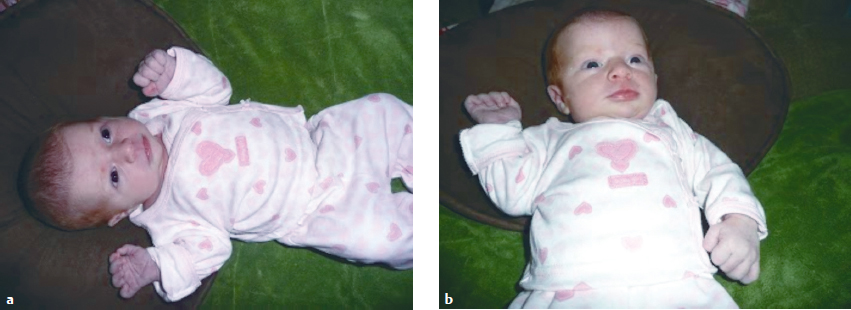
14 Motor Development As movement develops, it changes the way in which typical and atypical individuals manipulate and interact in their environment. This chapter examines motor development (MD) and postural control across the life span. It presents MD as a dynamic process emerging from changes in the neural and body systems that are influenced by exploration, stimulation, and learning in various contexts. Neuro-Developmental Treatment (NDT) practice relies on understanding the variation and predictability of MD and the connection to the various sensory systems to create intervention strategies that are age appropriate and meaningful. Learning Objectives Upon completing this chapter the reader will be able to do the following: • Link the NDT assumptions to the current principles of MD. • Apply the principles of MD to changes in movement throughout the life span for both typical individuals and those with neuromotor dysfunction. • Describe the stages and sequences of MD. • Describe the development of postural control and its influence on functional motor skills. • Explain the importance of variability and competition of motor patterns in building meaningful movement. • Explain the sensory systems’ contributions to functional movement in the developing child. • Describe the features of the musculoskeletal system that support MD. • Analyze how MD influences the way individuals interact, experience, and learn from the environment. • List ways in which various aspects of MD impact NDT intervention. As Campbell states, “Working knowledge of motor development is the very basis of the practice of pediatric physical therapy.”1 Knowledge of motor development (MD) is equally critical for occupational and speech-language pathologists working with children because MD changes the way children manipulate and interact in their environments.2 MD provides norms for (1) identifying competencies and impairments in developing body systems, (2) developing effective plans of care, (3) establishing age-appropriate skills as functional outcomes, (4) structuring intervention strategies to facilitate learning and motor control, and (5) selecting play and activities of daily living and contextual factors to promote participation in real-life settings. Therapists who work with adults know that changes in the expression of motor milestones continue across the life span. These changes influence social development and quality of life, including education, employment, and independent living.3 For older adults, the aging process may require new motor strategies and adaptation of motor skills to accommodate stiffer joints, weaker muscles, and changes in vision, hearing, and balance.4,5,6 Neuro-Developmental Treatment (NDT) has always had a strong foundation in MD. Almost since the inception of their approach, the Bobaths7 wrote and taught that understanding the development of posture and movement, and the changes that occur over time, provided the means for recognizing differences in typical movement and movement pathology. In an NDT framework, MD is considered a process that occurs throughout the life span. In children, movement repertoires develop, are refined, and adapt as a child grows, and responds to and learns from the demands of new contexts. Different movements are needed to cope with typical aging processes. Older adults may shorten their step and stride length, use hand support to ascend and descend stairs, hyperextend their neck to accommodate bifocals, and tilt or turn their head to listen with a better ear. Throughout life, experience and learning within specific environmental contexts strengthen certain motor behaviors, and at the same time provide opportunities for change. Therefore, in the NDT framework, MD is viewed as a lifelong process that explains uniquely individual motor characteristics while retaining the same general form of motor behavior at any point in time. Over time, researchers have offered different perspectives in MD. From the 1920s through the 1940s, MD was viewed as a neural-maturational process; genetic instructions were viewed as the driving force.8,9,10,11 Reflexes were considered the foundation of movement, and MD was thought to proceed from reflexive movement to highly skilled movement as the levels of the central nervous system (CNS) matured.7 The inhibition of reflexive movement brought about an orderly and predetermined progression of postural reactions and motor milestones that each child passed through on the way to adulthood. After maturity, the adult CNS was hardwired and fixed, and any substantial recovery of function was impossible no matter what intervention was used.10 Health care practitioners adopted a “wait and see” attitude. Although this practice persisted for many years, the Bobaths insisted that it was possible to produce changes in MD with specific intervention strategies.7 An initial shift of paradigm came from behavioral theories that stressed interactions between the infant and the environment. Skinner and Piaget emphasized the significance of environmental opportunities and the importance of learning and reinforcement on motor behavior.12,13 This shift paralleled changes in thinking about motor control as described in Chapter 12 of this unit. The impact that this had on the NDT approach was to shift the center of attention from facilitating motor progression to include exploratory movements and problem-solving activities for motivation and a focus on the importance of a supportive environment to foster and shape MD. The next shift in thinking has been the introduction of dynamic theories in motor control put forth by Bernstein and Edelman (see Chapter 12) and applied to MD development by Thelen14,15 and Hadders-Algra, among others.16,17,18,19 This new paradigm placed motor milestones as the end product of a complex and variable schema. Today, MD is thought to emerge from the cooperation and dynamic interactions of many subsystems—intrinsic and extrinsic—in task-specific contexts. Development of specific motor behaviors depends on a balanced combination of neural and body systems, including the biomechanical, kinematic, and anthropometric changes; cognitive and perceptual factors; and the individual genetic code (nature) and an environment that provides a context for experience and learning (nurture). The current NDT practice emphasizes variability—the way in which children carry out a particular motor function, and predictability—the progression of MD.20,21,22 These concepts underlie NDT assumptions in MD. 1. MD is a dynamic process rather than a linear progression that occurs throughout the life span and changes the way individuals interact with their environment. 2. MD emerges from the cooperation and changes in the neural and body systems that are influenced by exploration, stimulation, and learning in various contexts. 3. Body systems develop at different rates, enhancing or constraining the development of various motor behaviors. 4. Directionality of development, such as cephalocaudal and proximodistal, is only a general schema, whereas functional, skilled movement is a composite of postural stability and mobility patterns that support the observable function. 5. Newborns have primary motor repertoires that are complex and variable, but such repertoires must be connected to sensory input and feedback within context to result in meaningful actions. 6. The development of posture and movement is dependent on different muscle physiology and neural pathways; efficient motor function depends on the integration of these two aspects of motor behavior. 7. The various sensory systems—visual, olfactory, auditory, somatosensory (tactile and proprioceptive) and vestibular—are key elements in MD. 8. Motor milestones appear as discontinuous, discrete behaviors with a definable onset but actually result from continuous processes involving all the developing body systems. 9. Variability and competition among motor patterns are essential components of MD. 10. Understanding typical and atypical motor patterns that underlie motor function can enable one to identify differences in movement in both children and adults with CNS pathology. 11. MD provides guidelines for creating intervention strategies that are age appropriate and facilitate variation in movement and enhance motor learning. Stages of development reflect observable motor skills that are often described as motor milestones. The goals of MD are to develop upright posture, mobility, speech, and manipulation for mastery and control in changing contexts. Perfecting these skills leads to functional activities, including self-care, play, and social interactions. Knowledge about the stages of motor development addresses the question, What can I expect of infants at various ages? The answers provide a starting point for observing and identifying differences in typical and atypical development. What drives or constrains MD in a specific child requires an in-depth analysis of the processes underlying motor skills. Therapists start by examining observable motor activities to decide if a child’s MD is progressing as expected, taking into account individuality, culture, and experience. Various authors describe and illustrate the observable stages of motor milestones in children, including the progression of a stable head posture, rolling, transitions from prone to sitting and four-point position, creeping, pulling to stand, standing and walking, babbling and speaking, reaching, grasping, and hand control.23,24,25,26 As these postures or movements are attained, further development entails perfecting postural control in the new position and effortless transitions from one posture to another. As stated in the first assumption, MD is not viewed as a linear progression but as a dynamic one in which body structures and functions jointly mature, albeit at different rates, ultimately leading to observable milestones. From birth onward, infants begin with movement repertoires that are unique, complex, and species specific. These primary repertoires, listed in Chapter 12, sustain life and serve the newborn’s basic needs. Infants have a challenging job; they must cope with variability, link sensory input to multiple motor possibilities, determine which movements have (or will have) value in their lives, and solve increasingly complex problems that occur as they confront the force of gravity; all this while their own body is changing and growing. Neonates are gravity dependent, and their motor development begins as they discover, from among endless combinations, preferred motor patterns that are stable yet adaptable. At every age, emerging motor behavior must be adaptable enough to change along with changes in the musculoskeletal system (and other body systems) and with the intent of the movement, yet be stable enough to permit specific motor function to occur in spite of changes in the body systems or intent. NDT therapists know that observing the progression of the stages of MD is just a starting point in understanding motor behavior. Directionality, such as cephalocaudal and proximodistal, is only a general schema.23 The development of skilled movement is a composite of influences, and assigning developmental direction depends on (1) coordination of various parts of the body performing different functions (such as stability or mobility), (2) the interaction and feedback from the environment in which the motor function takes place, and (3) the purpose or goal.27 For example, head lifting from prone is an early benchmark of typical development. Head lifting begins in the first month and involves the muscles of the cervical spine and neck as the infant lifts and rights the head. This movement to clear the airway is seen before the infant activates postural muscles deep in the neck to sustain the posture against the force of gravity. Stability of the head in prone also requires concurrent biomechanical changes in the lower trunk, pelvis, and legs (Fig. 14.1a, b) In the newborn, head lifting is constrained by the flexed position of the legs and the lack of spinal extension. Newborns can turn their head to clear the airway while prone, an important life-sustaining primary repertoire (see Chapter 12 for information on primary repertoires). Initially, the overall flexed posture of the lower extremities raises the pelvis higher than the shoulders so that the center of mass (COM) is forward and much of the infant’s weight is on the shoulders, arms, and face. This posture, combined with the large mass of the infant’s head, makes head lifting against gravity nearly impossible. Although the weight on the face may constrain head lifting, it provides an important sensory experience to the lips and cheeks as they make contact with the surface as the infant attempts to turn or lift the head. This experience guides the organization for later active oral-motor activity.26 By 3 to 4 months of age, as infants activate their body against the force of gravity, the hips extend and the pelvis contacts the support surface and weight is taken on the lower rib cage, elbows, and forearms. Head lifting includes head and upper trunk extension combined with glenohumeral flexion. This pattern of movement shifts the COM distally and provides a stable base, which allows the infant to lift and turn the head freely and easily. Along with this bio-mechanical change comes a shift in the weight-bearing surface from the shoulders to the lower trunk and legs, and a concurrent increase in muscle strength in the shoulder girdle. Fig. 14.1 (a) A 10-day-old infant in prone. Head lifting is constrained by flexed posture, weight forward on shoulder and face and the large mass of the head. (b) Changes in head lifting by 3 months of age correspond to increased extension in trunk, weight shift caudally, strength in neck and shoulders, interest and fixation with the eyes, and practice in a stimulating environment. Exceptions to the cephalocaudal–proximodistal progression have been described in the literature and suggest that many aspects of motor development undergo simultaneous development. Neural and body systems develop at different rates to share in the control of motor behavior, enhancing or constraining particular motor patterns at different times over the lifespan. Rate-limiting variables include muscle strength and length, postural control, perceptual capabilities, body morphology, experience, memory, and opportunity for object exploration and positional experience.28,29 For example, various investigators have shown that precision grasp and release are not used for functional skills until the infant develops stability of the head, trunk, and shoulder girdle between 4 and 5 months of age, even though complex precise finger movements and hand shaping for grasp are seen in infants as early as 1 month of age.30,31 This relationship suggests that proximal stability must develop to support distal control needed for function. In the example of head lifting described earlier, head control develops in prone as the load-bearing surface gradually shifts caudally, taking weight off the face and shoulders. This caudal shift allows the shoulder girdle muscles to strengthen and frees the arms for reaching and exploring. The rate limitation factors include the size of the child’s head (relative to the body), the amount of time spent in prone, and the level of interesting sounds and sights to motivate the infant to lift the head. In the first 3 months of life, motor skill development focuses on both movement and postural stability of the head. From 4 to 6 months of age, infants develop postural control and balance for sitting, which frees the hands for grasp and play. From 7 to 9 months of age infants gain control over the lower extremities and pelvis in the upright position, and the hands and arms are no longer needed for support. Finally between 10 and 12 months of age infants gain control in upright stance and overall postural control for further independent exploration. Refinement of all these skills continues through the early school years, with new skills developing as environments and opportunities for dance, skiing, and other athletics become available. The following outline uses the principle of directionality to list observable motor behaviors as they relate to body movement in and through space, as well as speech and fine motor skills. • Gains stable vertical head position. • Lifts and turns head in prone. • Engages in meaningful visual gaze. • Develops social smile. • Vocalizes with movement; begins cooing. • Swipes with arm and hand when supine; begins goal-directed reaching. • Pivots in prone. • Rolls supine to prone and prone to supine. • Plays with legs in air in supine. • Develops ability to sit alone (but cannot move into and out of sitting). • Frees hands in supine, prone, and sitting for manipulation of objects; poking with fingers. • Utters long repetitive sound sequences, varying pitch, intonation, and loudness. • Vocalizes pleasure or displeasure. • Coordinates arm and hand control with vision. • Mobility in prone; crawling, creeping. • Moves into and out of sitting. • Bounces in standing, pulls to stand; cruises. • Refines arms and hands for pointing, precise release, transfer hand to hand; finger feeding. • Produces long chains of combinations of vowel and consonant sounds—babbling. • Creeps with increased velocity. • Activates feet in transitions to sitting, creeping, and walking. • Takes first independent steps. • Walks with or without using arms for balance. • Refines manipulation based on size and shape of object and task or goal. • Holds and manipulates two different objects. • Produces first real words. • Uses jargon; engages others in conversation. MD is a complex progression based on (1) neural system organization, (2) perceiving and accommodating to environmental demands, (3) body changes that accompany growth, and (4) the interplay and continuity of development of various body systems. Directionality of development results from interactive functioning of internal systems that infants bring to the exploration of a task and the capacity to benefit from the environmental context. The question remains, What enhances or constrains this seemingly effortless and orderly progression? The progression from non–goal directed mobility to accurate and skilled movement is supported by principles of (1) variability, (2) competition of motor patterns, (3) development of postural control, and (4) links between the sensory and motor systems. The following sections examine each of these concepts and relate them to NDT practice. Variability is the capacity to link movement to intention and the ability to select from a wide repertoire of possible motor solutions the one most appropriate for a specific situation.32 Variability is the broad spectrum of motor behaviors that characterize every typically developing infant’s movement. Variability is seen in the spontaneous arm, leg, and head movement of newborns32,33 Fig. 14.2a, b and has been shown to be characteristic of early sitting,34 reaching,35,36 and independent walking.37 The role of variability in MD supports those NDT assumptions that focus on the dynamic nature and system interactions of MD. In 2010, several investigators described the variability in posture and movement as an essential element of both development and motor learning.20,21,38 Once thought to be a constraint on development, variability is described as a driving force, giving the infant and child nearly unlimited possibilities with which to explore the environment, relate to persons, and develop a repertoire of movement strategies to solve motor problems. Variability reflects adaptations to changes in the biomechanical properties of the growing musculoskeletal system, maturation of the nervous system, changes in the environmental conditions, and increasingly more effective solutions to task demands. In the infant developing typically, both the amount and the quality of variability change over time. Heineman et al21 stress that in the process of learning, the infant (and later child and adult) selects the most appropriate movement variation to allow increasingly complex skill. This capacity to select and match movement with the task goal is indicative of humans’ capacity for adaptive variability. In infants developing typically, both the amount and the quality of variability change. Some variability must decrease to lead to increased consistency in outcome, whereas variability in other parameters increases to boost flexibility in performance. For example, a decreased variability in postural control is needed for a child to gain stability in the upright posture and to be able to attend to tasks, accurately perform functional activities (e.g., speech and manipulation of objects), and use these functions in activities of daily living. On the other hand, an increase in variability in hand movements leads to the development of in-hand manipulation of a wide variety of objects. Grasping depends on the correct hand orientation and the ability to switch between power and precision grips. Think of the ability to pick up coins with the radial digits while holding additional coins in your hand with the ulnar digits. Von Hofsten and Rönnqvist39 presented evidence that neonates’ spontaneous arm movements show distinct patterns of spatiotemporal organization that have one acceleration and one deceleration phase similar to those that occur in the reaching patterns of 5-month-old infants. However, in the neonate, the movements of the two arms are strongly coupled in all three planes, moving together along the body’s longitudinal axis, abducting and adducting together, and extending together in the forward direction. By 4 months of age, the trajectory is irregular and fragmented as the infant experiments with single-limb reaching. In order for the movement to become straight and fluid, purposeful reaching and manipulation involve, at the very least, postural control; development of control of arm movements (kinematics) against the force of gravity; development of a flexible coupling in eye–head and hand coordination and coordination between the two hands; shaping and molding of the hand as a terminal device; interpreting exteroceptive, proprioceptive, and visual information; developing control of strength, velocity, timing for initiation, and braking; as well as experience, learning, and desire.35,39,40 Fig. 14.2 (a) This newborn shows variability in arm and hand posture. The arms are symmetrical with hands fisted asymmetrically. (b) The newborn also shows variability with the arms asymmetrically postured and the hands fisted symmetrically. Infants have complex variability in grasp patterns produced by multijoint actions, but this must change for the infant to develop precision involving subtle single-joint motions with infinite combinations. Generally, the hand shape depends on specific objects in the environmental context. The hand shapes itself around an object and accommodates its own shape to the shape of the object. To do this, the hand must be expandable and malleable, and patterns of grip must be sufficiently variable to shape around both large and small objects. At times, the hand needs to be powerful and at other times delicate in its approach to grasp and manipulation. The ability of the hand to be functional in all these situations depends on the balance between the long finger flexors and extensors, the capability for alignment between the wrist and hand, the mobility of the carpal and metacarpal bones, and the activity of the intrinsic muscles of the hand. These biomechanical contributions, including the kinetics and kinematics of the upper extremity (UE), play an important role in the development of reach and grasp. Compromise of any of these anatomical structures or intrinsic movement dynamics will constrain hand trajectory, joint coordination, and muscle activation patterns. Increased variability is a source of information for exploration, tool use, and other task-specific actions38 (Fig. 14.3a–c). NDT therapists appreciate individual variability in task solutions and recognize that when a person is gaining (or regaining) a skill, active problem solving involves trying out various solutions, some of which may seem awkward, inappropriate, and even counterproductive to the developmental process. Clinicians allow individuals to experiment and discover what works best for them within the parameters of their musculoskeletal and neuromuscular abilities and constraints. Therapists also recognize that there is a developmental process to variability with periods of organization, variability, and reorganization as new skill develops. With greater variability, less postural muscle activation is used to stabilize the person against gravity, and there is more activation of muscle groups that create precision movements. Therapists are, therefore, responsible for recognizing which components of posture and movement are needed for skill development and for guiding or limiting the individual’s experimentation in order for this process to occur in a timely manner to ensure optimal development or recovery. Lack of variability may be indicative of neuropathology in both full-term and preterm infants.41,42,43 Variability is inherent to human behavior and is needed for exploration and interactions; however, therapists need to recognize when variability serves the development of the child and when it constrains function so they can adjust intervention strategies to the need of the child at the moment. For example, a child with athetoid cerebral palsy has too much variability when attempting intentional movement. The excessive movement often includes muscles normally used for postural control so that posture is not sustained. NDT therapists develop intervention strategies that focus on slow movements in short ranges to allow postural muscles to be used to their physiological advantage in patterns of coactivation and support for function (see assumptions 6, 9, and 11 in Section 14.2 earlier in the chapter.) Closely linked to the principle of variability is the concept of competition in motor patterns. Kong and Quinton developed methods of early detection and described competition of motor patterns in infants developing typically as well as in infants with neuropathology.44,45 Like the principle of variability, this concept is supported by theories of motor control and the current literature on human development.21,38,46,47 Quinton describes three characteristics in normally competing movement patterns. First, one pattern of movement never dominates any other. For example, one instant a newborn may show asymmetry in the arms, and in another moment, show symmetry as shown in Fig. 14.4a, b.
14.1 Motor Development as a Lifelong Process
14.1.1 Changes in Thinking about Motor Development
14.2 NDT Assumptions in Motor Development
14.3 Contemporary Principles in Motor Development That Support NDT Practice
14.3.1 Stages of Motor Development
14.3.2 Directionality
Birth to 3 Months—Development of Functional Head Control
Four to 6 Months—Development of Upper Trunk Control
Six to 9 Months—Lower Trunk Control
Nine to 12 Months—Lower Extremity Control in Upright Position
14.3.3 What Supports the Progression of Motor Development?
Variability in Motor Development
How Does Variability Impact NDT Intervention?
Competition in Motor Patterns
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree