the electrode and back to a pump. The coolant acts as a heat sink that removes heat from the tissue adjacent to the electrode. Consequently, larger lesion volumes can be produced by increasing power deposition and the duration at which current is delivered without causing tissue charring around the electrode.23 A larger lesion volume can be produced by using two internally cooled RF electrodes in a bipolar arrangement at the lower temperature.
Intradiscal Electrothermal Therapy
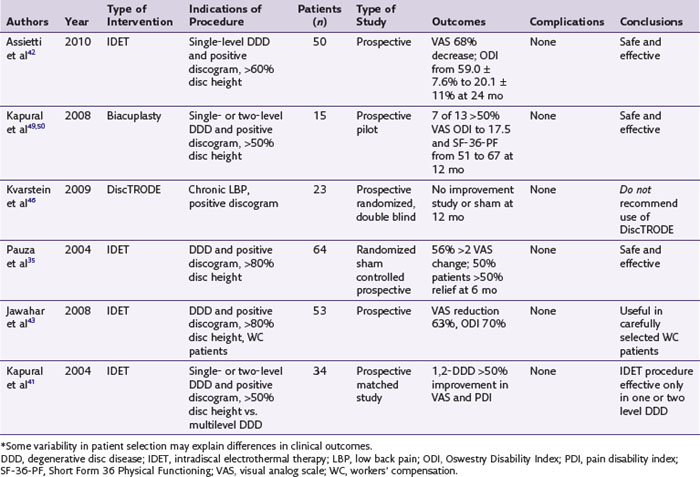
IDET technology (Figs. 18-2 and 18-4) relies on elongated resistive coil of very small diameter to deliver surrounding heat over the limited area of the posterior annulus. Possible mechanisms of pain relief were discussed above. The only difference between the IDET and other disc annuloplasty procedures is that the temperatures attained during the IDET are very high just around the electrode itself, and they dissipate relatively quickly at 2 to 4 mm radius away from the coil. The IDET procedure requires from the proceduralist a relatively long learning curve, and although it seems relatively easy to position resistive coil within the posterior annulus of the disc, multiple attempts may be required or it may be necessary to place another coil from the opposite side of the posterolateral disc to achieve optimal position within the interface between the annulus and nucleus (Fig. 18-2). This may contribute to further damage of the intervertebral disc, and sometimes placement of the tip of the coil within the posterior annular fissure may extend too close to the posterior edge of the disc. Indications for IDET include persistent discogenic low back pain despite comprehensive conservative treatments, including physical therapy, a directed home exercise program, and fluoroscopically guided epidural corticosteroid injections. The Saal brothers, inventors of the IDET catheter,29–31 used initially some additional criteria for the selection of patients, which include those with normal neurological examination results, negative results on straight-leg raise test, absence of any inflammatory arthritic or nonspinal condition that may impersonate lumbar pain, and the absence of prior surgery at the symptomatic intervertebral disc level.29–31 Provocative discography should replicate the concordant pain at low disc pressurization at up to three intervertebral disc levels. The above selection criteria disparities used in subsequent studies evaluating the effectiveness of IDET are thought to account for divergence seen in clinical results (Table 18-1).29–43
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree