CHAPTER 307 Minimally Invasive Techniques for Lumbar Disorders
Minimally invasive techniques have evolved during the past decade to affect all aspects of lumbar spine surgery, from congenital disorders to adult deformity. Surgical series have demonstrated efficacy for decompressive procedures,1 short-segment lumbar fusions,2,3 and intradural exposures to spinal tumors4–7 and to tethered cords.8 More recent efforts have involved applying this experience to reduce the morbidity of deformity procedures. The advantages of minimally invasive spine surgery include decreased postoperative pain, more rapid postoperative mobilization, shorter length of hospitalization, shorter postoperative recovery times, and less disruption to the paraspinal muscles and ligaments that contribute to the maintenance of proper spine biomechanics.
Lumbar Diskectomy
Minimally invasive lumbar microdiskectomy, as it is known in the neurosurgical community, involves a similar procedure to traditional microdiskectomy but uses muscle dilators and a tubular retractor to access the interlaminar space with less soft tissue damage. It is performed routinely through tubes ranging from 14 to 22 mm in diameter and has been successfully applied to recurrent disk herniations9,10 and far lateral disk herniations,11,12 in addition to standard disk herniations. Originally developed using an endoscope for visualization, many practitioners use the operating microscope to perform the procedure through the same exposure, and excellent results have been reported.13 Whether a simple lumbar diskectomy using a tubular retractor has significant clinical advantage over an open diskectomy with a conventional subperiosteal muscle dissection and muscle retraction with a Taylor or Thompson-Farley retractor remains a matter of debate.14,15 However, when one considers the increased incisional length and muscle dissection required for proper exposure during a midline approach in heavy patients with typical disk herniations or in all patients with far lateral disk herniations, the advantages of using a tubular retractor centered directly over the site of pathology become obvious.
Stenosis Decompression
Although the advantages of minimally invasive techniques for microdiskectomy may be debatable, the advantages are clearer for patients with lumbar stenosis requiring a bilateral decompression. Through the same-sized incision as a microdiskectomy, a one-level or two-level stenosis decompression can be performed. Several variations of this procedure have been described, but all share the essential strategy of a bilateral decompression through a hemilaminar approach. This strategy has been proved feasible and effective in large clinical series.1,16
Lumbar Fusion
Minimally Invasive Transforaminal Interbody Fusion
The indications for minimally invasive fusions are the same as for open fusions. The best studied of these techniques is the minimally invasive TLIF developed by Foley and Fessler.2,17,18 Its advantages include less blood loss, decreased perioperative narcotic requirements, and decreased length of stay compared with open lumbar fusions. Beyond a clear perioperative superiority, surgical results from open and minimally invasive fusions are similar in terms of validated self-reported patient outcomes after 1 year.3
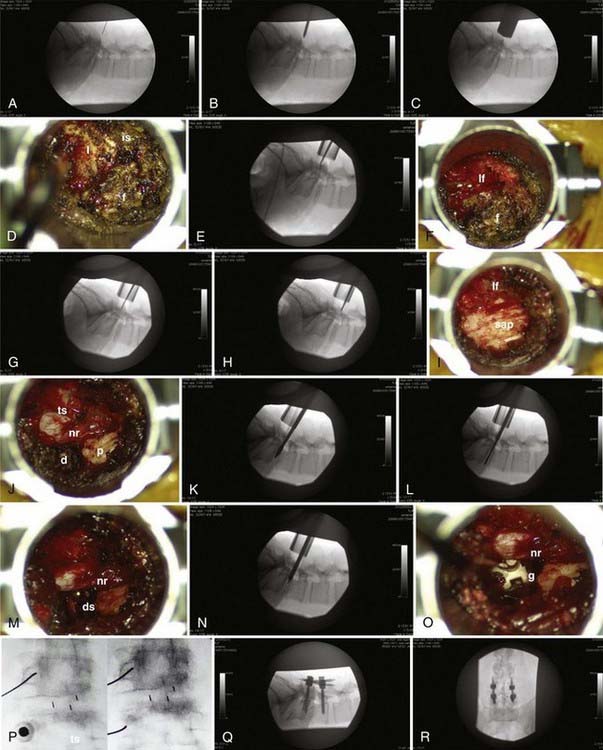
The procedure can be considered in two parts (Fig. 307-1): the interbody fusion and the percutaneous placement of pedicle screw fixation. An incision 2.5 to 3 cm long is made 3 to 5 cm off of midline. This distance is determined by the thickness of overlying soft tissues and can be measured on preoperative imaging to provide the desired working angle. A K wire is angled medially 35 to 45 degrees and docked on the facet joint. After muscle dilation, a working channel 22 to 26 mm is introduced directly over and perpendicular to the disk space, spanning the pedicles. After removal of residual soft tissue, the lamina, facet, and interlaminar space are identified. The canal is defined with curets, and a laminotomy is performed, exposing the ligamentum flavum. The inferior articular process is removed using an osteotome, drill, or rongeurs. All bone is saved for the interbody arthrodesis. The superior articular process is removed, as is the ligamentum flavum. The pedicle inferior to the disk space is identified, as are the exiting nerve root and disk anulus. The anulus is cleaned off of fat and epidural veins and incised. A series of pituitary rongeurs, curets, and scrapers are used to remove the intervertebral disk. An interbody graft is placed along with the arthrodesis material of the surgeon’s choice. Hemostasis is achieved, and the working channel is removed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree