Miscellaneous Conditions of the Cervical Spine: Neurofibromatosis, Juvenile Rheumatoid Arthritis, and Rickets
Viral V. Jain
Alvin H. Crawford
Knowledge of pediatric cervical spine disorders in neurofibromatosis (NF), juvenile rheumatoid arthritis (JRA), and rickets is essential for the pediatric orthopaedist and the spine surgeon. Detailed evaluation and appropriate early management may prevent potential serious neurologic insult and other complications related to the cervical spine.
NEUROFIBROMATOSIS
BACKGROUND
NF is a spectrum of multifaceted diseases with a wide range of clinical manifestations that have in common the presence of schwannomas, neurofibromas, and/or café au lait spots (1). Clinically, this multisystemic, hereditary disease may manifest as abnormalities of the skin, nervous tissue, bones, and soft tissues. The primary pathology is believed to be a hamartomatous disorder of neural crest derivation. Akenside (2), in 1768, described a patient with multiple NF: however, first credit is most frequently given to Wilhelm G. Tilesius von Tilenau (3) for his 1793 clinical description of a patient with NF. In 1882, Frederick Daniel von Recklinghausen (4) coined the term neurofibroma, and he was able to demonstrate that a small cutaneous nerve was connected to each of the cutaneous and subcutaneous tumors. Prior to this, the terms dermal fibroma or false neuroma had been applied to the nodules. Thus, von Recklinghausen, with his clinical and pathologic description, was the first to associate the origin of the disorder to tumors from arising nerve sheaths (4).
TYPES OF NEUROFIBROMATOSIS
NFs are a group of genetic multisystem disorders involving products of all three germ lines: neuroectoderm, mesoderm, and endoderm. Four varieties of this disorder have been described. The most common form is neurofibromatosis type 1 (NF1), previously known as von Recklinghausen disease, which involves predominantly peripheral nervous system although it involves cells of mesodermal origin as well. NF2 is the second most common form of the disorder involving the central nervous system and is associated with bilateral vestibular schwannomas and multiple spinal schwannomas. Segmental NF is considered to be a mosaic form of NF1 with features of NF1 present in single body segment (1). Schwannomatosis is the most recently described form manifesting itself as multiple deep painful schwannomas and is thought to represent a mosaic form of NF2 (5). Since NF1 is the only form associated with the disorders of the spine, all the discussion in this chapter focuses on NF1.
EPIDEMIOLOGY AND GENETICS
NF1 is one of the most common autosomal dominant disorders with a prevalence rate of 1:4,000 (6). It occurs almost equally in all ethnic groups (7). Approximately 50% of all cases of NF1 are due to new mutations. The NF1 gene mutations have variable expression—the clinical manifestations of NF1 range from subclinical to severe. However, it has nearly 100% penetrance in adult individuals; therefore, an adult carrying the mutation will eventually exhibit some clinical feature of the disease (8). The NF1 gene is located on the long arm of chromosome 17 (17q) and is of relatively large size (350,000 bp). This may explain the large rate of new mutations associated with this disorder. The gene product neurofibromin acts as a tumor suppressor gene (9). Direct sequencing of the NF1 gene is now available for genetic testing. In contrast to the
previously used protein truncation assay that only detected 60% to 70% of NF1 mutations, it detects the mutation in 95% and is considered as the gold standard (10,11). Animal models such as knockout mouse are now available that will greatly increase our understandings of the disease and help in development of therapeutic strategies.
previously used protein truncation assay that only detected 60% to 70% of NF1 mutations, it detects the mutation in 95% and is considered as the gold standard (10,11). Animal models such as knockout mouse are now available that will greatly increase our understandings of the disease and help in development of therapeutic strategies.
CLINICAL FEATURES
The most characteristic clinical features of NF1 are multiple hyperpigmented areas (café au lait macules) and neurofibroma. The Consensus Development Conference of the National Institutes of Health has published diagnostic criteria of NF1 in 1987 Table 32.1. The presence of two or more of the criteria is essential for establishing the diagnosis of NF1 (12). Since the consensus panel meeting, specific kinds of learning disabilities and MRI abnormalities (especially in children) have been associated specifically with NF1. These are useful even during early life (13). More recently, ventrolateral bowing of the tibia has been considered as one of the criteria for the diagnosis of NF1 (14). Axillary freckling and, especially, café au lait spots occur very early and may be the only easily noticeable manifestations of the disease in very young children. Other conditions presenting with similar pigmented macules include Watson’s syndrome, McCune-Albright syndrome, LEOPARD syndrome (lentigines, electrocardiogram abnormalities, ocular hypertelorism, pulmonary stenosis, abnormalities of genitalia, retardation of growth, and deafness), and Noonan’s syndrome.
There are two peaks of severe clinical problems in NF1 patients: one peak from 5 to 10 years of age and a second from 36 to 50 years of age. At the second peak, 75% of the clinical problems are related to malignant neoplasms (15).
Genetic testing should be utilized to confirm or rule out the diagnosis of NF1 in uncertain cases especially in young children with presence of café au lait spots only. For individuals who meet clinical diagnostic criteria for NF1, molecular testing is generally not felt to be necessary for diagnostic purposes.
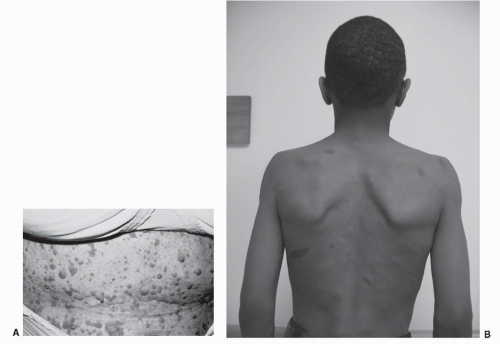
Café au Lait Spots
Café au lait spots are present in well over 99% of all patients with NF1. The pigmentation is tan, macular, and melanotic in origin and is located in and around the basal layer of the epidermis; the lesions may vary in shape, size, number, and location (Fig. 32.1A). In NF1, these spots are frequently found in areas of the skin not exposed to the sun. The presence of one café au lait spot may be normal.
TABLE 32.1 Diagnostic Criteria of NF1 | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Lisch Nodules
Lisch nodules, or iris-pigmented hamartomas, are present in 94% of patients with NF1 who are 6 years of age or older; 28% of younger patients have them. They increase in number with age (16), but they do not become symptomatic. The lesions appear to be specific for von Recklinghausen’s NF1; they are not seen in normal persons or in patients with central acoustic NF or segmental NF.
Neurofibromas
Neurofibromas mostly involve the skin, but they may be seen in deeper peripheral nerves. They may be nodular and discrete or diffuse with interdigitation with surrounding tissues. Highly vascular plexiform neurofibromas may cause segmental or localized hypertrophy. Puberty or pregnancy may cause an increase in the size and number of the lesions. It is quite rare for neurofibromas to be present in the absence of café au lait spots (17).
Cutaneous Neurofibroma
Cutaneous neurofibromas, formerly called fibroma molluscum, are found in subcutaneous tissues, after puberty. They are usually manifestations of long-standing or adult disease and do not occur with any frequency (12%) in childhood (18) (Fig. 32.1B). Recent electron microscopy studies have demonstrated that axons and Schwann cells are present in these tumors; therefore, it is appropriate that they be included under the term dermal neurofibroma.
Elephantiasis
Frequently, large soft tissue masses are seen in NF1. These masses have been termed pachydermatocele or elephantiasis neuromatosa and are characterized by a rough, raised, villous type of skin hypertrophy presenting an unmistakable appearance. There is usually dysplasia of the underlying bone when the lesion occurs in an extremity.
Pigmented Nevi
Eight percent of all patients presenting with NF1 have pigmented nevi, some presenting with geographic descriptions, for example, “nevus lateralis” and “bathing trunk.” The nevus lateralus can be described as dark brown, pigmented skin over half the abdominal wall or back, with an abrupt change of pigmentation occurring along the midline. Nevi or hyperpigmentation may be present in up to 6% of children with NF1 (18).
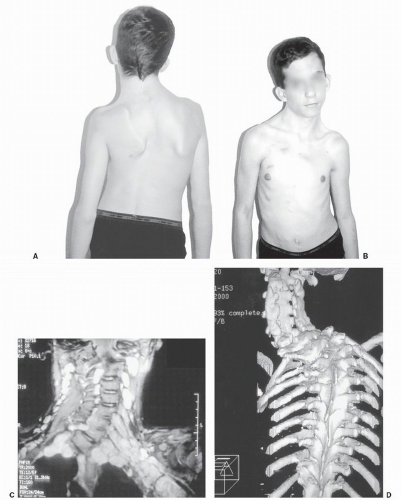
Plexiform Neurofibroma
Plexiform neurofibromas are subcutaneous neurofibromas that have a ropy, “bag of worms” feeling. Their cutaneous involvement may cause decreased sensation, causing sores to develop under a brace or cast without the patient’s knowledge, or they may be hypersensitive. When a plexiform neurofibroma is found underlying an area of dorsal cutaneous hyperpigmentation, especially when the pigmentation approaches or crosses the midline of the body, it appears that the tumor will be aggressive and may originate from the spinal canal. (Figs. 32.2 and 32.3) The plexiform neurofibroma has the potential for malignant degeneration (18).
Optic Gliomas
Although optic gliomas account for only 2% to 5% of all brain tumors in childhood, as many as 70% of cases are found in persons with NF1. In many NF1 patients, these tumors change little in size over many years, but a small percentage of such tumors may enlarge rapidly, leading to exophthalmos and visual impairment.
Verrucous Hyperplasia
Verrucous hyperplasia is an infrequent but definite cutaneous lesion of NF1. There is tremendous overgrowth of the skin, with thickening of a velvety-soft papillary quality. Many crevices form and tend to break down easily, with some weeping occurring in the skin folds. The sites often become superficially infected and may give rise to a foul odor. The lesion presents most often unilaterally and can be considered one of the most grotesque lesions of NF1.
Axillary and Inguinal Freckling
Freckles—diffuse, small, hyperpigmented spots up to 2 to 3 mm in diameter found in the armpits and inguinal region (areas not usually exposed to sunlight)—are helpful diagnostic criteria for NF1. Freckling and an occasional dermal fibroma may be the only physical findings in the parent of a child who shows all the criteria required for the diagnosis of NF1.
Spinal Deformities
Spinal deformities are the most common orthopaedic manifestation of NF1. True incidence of spinal deformities in NF1 is not known. It is quoted as from 2% to 36% in the literature (19,20). In the NF clinic at our institution, it is 23% (6). In
a report in 1988, Winter et al. (21) found only 102 patients having NF1 by clinical criteria in a pool of approximately 10,000 patients with scoliosis. Functional scoliosis resulting from limb hypertrophy or long-bone dysplasia leading to limb length inequality must be ruled out in patients with NF1. Rarely, unrecognized extrapleural thoracic tumors can present as focal scoliosis. These lesions are usually plexiform neurofibroma and are not visible on plain radiographs (22). The spinal deformities tend to develop early in the life; therefore, all preadolescent children with NF1 should be evaluated by scoliosis screening or the Adam forward bend test to rule out the presence of a spinal deformity.
a report in 1988, Winter et al. (21) found only 102 patients having NF1 by clinical criteria in a pool of approximately 10,000 patients with scoliosis. Functional scoliosis resulting from limb hypertrophy or long-bone dysplasia leading to limb length inequality must be ruled out in patients with NF1. Rarely, unrecognized extrapleural thoracic tumors can present as focal scoliosis. These lesions are usually plexiform neurofibroma and are not visible on plain radiographs (22). The spinal deformities tend to develop early in the life; therefore, all preadolescent children with NF1 should be evaluated by scoliosis screening or the Adam forward bend test to rule out the presence of a spinal deformity.
Traditionally, two forms of spinal deformities are described in NF1: dystrophic and nondystrophic. The
distinctions between these two varieties of spinal deformities are clearer in the thoracic and thoracolumbar regions. Nondystrophic curves are similar to idiopathic curves with some exceptions. The dystrophic changes in NF1 are described in the Table 32.2. The cause of dystrophic changes may be intrinsic or associated with anomalies of the spinal canal secondary to abnormalities of the spinal cord/dura mater such as tumors, meningoceles, and/or dural ectasia. Dystrophic changes may also occur even if the intraspinal contents are normal. Several investigators have suggested that there is no standard pattern of spinal deformity in NF1 and that the types of curvature are variable (23,24).
distinctions between these two varieties of spinal deformities are clearer in the thoracic and thoracolumbar regions. Nondystrophic curves are similar to idiopathic curves with some exceptions. The dystrophic changes in NF1 are described in the Table 32.2. The cause of dystrophic changes may be intrinsic or associated with anomalies of the spinal canal secondary to abnormalities of the spinal cord/dura mater such as tumors, meningoceles, and/or dural ectasia. Dystrophic changes may also occur even if the intraspinal contents are normal. Several investigators have suggested that there is no standard pattern of spinal deformity in NF1 and that the types of curvature are variable (23,24).
TABLE 32.2 Characteristics of Dystrophic Spine | ||||||||
|---|---|---|---|---|---|---|---|---|
|
CERVICAL SPINE ABNORMALITIES
The cervical spine in patients with NF1 has not received much attention in the literature (25). Cervical abnormalities are more likely to be overlooked when scoliosis or kyphoscoliosis is present in the thoracolumbar region, which distracts the examiner’s attention to the more obvious deformity. Often, the cervical lesion is asymptomatic. When the lesion is symptomatic, pain is the most common presenting symptom (26). The clinical consequences of cervical NF1 are less remarkable than in other regions because cord versus canal diameter is less critical. Because of its generally asymptomatic nature, the problem is probably underreported. However, these lesions should not be disregarded because the tendency of the disease to progress has led to severe neurologic deficits in several cases (27,28).
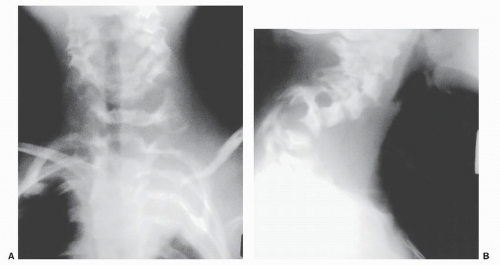
Cervical Kyphosis
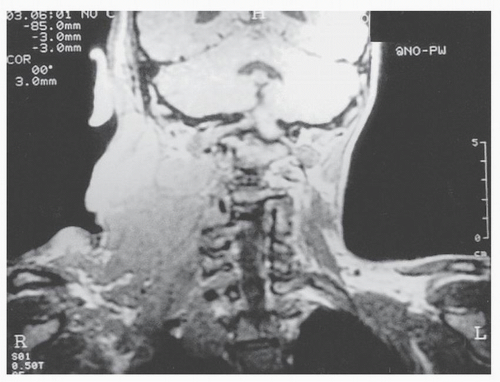
The most common abnormality is a severe cervical kyphosis (Fig. 32.4), which is most often seen following surgery and is highly suggestive of the disorder (29). Yong-Hing et al. (25) reported on 56 patients with NF1, of whom 17 patients (30%) were found to have cervical abnormalities. Of these, seven patients were asymptomatic (the rest had either limited motion or pain in the
neck), and four patients had neurologic deficits, which probably could be attributed to cervical instability. Four of the seventeen patients required fusion of the cervical spine. Curtis et al. (30) described eight patients with paraplegia and NF1. In four of these patients, the paraplegia was due to cervical spine instability or cervical intraspinal pathology.
neck), and four patients had neurologic deficits, which probably could be attributed to cervical instability. Four of the seventeen patients required fusion of the cervical spine. Curtis et al. (30) described eight patients with paraplegia and NF1. In four of these patients, the paraplegia was due to cervical spine instability or cervical intraspinal pathology.
Atlantoaxial Instability
Attention should also be paid to the C1-C2 region. Isu et al. (31) described three patients with NF1 who had a C1-on-C2 dislocation with a neurologic deficit, all three of whom improved after decompression and/or fusion. They pointed out that laxity of capsular and ligamentous structures in patients with NF1 may contribute to a predisposition to instability of the cervical spine. It is worthwhile to note that no osseous changes in the C1 to C2 relation were seen on the flexion-extension radiographs in any of these patients (28). Therefore, relying only on these views to detect instability is unwise. Five cases of atlantoaxial dislocation have been reported in patients with NF1, two of whom were noted to have neurofibromas between the odontoid and ventral arch of C1 (25,31).
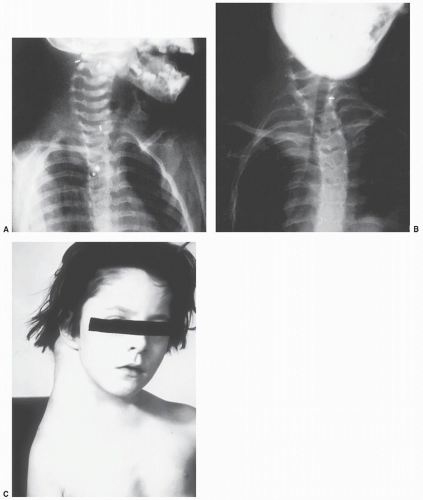
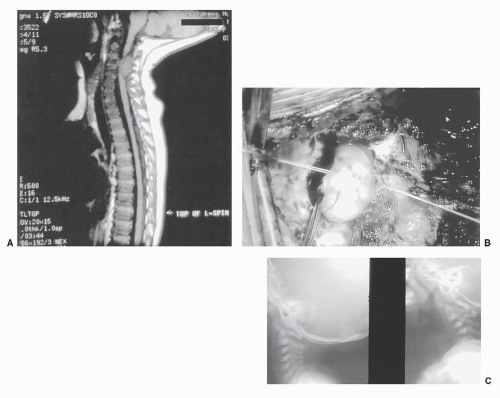
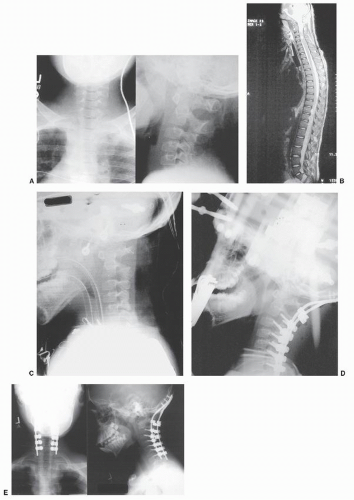
Postlaminectomy Kyphosis
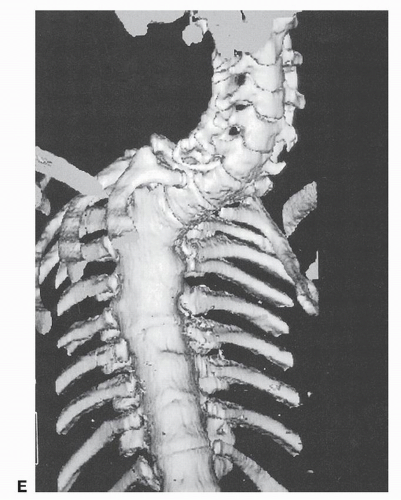
Adkins and Ratvich (32) reviewed 85 patients with von Recklinghausen’s NF1 and found that head and neck masses were responsible for 22% of the patients’ complaints. Most of the problems that we have seen in the cervical spine were those that occurred after excision of tumors, the operations for which included resection of the laminae and dorsal elements (Figs. 32.4, 32.5 and 32.6). Postoperatively, the spine is unstable and tends to develop progressive kyphosis. Therefore, it is important to be aware of the patient with NF1 who presents with a scar in and about the neck and gives a history of having a mass removed in the past. Collaborative efforts with neurosurgery colleagues to stabilize the spinal column at the time of removal of tumors from the spinal canal is the best approach to prevent this complication (Fig. 32.7).
Vertebral Column Dislocation
Complete dislocation of the spine in NF1 is rare. Involvement of the cervical spine by NF1 was noted in one study in which five patients had subluxation of a cervical vertebral body (33). In a second study of 56 patients, 17 had abnormal cervical spines; one patient had a fixed subluxation of the second cervical vertebra on the third, and another had an atlantoaxial rotatory instability (25). Rockower et al. (34) reported two cases of spinal dislocation after minor trauma in children who had NF1. One patient had a dislocation of the fourth thoracic vertebra on the fifth and no neurologic deficit. At surgery, neurofibromatous tissue was found to envelop the vertebral bodies ventrally but not dorsally. The second patient had a dislocation of the sixth cervical vertebra on the seventh and was quadriparetic. Stone et al. (35) reported on a 9-year-old child with NF1 who
had complete dislocation of the first thoracic vertebra on the second ventrally, with the body of the seventh cervical vertebra situated completely ventral to that of the second thoracic vertebra following a 2-day history of pain in the lower part of the neck. Complete reduction following traction and manipulation was not successful. Surgery resulted in the child having a solid union with no neurologic deficits. They believed that dural ectasia produced erosion of the middle column of the spine, with dissociation of the dorsal elements from the body of the first thoracic vertebra and complete dislocation of the first thoracic vertebra on the second.
had complete dislocation of the first thoracic vertebra on the second ventrally, with the body of the seventh cervical vertebra situated completely ventral to that of the second thoracic vertebra following a 2-day history of pain in the lower part of the neck. Complete reduction following traction and manipulation was not successful. Surgery resulted in the child having a solid union with no neurologic deficits. They believed that dural ectasia produced erosion of the middle column of the spine, with dissociation of the dorsal elements from the body of the first thoracic vertebra and complete dislocation of the first thoracic vertebra on the second.
Significant subluxation or dislocation of the spine in patients who have NF1 can occur with little radiographic or clinical warning, because the osseous erosion is so extensive. This diagnosis should be considered in any patient who has NF1 and unexplained pain in the neck or back. Although similar erosion of bone can be caused by tumor tissue, with modern diagnostic techniques such as computed tomography (CT), myelography, and especially magnetic resonance imaging (MRI), one can easily distinguish between tumor and ectasia. Aggressive surgical stabilization should be carried out when radiographic examination reveals instability of the spine, which may precede dislocation (36,37).
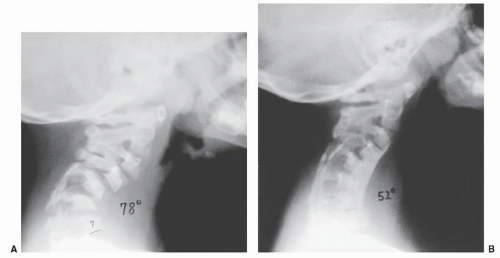
Diagnosis
Anteroposterior and lateral cervical radiographs should be made for all patients with NF1 who (a) undergo surgery, (b) require endotracheal anesthesia, (c) require cranial traction, or (d) present with neck tumors. If there is any suspicion of subluxation, CT or flexion-extension MRI scans are appropriate studies. Other reasons for obtaining radiographs of the cervical spine in the patient with NF1 include ruling out the presence of torticollis or dysphagia (37). On plain radiograph, careful attention should be directed to the sagittal plane for evidence of abnormal lordosis, kyphosis, or dystrophic changes (Fig. 32.8 and 32.8). If dystrophic changes are present, oblique radiographs to rule out so-called dumbbell lesions (Fig. 32.10B) and lateral flexion and extension radiographs to rule out instability should be obtained. One should be suspicious of dorsal scalloping of the vertebral bodies indicating the presence of a spinal canal lesion.
Because we have seen patients with erosive defects in the skull, it is important to obtain skull radiographs prior to applying halo or Gardner-Wells tong traction pins. Stabilization of these patients has been improved by the addition of pedicle screw anchors when laminectomy has been necessary. A reformatted CT scan is extremely helpful to evaluate the osseous anatomy of the cervical spine. CT has been used extensively to identify the occasional abnormal structure of the spine in NF1; it allows one to assess the spinal canal, its contents, and the associated anatomy. Three-dimensional reconstruction enhances the explicitness of the bony detail. The addition of contrast myelography to CT has allowed the surgeon to identify lesions found in and about the spinal canal. MRI should be utilized to determine the internal contents of the spinal canal and will show the presence of lesions within and about the spinal cord itself. There are occasional problems interpreting magnetic resonance image of severe deformities because of distortion brought on by complex three-plane deformity of kyphoscoliosis (38).
Management
Ogilvie reported on the surgical treatment of cervical kyphosis by ventral fusion with iliac crest or fibular bone
graft or both. He considered halo traction to be a useful preoperative step if the kyphosis was greater than 45 degrees. When progressive cervical kyphosis is the presenting deformity, preoperative halo traction of flexible deformities, followed by dorsal fusion, is the treatment of choice (Fig. 32.6). If the deformity is rigid, then soft tissue release followed by traction is believed to be safer. If sufficient bone stock is present, internal fixation with rods, wires, screws, or hooks may be used. Sublaminar wire fixation may be difficult secondary to dural ectasia and osseous fragility. If there is osteolysis with poor bone stock of the vertebral body, combined ventral and dorsal fusion is needed, and postoperative immobilization with use of a halo vest is recommended.
graft or both. He considered halo traction to be a useful preoperative step if the kyphosis was greater than 45 degrees. When progressive cervical kyphosis is the presenting deformity, preoperative halo traction of flexible deformities, followed by dorsal fusion, is the treatment of choice (Fig. 32.6). If the deformity is rigid, then soft tissue release followed by traction is believed to be safer. If sufficient bone stock is present, internal fixation with rods, wires, screws, or hooks may be used. Sublaminar wire fixation may be difficult secondary to dural ectasia and osseous fragility. If there is osteolysis with poor bone stock of the vertebral body, combined ventral and dorsal fusion is needed, and postoperative immobilization with use of a halo vest is recommended.
Trapdoor Procedure
A few of the NF1 patients develop very high thoracic curve extending in the cervicothoracic junction. These patients need fusion and instrumentation in lower cervical and upper thoracic spine. This group of patients may benefit from a “trapdoor” sternal split approach if ventral fusion is needed (39,40). This approach allows ventral exposure of the lower cervical and upper thoracic spine. Bracing may need to be extended to the cervical region in cases of severe dysplastic curves that are instrumented into the upper thoracic and cervicothoracic region. Cervical bracing, halo vest, or Minerva casting may help to prevent the possibility of screw/hook pullout. This is especially true for dysplastic curves that have low bone mineral density (9).
NEUROLOGIC DEFICITS
A number of authors have reported development of neurologic deficits in patients with NF1 (30,41). Possible etiology could be related to intraspinal tumors, instability of the vertebral column, fibrofatty tissue reaction, severe kyphosis, vertebral subluxation, dislocation, protrusion of ribs into the spinal canal, or progressive dystrophy of the bony elements of the spine. A neoplasm is usually responsible for paraplegia in older patients, whereas spinal malalignment or ribs displacing into the spinal canal is the most common cause in younger individuals. Kyphosis contributes more than scoliosis to neurologic impairment. The patients of NF1 with neurologic deficits, the distinction must be made between intraspinal lesion versus angular kyphotic deformity causing spinal cord compression. Those with severe spinal curvatures without significant kyphosis and with evidence of neurologic deficits should be assumed to have intraspinal lesions until proved otherwise.
Winter et al. (21) reported two cases of paralysis due to contusion of the spinal cord by the subperiosteal elevation during exposure of the dorsal elements in patients who had unsuspected areas of laminar erosion due to dural ectasia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree