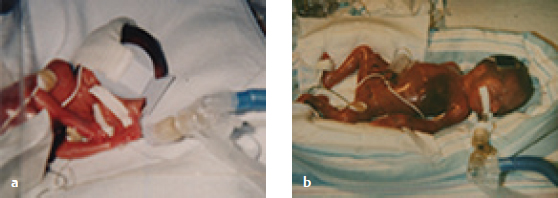
Case Report B8 Providing Ongoing Neuro-Developmental Treatment–Based Physical Therapy Intervention for a Medically Fragile Child with Severe Disabilities Physical therapists (PTs) who work with children see a wide spectrum of clients or students. Even if one considers the management of only those children with developmental disabilities or with cerebral palsy (CP), the scope of practice remains wide. The focus narrows substantially when considering the examination of and intervention for children with CP who are severely involved. These children represent a small number and are especially challenging for clinicians to manage. In trying to best prepare future therapists for the entire breadth of potential practice, professional educators tend to emphasize the most prevalent issues or those the clinician would be most likely to encounter. Because children with developmental disabilities who are severely involved represent such a small percentage of the total population, therapists may be less prepared to manage the special needs of this population. In addition, there is a general perception that therapy is less effective for individuals who are more severely involved because these children may be perceived as being unlikely to make marked progress. Therapists managing a busy case schedule may elect to and be directed to provide more intensive therapy for children who are more likely to make faster functional gains. Brandon is one child who is included in this group of children who are more severely involved. Brandon and his twin, Blake, were born at 25 weeks’ gestation (Fig. B8.1a, b). Initially, Brandon was the healthier of the twins and was discharged from the neonatal intensive care unit (NICU) after 4 months. However, after a short stay at home, he demonstrated increasing difficulties and was admitted to the pediatric intensive care unit (PICU) for a month and a half. Both he and his brother were diagnosed as having CP, although Brandon had more significant impairments and activity limitations than did Blake. During this second hospital stay, the family was advised to consider halting intensive medical intervention because the predicted outcome for Brandon was bleak. The family decided this was not an option for Brandon. They took Brandon home with his brother and started the journey as a family. This case report describes Brandon as a child with severe involvement within the framework of the International Classification of Functioning, Disability and Health—Version for Children and Youth (ICF-CY).1 The case report thus offers therapists an example of how a Neuro-Developmental Treatment (NDT) framework was used specifically to improve the participation domain for a child functioning within level V of the Gross Motor Function Classification System (GMFCS).2,3,4 Intervention focused on improving Brandon’s participation in his home and community and included both the careful selection of adaptive equipment and assistive technology and direct hands-on intervention within the NDT Practice Model. In the definitions of CP,5,6,7,8 the effects of the posture and movement disorder are anticipated to be present throughout life, but the impairments and their influences on functional activity and participation are changeable across that lifetime. Although CP is viewed as a chronic condition, currently, it is usually not viewed as one that will significantly alter the length of life. The life span of individuals with CP is now approaching a typical length unless one includes those that are severely involved.9,10,11 Hutton12,13 reported that a 2-year-old with severe CP has an ~40% chance of living to age 20 as compared with a child with mild CP, who would have a 99% chance. The most frequently reported causes of death include respiratory diseases, epilepsy, and congenital malformations.13 Additionally, there are several factors associated with a shorter life span, including the number of impairments, the overall severity level, mobility restrictions, feeding difficulties, seizures, lower cognitive function, decreased visual acuity, quadriplegia, and impaired respiratory function.14 In a review paper by Imms et al15 in 2008, it was reported that all children with CP were found to have more restricted participation diversity and intensity as compared with children without disabilities. These findings were confirmed in more current reports.16,17,18 Children who are severely involved GMFCS2,3,4 level V are found to have the most restricted participation, with activities being performed either individually or with the extended family, rather than being community based.15,16 The level and intensity of participation are determined by a combination of multiple contextual factors, including the specific child’s characteristics, family characteristics, education, and health care and community services.16,17,18,19,20,21,22 Overall, the child’s gross motor function and adaptive behavior are important factors in determining participation.21 Knowledge of the child’s preferences also has a role in the selection of appropriate opportunities for participation.17 Finally, environmental modifications and assistive technology are important considerations in enabling participation of children with CP.22 Therapists who work with individuals who are more severely involved must take these factors into account because a prime role of intervention is to improve participation. The therapist should include a careful review of individual and environmental contextual factors, gross motor skills, and development of adaptive skills that would support participation in the data collection, examination, evaluation, and plan of care. Environmental factors should include a review of the availability and use of adaptive equipment and assistive technology. This process is well imbedded in the NDT Practice Model. Children who are severely involved are identified by the significant activity limitations in many areas of daily life function. Activity is currently classified as related specifically to the GMFCS,2,3,4 the Manual Ability Classification System (MACS),23,24 and the Communication Function Classification System (CFCS)25 skills. In all three systems, level V would include the description of children with severe activity limitations. The skills are summarized in Table B8.1. After the birth of a child with special needs, the parents are faced with raising a child without specialized training. Typically, parents anticipate sharing in the development of motor milestones, such as rolling over, sitting, walking, running, bicycling, or maybe even the Olympics. Instead, parents of children who are severely involved observe their child struggling to achieve even basic skills. Strategies to teach motor skills employed with siblings are not effective in improving the desired skills. If referred for physical therapy and asked what their goals are for their child in therapy, those parents usually answer, “I want my child to walk.” The parent may not have any idea of what is actually possible. Often parents at the time of diagnosis report that physicians stress what is not likely or possible to occur for their child. The parent may be clinging to the hopes and dreams of all parents for their children. However, the more realistically achievable gross motor skills may be that these children will sit safely in a car seat, that they will do a standing transfer from the wheelchair to the bed, or that they will take a few supported steps with the assist of a caregiver. These are not activities that parents routinely include in goal statements nor are they routinely included in standardized lists of developmental milestones. They are, however, activities that can dramatically alter participation for both a child with severe involvement and that child’s entire family. Table B8.1 Classifications of function: level V descriptors
B8.1 Introduction
B8.2 Review of the Literature
B8.2.1 Who Is the Child with CP Who Is Severely Involved?
Social Function: Participation and Participation Restrictions
Individual Function Activity and Activity Limitation
B8.3 The Family with a Child with Severe Developmental Disabilities
Functional classification system | Classification description |
Gross Motor Function Classification System (GMFCS) level V | Physical impairments restrict voluntary control of movement and the ability to maintain antigravity head and trunk postures. All areas of motor function are limited. Functional limitations in sitting and standing are not fully compensated for through the use of adaptive equipment and assistive technology. At level V, children have no means of independent mobility and are transported. Some children achieve self-mobility using a power wheelchair with extensive adaptations.2,3,4 |
Manual Ability Classification System (MACS) level V | Does not handle objects and has severely limited ability to perform even simple actions. Requires total assistance.24 |
Communication Function Classification System (CFCS) level V | Seldom effective sender and receiver, even with familiar partners. The person is limited as both a sender and a receiver. The person’s communication is difficult for most people to understand. The person appears to have limited understanding of messages from most people. Communication is seldom effective, even with familiar partners.25 |
B8.4 Case Description
Brandon spent the initial months of his life in an NICU. Initially, he was the healthier of the twins and was discharged from the NICU after 4 months. However, after a short stay at home, he demonstrated increasing difficulties and was readmitted to the PICU for a month and a half. (See photos in photo gallery in the NICU file on Thieme MediaCenter.) This case report will be presented from age 2, when Brandon and his family moved to the therapist’s geographic area, and will follow him to the end of his life at age 10. The ICF-CY1 model will be used to organize the clinical description for Brandon. The description begins with the domain of social function, transition to individual function domain, and finish with the body structure and function domain. Finally, the influences from the environmental and personal contextual factors are discussed, with the overarching influences on all of the domains.
The domains and contextual factors are explored in three different time frames. The first frame includes the early years for Brandon and Blake, when the care was more like baby care. Although the two boys were different, both boys needed to be carried, positioned, fed, diapered, and so forth. The second frame is the early school years. Brandon was attending school, but the differences in abilities and participation were more evident, not only between same-age peers but also with his twin. The final frame explores when Brandon became more medically fragile such that what separated him from his brother as well as his peers was more medically based rather than activity or participation based.
B8.4.1 Medical Diagnoses
Brandon’s diagnoses (listed in approximately chronological order) include intraventricular hemorrhage (IVH, bilateral grade IV), bronchopulmonary dysplasia (BPD), retinopathy of prematurity (ROP, stage III+; resolved), hydrocephalus, CP, cortical visual impairment, severe mental retardation, seizure disorder, oral motor dysfunction, gastroesophageal reflux disease (GERD), chronic sinusitis, chronic pneumonia, hypothyroidism/hypoadrenalism, scoliosis, gastrostomy tube (G-tube) for all nutrition, osteopenia, and bilateral hip dysplasia.
B8.4.2 Examination
Social Function—Participation and Participation Restrictions
Brandon was always a full participant in family life. Once living at home, he shared a bedroom with his twin and slept at the same hours. As he became more medically fragile, he was moved into his own bedroom because his sleep and wake cycles were less consistent. His room was centrally located so that he could be a part of family life, and it was spacious enough to accommodate all of his equipment. His bedroom looked like a boy’s bedroom rather than a hospital room. Brandon’s family moved twice to better accommodate his needs in the home and to support his inclusion in family life. The family had meals together throughout Brandon’s life, even though Brandon was fed by a G-tube. They enjoyed music and had regular video nights at home. Brandon participated in all of these activities, whether in his wheelchair, his special activity chair in the family room, his stander, or in one of his parents’ arms.
Brandon and his brothers liked to play together, especially when he was upright in his chairs or stander. Brandon liked to shake bells secured to his wrist and did it best in supported standing. He and his brother would dance together in this fashion. His family life did change significantly when he was 5 years old with the addition of a younger brother. He had to learn to share his parents’ attention even more, to play with someone younger than himself, to wait for short periods, and to take turns. His home environment was now more active and complex.
Brandon’s participation with the family expanded to include his extended family. He loved visits of his grandparents and liked to be held and pampered by them. He could sleep, eat, and play in his home with the assistance of his grandparents while the parents had some respite from the constant care of Brandon and Blake. He also learned to be cared for by in-home nurses and adjusted to having a series of less familiar adults assist him with all activities of daily living (ADLs). He had preferences of who could assist him, but he did participate with this wider group of caregivers. In his final days and hours of life, he returned to being held in the arms of his parents, where he had always experienced the least discomfort and the best possible breathing, and where he did what he did best, which was to love and to be loved. See photos in the galleries “I am a Twin,” “I am a Unique Person,” and “I am a Family Member” on Thieme MediaCenter.
Brandon initially attended a public preschool for children with special needs and then an elementary school in a self-contained class for children with severe and profound physical and cognitive impairments. He attended the same school as his brother for the initial years. It was not the neighborhood school, making it more difficult to build a convenient group of friends nearby. As the differences between Brandon and Blake’s educational needs widened, the boys attended different schools. Neither Brandon nor Blake could ride the regular school bus. Their mother chose to drive Brandon to school because it was difficult to position him safely in his chair for the long rides without her watchful eye. By 8 years of age, his health eventually prevented him from attending school, even in a small self-contained class, so educational services were provided on a homebound basis with a teacher coming in on a weekly basis.
Brandon initially participated in early intervention with home-based occupational therapy, physical therapy, and speech-language pathology services. His parents selected to have clinic-based outpatient therapy services where therapists were more familiar with a medical model required for his care and directed toward meeting his specific needs. At age 2, he began out-patient therapy services when his health permitted. He also attended frequent medical visits with a wide range of specialists, in both Augusta and Atlanta, Georgia. He lived at home whenever care could be provided there, even when it required multiple hours of home health nursing care. He required multiple trips to the hospital, however, for stays varying from several days to a month at a time. Hospitalizations were based on respiratory infections, one cardiac arrest, severe gastrointestinal (GI) problems, and several episodes of infections that were difficult to diagnose and treat. Most visits entailed PICU stays, with an occasional stay on the regular pediatric floor. As time progressed, the home environment was adapted to provide most of the needed medical equipment and supplies of a hospital room, and Brandon’s mother and regular in-home nurses were able to provide closer supervision. Brandon’s mother was also better able to detect and respond to his signs of distress or recovery compared with unfamiliar hospital staff. The entire family dynamics changed when Brandon was in the hospital. Blake especially missed his brother and would at times report that he had some unnoticed medical problem that required a trip to the hospital.
Individual Function—Activity and Activity Limitations
Brandon’s functional activities varied based on his health. He could usually reposition himself by rolling when uncomfortable if positioned in prone, supine, or side lying. He could, at different points in his life span, sit independently, either in a modified long sit position or in supported bench sitting with upper extremity (UE) support, and he enjoyed sitting in a wide variety of chairs outside his wheelchair. He also, at times, could assist with standing transfers between these chairs or when preparing to be picked up and carried if supported by a caregiver and when wearing his ankle-foot orthoses (AFOs). He could usually stand with support of his stander, a partial body-weight-bearing device (PBWB), or an adult to watch videos or play with his brother. He could take some assisted steps during his healthier periods. These skills would improve as his health did and then disappear for periods after each hospitalization or when his oxygen saturations remained very low. His desire to accomplish daily tasks never decreased, and he worked hard each time after a medical crisis to regain those skills.
Body Structure and Function: Integrities and Impairments
Multisystem Issues Related to Posture and Movement
Brandon required support in all antigravity postures. He could lie independently in prone, supine, or side lying but required support for sitting and standing. As a pre-schooler, he could roll quickly from prone to supine and developed head control for sitting and standing for short periods of time. In all postures, Brandon always assumed a large base of support and was asymmetrical. His head was usually rotated and laterally flexed to the right and hyperextended. He had a significant scoliosis. Surgical spinal stabilization corrected this spinal asymmetry and made sitting far easier for him. His extremities also demonstrated the asymmetry, the lower extremities (LEs) more so than the UEs.
He had a paucity of movement, especially when his O2 saturation levels (SaO2) were low. He tended to move in full flexion or extension, but the range of movement was altered by his surgeries. When feeling well, he could demonstrate reciprocal flexion and extension in the LEs and could reach with either arm. He could move his extremities but had difficulty after each surgery developing the control necessary to manage the new situation (e.g., the hip control in both sitting and standing after an osteotomy). He had the freest movement when supported in the PBWB.
Single-System Integrities and Impairments
Brandon had many system impairments that varied across time. For each system, a general status will be given along with trends across time for that system. The constant changes in different systems’ status, the interaction between the body systems and posture and movement impairments, and the influence of all of this on his functional activity were challenging for the PT to analyze and to make the necessary shifts in his plan of care and intervention.
Regulatory System
At age 2, Brandon had difficulty with temperature control and could not go outside on very hot days. He had increased redness across the extremities and would also suddenly flush. His heart rate and SaO2 levels demonstrated sporadic changes not based on activity or observable environmental stresses, reflecting poor central regulation of basic physiological systems. He always required more sleep than his brother and always had difficulty with constipation. He was initially more irritable than his brother, and if something went wrong in the day, the entire day could be a bad day.
By age 9, Brandon could demonstrate a wider variety of states. He could be happy, quiet, fussy, or angry. Changes in status were often related to SaO2 levels. He wore a monitor at all times that sounded when his O2 levels were below 85%. His heart rate fluctuated. He took melatonin as needed to aid in sleep.
Respiratory System
Brandon demonstrated greater impairments in the respiratory system with chronic pneumonia. He first required supplemental O2 at night for sleep apnea and eventually the use of O2 throughout most of the day. The spinal stabilization also immediately improved his SaO2 levels. He eventually required a tracheostomy and required ventilation on several hospital stays. His baseline SaO2 gradually dropped and was monitored constantly. After the tracheostomy, the shifts in SaO2 were not significantly altered by changes in postures, allowing him to be positioned safely in prone, supine, sitting, or standing. He had ongoing difficulties with congestion and upper airway infections. He developed severe sinusitis. He frequently stopped breathing altogether during seizures, yet the physicians had difficulty with balancing sufficient seizure medication to control his seizures and maintain adequate O2 levels because the medication also tended to decrease his respiratory drive.
His breathing pattern was primarily diaphragmatic without full expansion of the rib cage. Medications for the respiratory system included Singulair (Merck Sharp and Dohme Corp.), Nasonex (Merck Sharp & Dohme Corp.), Pulmicort (AstraZeneca), albuterol, Atrovent (Boehringer Ingelheim), and Clarinex (Merck Sharp & Dohme Corp.) daily. In addition, he took tobramycin and Septra (Pfizer, Inc.) to address the chronic respiratory infections.
Cardiovascular System
During the later stages of Brandon’s life, his heart rate was also monitored constantly by the oxygen monitors. His heart rate varied from the 40 bpm range when he was asleep to between 60 and 80 bpm when he was awake and alert, but it did occasionally jump to the mid to upper 90s. He did have one cardiac arrest during a long seizure when he was 8 years old.
Neuromuscular System
Brandon could initiate, sustain, and terminate motor unit activity but had difficulty with the control/gradation of muscle activation and the coordination or timing and sequencing of muscle activation for functional activities. He initially had the greatest difficulty in terminating motor unit activity and would depend on a caregiver or changes in the environment to inhibit muscle activation. Most often, the muscle activation was isometric or concentric in nature with almost no eccentric control demonstrated. He also demonstrated a restricted number of synergies for function, with limitations in isolated control. He moved in full patterns of flexion and extension or if his head was positioned more asymmetrically—one side of his body in full flexion and the contralateral side in extension.
His overall dynamic stiffness varied from being low to very high. The changes were based on intrinsic changes in physiological status as well as from changes in the environment. He demonstrated very low levels of stiffness and was more flail when his oxygen levels were the lowest. He demonstrated clonus more so in the left LE than in the UEs. At times, however, he could demonstrate clonus throughout both LEs, both UEs, and even at the jaw.
Brandon had multiple medical interventions that addressed his neuromuscular system with eight sets of Botox (Allergan) or phenol injections to the hamstrings, adductors, and gastrocnemius, as well as to the pectorals, sternocleidomastoid, and latissimus dorsi. He had a baclofen pump trial but did not have a pump inserted, so he took oral baclofen daily. His seizure medications included phenobarbital, Trileptal (Novartis), Keppra (UCB), and Diastat (Valeant Pharmaceuticals North America) as needed for uncontrolled seizures. These medications also influenced his neuromuscular status.
Musculoskeletal System
Skeletal deformities include leg length discrepancy with the left ~1 in shorter than the right. The legs also demonstrated asymmetry in circumferences, with the left calf being a quarter inch bigger than the right and the left thigh being 2 in smaller than the right. As mentioned previously, he developed a scoliosis that was surgically stabilized. He had right hip dysplasia with surgical correction. He had severe forefoot varus on the left. He had severe osteopoenia with a fracture of his left distal femur with titanium rod implantation and later removal. He had marked limitations in range of motion (ROM) in both the UEs and the LEs and had significant weakness in all four limbs.
Integumentary System
His skin overall was fine and fragile. This fragility was true particularly in his hands and feet and was perhaps related to impaired distal circulation. His compromised skin integrity made it more difficult to wear orthoses successfully and required ongoing modifications of fit and careful monitoring within the day and across time.
Gastrointestinal System
Brandon had severe GERD with subsequent G-tube placement and a Nissan procedure within the first months of life. Even after the Nissan procedure, vomiting of meals was common. Brandon had difficulties with drooling and with constipation that were related to intrinsic impairments as well as being associated with his medications for other body system issues. His medications for his GI system included Reglan (Baxter Pharmaceutical), Robinul (Caspar Pharmaceuticals), MiraLAX (Bayer), Prevacid (Takeda Pharmaceuticals USA, Inc.), and vitamin B complex drops.
Sensory Systems
Although Brandon was reported to have cortical visual impairments, he did see many things in his environment. His ability to focus or track items changed based on his health status. Brandon had good hearing. He loved vestibular input, and his swing was his favorite way to get that input. Brandon loved tactile input, including deep pressure, particularly with cuddling, and he enjoyed moving tactile input.
Contextual Factors—the Family, Health Care System, Schools, Equipment, and Brandon’s Health as an Individual
The family preferred country living and being outdoors. Brandon had excellent support of his family. When Brandon was 3 years old, the family moved to another state for better employment for the father, but the family found that they could not find adequate therapy services for Brandon and Blake, so they returned to the previous state to obtain those services.
It was stressful for the family to have two boys with very different special needs. Blake was ambulatory by age 2 but had a diplegia with a marked asymmetry. He had sensory impairments with difficulty attending to tasks and had been identified as being on the autism spectrum. The younger brother also had some health concerns with a cardiac defect that resolved spontaneously.
The parents were the foundation of the family. The stresses on a marriage of having a single child born prematurely and then raising that child with special needs are well documented.25,26 In this family’s case, the stress was multiplied with twins, both with disabilities. In addition, one child had multiple medical crises and the need for ongoing intensive medical care in the home. Brandon’s dad managed the roles of being the bread winner, a father, a spouse, and the caregiver for any one of the children at times.
Brandon’s mother was the day to day, minute to minute manager for the family. She did all the jobs of every mother, with cooking, cleaning, feeding, dressing, bathing, playing, teaching, as well as driving to two different schools, to therapies, to medical appointments; coordinating the array of professionals who provided care for the boys; loading and unloading equipment; using adaptive equipment; monitoring that equipment; and then making suggestions as to how it could work better for her child. She even stayed in the hospital during Brandon’s stays. Brandon’s mother responded to the challenges and stresses by educating herself and completing nursing school.
Brandon’s extended family is also strong, with the grandparents supporting the parents during difficult hospitalizations as well as in good or healthy times to allow some respite. The family lived in a town with a major children’s medical center with the availability of most of the medical specialists required for Brandon’s care. Brandon’s family had good insurance through the father’s work. Brandon’s case manager through the insurance company worked well with the health care providers and streamlined the process for prior authorizations for his care as outlined in the family’s policy. In addition, Brandon qualified for Medicaid in the state as a secondary form of insurance.
Brandon’s family and health care team obtained necessary medical and adaptive equipment. The following is a list of equipment Brandon used in October 2009:
• Adjustable protective bed.
• Adapted car seat.
• Adapted toilet seat.
• Adapted vestibular swing.
• Bath bench.
• Bilateral solid AFOs.
• Continuous positive airway pressure (CPAP) machine.
• Chest physical therapy.
• Feeding pump.
• Knee immobilizers.
• Monitor for SaO2 and heart rate.
• Nebulizer.
• Oxygen concentrator.
• Positioning activity chair.
• Standing, Walking, and Sitting Hip Orthosis (SWASH).
• Supine stander.
• Thoracic-lumbar-sacral orthosis (TLSO)
• Wheelchair.
Brandon’s medications are summarized in Table B8.2.
Table B8.2 Summary of medications from October 2009
Medication | Dose | Schedule |
Phenobarbital | 20 mg/5mL | 5 mL twice a day |
Baclofen | 10 mg tablet | One tablet 3 times/d |
Reglan (Baxter Pharmaceutical) | 5 mg/5 mL | 4 mL 4 times/d |
Trileptal (Novartis) | 300 mg/5mL | 7.5 mL every morning and 8 mL every evening |
Keppra (UCB) | 100 mg/1mL | 6 mL twice a day |
Singulair (Merck Sharp & Dohme Corp.) | 5 mg tablet | 1 tablet daily |
MiraLAX (Bayer) |
| 1 capful every other day (MWF) |
Robinul (Caspar Pharmaceuticals) | 1 mg tablet | 1 tablet 3 times/d |
Nasonex (Merck Sharp & Dohme Corp.) |
| 2 puffs each nare twice a day |
Melatonin | 1 mg tablet | 1–2 tablets hours of sleep as needed |
Prevacid (Takeda Pharmaceuticals USA, Inc.) | 30 mg solutab | Once daily |
Pulmicort (AstraZeneca) | 0.5 mg/2 mL | 2.5 mL 3 times/d via jet nebulizer |
Albuterol | 2.5 mg/3 mL | 3 mL 4 times/d via jet nebulizer |
Atrovent (Boehringer Ingelheim) | 5 mg/2.5 mL | 5 mL 3 times/d via jet nebulizer |
Clarinex (Merck Sharp & Dohme Corp.) | 5 mg/2 mL | 5 mL daily |
Diastat (Valeant Pharmaceutials North America) | 5 mg | As needed |
Ciprodex (Alcon) |
| 4 drops in affected ear twice a day as needed |
Cortef (Pfizer) | 5 mg tablet | 1 tablet every morning and ½ tablet every evening and stress dose 3 tablets every 8 h as needed for fever/vomiting |
Synthroid (AbbVie) | 125 μg tablet | ½ tablet daily |
Ketoconazole shampoo | 2% | Use 2 times/wk |
Vitamin B complex drops |
| 1 mL daily |
Tobramycin | 40 mg/mL vial | Give 80 mg by inhalation twice a day for 30 days, then 30 days off |
Septra (Pfizer, Inc.) |
| 15 mL every day |
Nutrition | 6 oz PediaSure (Abbott) with fiber flushed with 15 mL of water | Give 4 times/d in 4 h intervals during daytime only |
B8.4.3 Evaluation Summary
The analysis of the data gathered from annual examinations varied. As Brandon grew, the desired participation and activity outcomes changed. Brandon’s parents were critical in selecting outcomes around which intervention focused. Across the years during his annual evaluations, the parents consistently stated that they wanted one focus to be on sitting for a variety of functions as well as wanting him to stand and take assisted steps. There were, however, also time frames in which the family said that they had no idea as to what was possible due to the multitude of medical complications. The therapist educated the family as to what might be important skills to develop for the future and what were potential future complications that could occur based on Brandon’s overall status.
As Brandon’s health changed, the relative importance of each impairment changed. Initially, the family focused on outcomes that were more developmentally age appropriate. He learned to roll and to inch forward on the floor in a commando-style crawl.
The following is a summary of outcomes from his annual evaluations and the associated intervention objectives related to the highest-priority impairments.
• By age 2 to 3 years, the family wanted him to be able to sit and hoped for some form of ambulation, even if it was with assistance.
Therefore, the outcomes for the years when Brandon was 2 and 3 years old were that he would be able to do the following:
 Sit on the floor in either long or tailor sitting consistently for 20 seconds for play at home.
Sit on the floor in either long or tailor sitting consistently for 20 seconds for play at home.
 Bench sit with elbows propping on a tabletop surface for 45 seconds at a time for educational activities and to watch videos or his brother at play.
Bench sit with elbows propping on a tabletop surface for 45 seconds at a time for educational activities and to watch videos or his brother at play.
 Transfer from his wheelchair to other chairs with assistance of an adult to UEs and trunk but not LEs while wearing AFOs.
Transfer from his wheelchair to other chairs with assistance of an adult to UEs and trunk but not LEs while wearing AFOs.
• By age 4, the outcomes were expanded to include the following abilities:
 Sit for longer episodes (up to a minute at a time).
Sit for longer episodes (up to a minute at a time).
 Transfer with assist of an adult to only the pelvis.
Transfer with assist of an adult to only the pelvis.
 Stand with support of a surface while engaging in UE play.
Stand with support of a surface while engaging in UE play.
 Take 50 steps with assistance of an anterior support walker with support of the therapist at the pelvis.
Take 50 steps with assistance of an anterior support walker with support of the therapist at the pelvis.
• By age 5, the outcomes were that Brandon would be able to do the following:
 Sit without support for 3-plus minutes at a time to watch a video or listen to a song.
Sit without support for 3-plus minutes at a time to watch a video or listen to a song.
 Walk 10 feet in a PBWB system, advancing the limbs independently but with the adult controlling the speed and directionality of the movement of the device.
Walk 10 feet in a PBWB system, advancing the limbs independently but with the adult controlling the speed and directionality of the movement of the device.
 Transfer between chairs of uneven heights.
Transfer between chairs of uneven heights.
 Roll independently to cross a room for play.
Roll independently to cross a room for play.
• For the first time, when Brandon was 8 years old, the functional outcomes began to include qualifiers concerning SaO2. However, they kept a focus on skills in transferring, sitting, rolling, and assisted walking. They included Brandon being able to do the following:
 Transfer through stand pivot with assist of adult.
Transfer through stand pivot with assist of adult.
 Take five assisted steps in suspension-style walker.
Take five assisted steps in suspension-style walker.
 Reposition himself in prone, side lying, or supine to improve respiratory pattern, SaO2, or comfort level.
Reposition himself in prone, side lying, or supine to improve respiratory pattern, SaO2, or comfort level.
 Participate at home or at school in at least six different positions.
Participate at home or at school in at least six different positions.
• By age 9, the outcomes included being able to do the following:
 Sit on a bench with support of a small table to his arms for 10 minutes with supervision for play with a family member.
Sit on a bench with support of a small table to his arms for 10 minutes with supervision for play with a family member.
 Stand in stander for 30-minute episodes to complete a single educational activity.
Stand in stander for 30-minute episodes to complete a single educational activity.
 Take 10 assisted steps in a PBWB device with SaO2 remaining above 90%.
Take 10 assisted steps in a PBWB device with SaO2 remaining above 90%.
In order for Brandon to reach these outcomes, impairment related objectives were identified during each evaluation. Initially (age 2–3), the highest-priority objectives included that Brandon would need increased ROM in the LEs, increased dissociation between the trunk/pelvis/LEs, and increased dissociation between and within the LEs. It was also noted that Brandon would need more active rotation in the trunk and neck and would need increased strength and control in the LEs to meet the established outcomes.
When Brandon was 4 years old, the list of objectives expanded to include more consistent recruitment of the postural muscles of the trunk and neck with the continued emphasis on increasing isolated control in the trunk and extremities and on increasing soft tissue length and strength of the muscles.
By age 5 years, the impairment-related objectives included increasing postural holding through the head and trunk, increasing isolated control between trunk and extremities, increasing ability to perform lateral weight shifts through the lower body, increasing strength through all extremities and the trunk, increasing soft tissue mobility, and increasing symmetry.
At age 8 and 9 years, the plan of care also included mention of increased chest expansion during respiration, an increase in body symmetry, and increased respiratory support for gross motor function.
It is possible to track the therapist’s problem-solving process relating impairments to activity limitations and subsequently to the individual’s participation restrictions. The evaluation of Brandon not only outlines the relationships between the different domains but also lays the foundation of the individualized intervention plan.
B8.4.4 Intervention
The intervention process with Brandon across the years was modified to meet his ongoing changes in medical status. The therapist used the NDT problem-solving process and Practice Model at every step of the intervention course. As reported in the literature, the participation of a child with severe involvement is heavily influenced by the child’s gross motor functional abilities as well as the child’s preferences.15,16,17,18,19,20,21 For this report, two specific aspects of intervention across the years will be presented. The first is related to sitting with support for functional activities and participation, and the second focuses on working in supported standing again for increased activity and participation. Both examples include a review of problem solving related to the selection of adaptive equipment for use in the home and community as well as the specific intervention strategies that were used to address impairments within functional contexts.
Supported Sitting
The ability to sit independently or with support has been identified as a critical component for success in a wide variety of functional activities as well as increasing the participation of the individuals.16,17,18,19,20,21,22 For Brandon, sitting was important for many activities and participation. Brandon had episodes when he could sit independently for minutes at a time for play or interaction with others. However, he more often sat with support for activities and participation at home for family activities, such as for meals, birthday parties, play, and recreation, and for many of his medical treatments, as well as for loving and cuddling (see photos on Thieme MediaCenter). As expected, Brandon’s respiratory status was better in upright positioning, such as sitting, than in supine.27,28,29,30 Thus he frequently slept in supported sitting. He also needed to be in a more upright posture during meals and for at least an hour after his meals due to his reflux.
As he grew, gained weight, and was too big to be carried places, he was transported in sitting in a wheelchair. He had to be able to sit to ride in the family vehicle for trips to school (when he was able to attend), to his medical appointments, to therapy sessions, to participate in family errands such as taking his brothers to and from school, and for long rides for vacations or to visit his grandparents. He sat to participate in family activities, such as video night, to play with his dad on vacation in the surf, and to swing outside in an adaptive swing. He sat in his parents’ laps to be cuddled and hugged and for play.
His adapted activity chair was such a part of family life that 2 years after his death, it still remains in the family room and is used by his siblings for the same activities for which Brandon used it. He sat at school for learning. Initially for school, he needed to be able to sit safely on a school bus as well as in chairs within the school setting.
From this long list, it is clear that supported sitting was important for Brandon. One of the challenges for the therapist was then to determine what made it so difficult for Brandon to achieve this skill. What were the impairments that contributed to the difficulties? What recommendations could be made concerning the selection and use of adaptive seating to improve function and participation? What could the therapist do to address the impairments in terms of hands-on intervention and suggestions for home management or carryover?
Brandon’s adaptive equipment related specifically to sitting for participation or activity and included a wheel-chair, car seat, bath seat, swing, and activity chair. His wheelchairs were custom designed to increase participation and activity and to both address current impairments and minimize chances for future secondary impairments. As Brandon grew and new chairs were required, the decision-making process changed. Decisions were based on what had worked well in the previous chair, what progress had been achieved, what had not worked well, and what new challenges were being encountered. The team involved in the problem solving included the parents and grandparents, the seating specialist from the durable medical equipment supplier, the physical and occupational therapist, the physician, and the case manager. Each chair ordered required a careful assessment and teamwork to make the best choice. The wheelchair selected had a bright orange frame—Brandon’s favorite color and one of the parents’ school colors. The family had lots of Auburn accessories, including blankets, jackets, and pillows, matching the chair and encouraging interactions with a variety of people in the community. This strategy served to increase Brandon’s inclusion in conversations in many settings. Brandon was naturally handsome, but these additions made him more approachable for people who did not know how to approach or talk with a child who is severely involved and in a wheelchair.
Table B8.3 contains the list and rationale for the customized components in Brandon’s chair.
Table B8.3 Brandon’s wheelchair with rationale for each component
Chair component | Rationale |
Tilt-in-space | A tilt-in-space chair was selected to aid in positioning throughout the day. |
Impairment-related decisions: | |
• The tilt mechanism was necessary due to the respiratory and digestive impairments and his seizure disorder. Brandon’s SaO2 dropped during and after seizure activity. He demonstrated postictal lethargy for several hours and needed to be reclined for sleep. | |
• He frequently had better SaO2 when upright and also avoided problems secondary to severe reflux when more upright. | |
• When positioned well in the chair, Brandon did not have the ability to relieve pressure, and the tilt provided options to avoid skin breakdown. | |
• The tilt also reduced the postural demands of sitting. | |
Participation-related decisions: | |
• Brandon could sit upright for short times, but his appointments and trips into the community often exceeded his endurance. The tilt option allowed longer outings. | |
• The tilt range was also shifted such that the chair could tilt forward by 10–15° to assist in transferring in and out of the chair. The option allowed a wider variety of caregivers strategies to better position his body in the chair and to assist Brandon in standing transfers. | |
• This modification allowed him to tilt forward or backward sufficiently to relieve pressure and to assist in ADLs, such as dressing while in the chair. | |
• The seat cushion included special foam to allow padding and yet be firm enough for positioning of his LEs. | |
• Brandon’s legs were asymmetrical in length and in positioning. The seat cushion was shorter on the left than the right. | |
• The cushion had troughs to help keep the limbs in more neutral abduction/adduction and toward neutral rotation. | |
• The cushion prevented asymmetrical abnormal pressure over the ischial seats and across the area of the greater trochanters that were more prominent after the osteotomies. | |
• Due to the severe osteopenia, the legs needed to be padded to prevent bumps during transport. | |
• The seat back was a slightly rounded back to help position the trunk in midline over the pelvis. Once the spine had been stabilized, he did not require a molded cushion back as he did not demonstrate marked rotational deformity related to the scoliosis. | |
Lateral pads | • Even after his spinal stabilization, Brandon required bilateral trunk pads to position the upper body over the pelvis. |
• The pelvis could be positioned almost in midline, but there was a tendency for Brandon to lean to the side and to laterally flex the neck to his right with the head flexed forward toward the chest. | |
• The lateral pads helped to keep the thoracic spine near midline and therefore to keep the head more in midline. | |
Pelvic stabilizer | • The pelvic stabilizer (seat belt) was modified to meet his specific needs. A wide neoprene strap that was the width of his femurs was selected. This style belt instead of a narrower car seat style belt spread any pressure exerted on the femurs out across more area. |
• It also increased the sensory input to the femurs against the seat cushion as being the base of support rather than having Brandon pull into greater thoracic flexion to provide a sense of stability. | |
• All the stabilizing straps had to be quick release as Brandon had seizures that interfered with respirations, and it was important that he be able to be lifted from the chair quickly. | |
Dynamic harness | Brandon typically pulled his upper body into full flexion when positioned in sitting. Part of this tendency was due to the difficulty the Brandon had in isolating motion from one body part to another. When Brandon flexed at the hips and knees and ankles, as happens in sitting, his trunk also pulled into flexion with the rectus abdominis and pectorals pulling him forward. With the positioning in the chair, Brandon required increased input to hold the upper body into greater extension. A wider harness that crossed the shoulders to assist in positioning the scapulae in slight adduction and to gain some depression of the shoulder girdle was used. A wide variety of harnesses were tried as is seen by watching his chairs across the years. |
Collar | The positioning of the trunk via the seat cushion and back, scoliosis pads, pelvic stabilizer, harness, and the head support were not sufficient to keep Brandon’s head from pulling forward, down, and laterally such that it could be trapped to the side of the support. A collar assisted more directly to depress the shoulders and keep the top of the spine against the seat back. The neck could also be held more in midline and decrease the increasing impact of the spinal asymmetry and the pelvic girdle. |
Head support | Brandon had tried more head supports than any other component of the chair. None of them worked entirely well. Brandon moved his head forward into flexion and then laterally flexed it to the side and would also extend the neck asymmetrically from this posture. |
Chin roll | A chin roll was added for a period of ~18 months. This roll was used to block the pull of the head into forward flexion and subsequent lateral flexion and asymmetrical extension or chin jutting. The asymmetrical posture was particularly problematic when he was riding in the car because the extreme positioning prevented easy breathing. His mother had to stop the car to reposition Brandon at times. He would stay in the corrected position only for moments. We began using the roll only as a training device with a caregiver sitting and watching to be sure it did not block his breathing. His pulmonologist approved the modification. However, it became possible for him to sit for long times without ever pulling his head forward, down, and to the side. Finally, the last chair did not require the chin roll because Brandon sat erect with his head in midline. It was thought that this worked by gradually changing the set point for the muscle spindles of the neck extensors and increasing activation of the postural extensors (refer to Chapter 4 on a posture and movement model), and that it changed the perception of the visual horizon. |
Abbreviations: ADLs, activities of daily living; SaO2, oxygen saturation.
Brandon’s wheelchair was an important contextual factor in his life. However, selecting it and monitoring it for fit and function were only small parts of the intervention plan. The therapist had to intervene to prepare and assist Brandon to learn how to sit in the chair, to develop the functional skills that could occur while he was in the chair, and to instruct the family in how to capitalize on possibilities the chair afforded to address Brandon’s impairments and to maximize his participation. After establishing the session outcomes, the therapist needed to be mindful of the impairments identified in his evaluation that interfered with functional sitting in the chair. Once these were known, the therapist could select intervention strategies that would best address each impairment.
Summary of Impairments Preventing Activity or Participation Related to Supported Sitting
Multisystem Impairments
• Decreased postural control of head, neck and trunk.
• asymmetry LEs > UEs; atypical alignment of the hips.
• Poor sitting balance.
• Slow and limited limb movement—predominantly to midrange movement.
The options for specific standardized testing of the multisystem impairments are still somewhat limited. However, clinical measures for postural control are being developed.31,32,33 In addition, the literature is beginning to explore the effectiveness of adaptive seating on posture and control in children with CP.34
Single-System Impairments
Skeletal
These bony deformities contributed to asymmetrical weight bearing through the pelvis and therefore poor alignment.
• Scoliosis with surgical stabilization.
• Hip dysplasia; status post–derotation osteotomy.
• Osteopenia with fracture of left distal femur repaired with titanium rod.
• Leg length discrepancy with left leg ~1 in shorter than right.
Muscular/Soft Tissue
• Shortened cervical muscles, right more than left, and extensors more than flexors.
• Shortened hip musculature—flexors, extensors, and hamstrings and shortened gastrocnemius–soleus groups.
• Decreased strength of all muscles with all muscles below the Fair grade.
Integumentary
These range limitations make it more difficult to move the pelvis over the femurs for dynamic control in sitting and contribute to poor trunk and head control. He did not have significant issues surrounding the spinal stabilization.
• Fascial restrictions that limited movement following each surgery with restrictions
 Near incision sites from the osteotomy.
Near incision sites from the osteotomy.
 Near left knee near fracture site.
Near left knee near fracture site.
 Throughout the abdomen related to GI surgeries and his shunt placement and revisions.
Throughout the abdomen related to GI surgeries and his shunt placement and revisions.
Neuromuscular
• Decreased recruitment of postural motor units.
• Muscle activation with isometric or concentric work most often and with extremely limited eccentric control.
• Limited repertoire of movement synergies with limited movement in frontal plane and extremely limited movements in transverse plane.
• Decreased isolated recruitment within limbs.
• Hyperstiffness of all four limbs.
Sensory
• Diagnosed with cortical visual impairments.
• Decreased somatosensory awareness of the lower body.
Specific Physical Therapy Intervention to Meet Outcomes Related to Participation in Supported Sitting
A pretest was performed in each session that focused on a sitting activity. In addition to having an activity pretest, Brandon required a medical status pretest to establish boundaries for the day. Brandon’s mother and, with time, his home health nurses, were excellent at providing information on his status that could set the stage for a good day or a not-so-good day. As is common in children with severe involvement, many of Brandon’s activities were borderline skills. Even a slight decrease in his medical status could result in major changes in his functional abilities. For Brandon, monitoring his respiratory status and his regulatory status had to be an ongoing process. However, in many ways, it was made easier by the constant use of a pulse oximeter with an alarm that triggered at an established basement level. Brandon’s overall affect was also a clear expression of his O2 level. When he was not getting adequate oxygenation, Brandon became lethargic, even if his monitor had not registered the critically low oxygenation level. However, Brandon usually came to therapy ready to move, to work, and to try new tasks. If he did not have that attitude, he did not feel well.
The first step in each session was to transition out of the wheelchair. Even when the activity outcome involved sitting in his wheelchair, the first therapeutic activity done after the pretest was to transition him out of the chair. The only way to facilitate Brandon to sit more functionally in the chair was to transfer him out of the chair and begin to address the impairments that were interfering with the outcome achievement.
The preparation aspects of intervention usually began with a focus on the respiratory and regulatory systems. The role of the therapist usually was not to treat the respiratory system because he was on numerous medications to address those needs (see medications listed in Table B8.2). There were, however, occasions when a session did include chest physical therapy. The strategies addressed the changes in the proportions of the chest29 as well as providing direct chest physical therapy.27,28 These were most often performed with Brandon positioned on a large therapy ball (the surface was forgiving for any of his trunk or limb malalignments) and could be rolled to assist in drainage. Brandon enjoyed the rhythmic clapping on his chest, and at times, this strategy was also used to modify his neuromuscular status by decreasing his overall hyperstiffness. The PT could then gradually reposition the limbs to elongate the overactive or tight muscles of the hips, shoulders, and trunk through weight shifting, tractioning, and adding manual vibration through the length of the limbs. This work also provided an opportunity to introduce elongation of the hamstrings through weight shifting of the pelvis across the LEs. He had greater limitations on the left because it was the leg that had fractured. He had fascial scarring both distally and medially near the knee at the point at which the titanium rod had been inserted and proximally from the varus derotation osteotomy that had been performed. At times, the therapist added myofascial elongation to lengthen those specific regions.
There were many other days when it was not necessary to start with this respiratory intervention and ball strategies. On those days, we were more likely to start the session by jointly addressing the musculoskeletal and neuromuscular impairments with Brandon moving into, out of, and around a variety of sitting postures. When he was in physical therapy, he was moving and transitioning between functional postures. Initial movements or transitions stressed weight shifting in the frontal and transverse planes through and over the pelvis (Fig. B8.2). With assistance, Brandon could transition from a modified prone or supine position through side lying and move up and down toward sitting. A larger ball allowed more support to greater parts of his body. After Brandon’s spinal stabilization, most of this motion occurred at the pelvic–femoral (hip) joints and within the shoulder girdle, but there were associated movements of the ribs and soft tissue of the trunk.
For function, Brandon needed to be able to move his pelvis over stabilized femurs. His legs needed slightly more than 90° of hip flexion to be placed in the wheelchair, when he was lifted from the chair, and to make small weight shifts forward to vocalize, to reach for items, toys, caregivers, or his brothers. He needed to be able to relieve pressure from the ischial tuberosities. These weight shifts were important both in and out of the chair. The mobility was facilitated during activities of play, reach, or transitions primarily out of the chair.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Be able to perform stand pivot transfers between surfaces of equal heights; that he could hold supported standing for 30 seconds to aid in transfers and in ADLs, such as dressing.
Be able to perform stand pivot transfers between surfaces of equal heights; that he could hold supported standing for 30 seconds to aid in transfers and in ADLs, such as dressing.






