The levels of the MRC scale are precisely defined, but not linear. It is a common error to believe the MRC grades are evenly spaced and that grade 5 is normal, grade 4 is minimal or mild weakness, grade 3 is moderate weakness, grade 2 is severe, and so forth. In fact, anything less than grade 5 denotes significant weakness. Grade 4 is moderate weakness, and anything less is severe weakness. A patient who is diffusely 4/5 does not have mild or equivocal weakness but major and serious involvement. One must not confuse poor effort with weakness. A muscle is graded by the maximal power demonstrated, even if it is only briefly.
The muscle strength scale used by physical therapists grades muscles on a six-point scale from zero (no motion) through trace, poor, fair, and good to normal. The scale used at the Mayo clinic grades muscle strength on a five-point scale that is more linear. Normal is designated as zero, mild weakness is -1, and total paralysis is -4.
The different levels of the MRC scale are so precisely defined that there is good interexaminer consistency once the fine points of proper positioning and other details are mastered. In clinical practice, the MRC scale is often expanded to include subgrades (e.g., 5-, 4+). The MRC eventually saw the need to include grades 4-and 4+. Mendell and Florence developed a formal modified MRC scale. In general use, the subgrades are not so precisely defined, and there is much less inter-and even intraexaminer consistency. Approximate guidelines are all that is possible. Before attempting to describe these guidelines, the important issue of examiner-patient mismatch should be recognized.
There is obviously considerable individual variation in muscle power, dependent in part upon size, gender, body build, age, and activity level. This variability affects examiners as well as patients. Patients come large and small, young and old, male and female, and physically strong and relatively weak. So do physicians. A large, young, powerful, male physician examining a small, old, sick, female patient has an unfair advantage. He may tend to think she is weak when she is in fact normal for her age, sex, and circumstances. Conversely, a small, relatively weak female physician examining a large, powerful man may miss significant weakness because of strength mismatch.
As a general principle, reliable strength testing should attempt to break a given muscle. Muscles are most powerful when maximally shortened. Another consideration is the lever effect. Attempting to overpower a muscle, such as a deltoid, using a very short lever (examiner’s hand at the mid-upper arm) is much less likely to meet with success than using a long lever (patient’s elbow extended and examiner pressing down on the wrist). A small, weak examiner can overcome the deltoid of the most powerful man by keeping the patient’s elbow extended and using both hands to pull down the wrist. Technique matters.
By varying the length of lever and the shortening of the muscle permitted, the examiner may give or take mechanical advantage as necessary to compensate for strength mismatch. Many patients of different ages, sizes, and strength levels must be examined in this fashion in order to develop an appreciation of the expected strength of a muscle for a given set of circumstances.
So, for an examiner of average size and strength examining a patient of average size and presumed normal strength, the following is a useful guideline for assessing power in the major muscle groups. If it requires the whole hand and a firm push to break the muscle, the power is grade 4+. If the muscle can be broken using three fingers, it is grade 4. If it can be broken using one finger, it is grade 4-. Some clinicians use the grades of 3-and 2-to describe muscles that can move against gravity or with gravity eliminated, but not through a full range, and the grade of 5-to indicate borderline or equivocal weakness.
Some muscles are “special cases.” The small hand muscles are best examined by matching them against the examiner’s like muscle (e.g., abductor pollicis brevis [APB] to abductor pollicis brevis). This method is beautifully described and illustrated in Segmental Neurology by John K. Wolf. The gastrocnemius muscles are normally so powerful it is virtually useless to examine them using hand and arm strength, unless they are very weak. Having the patient walk on tiptoe, hop, support the entire body weight on one tiptoe, or do one-legged toe raises are usually better methods.
PATTERNS OF WEAKNESS
There are common patterns of weakness. Recognition of a pattern may help greatly in lesion localization and differential diagnosis. Identification of the process causing weakness is further aided by accompanying signs, such as reflex alterations and sensory loss. Table 27.2 reviews the features of upper motor neuron versus lower motor neuron weakness. Table 27.3 summarizes some common patterns of weakness and their localization.
TABLE 27.2 Features of Upper Motor Neuron versus Lower Motor Neuron Weakness
CNS, central nervous system.
TABLE 27.3 Common Patterns of Weakness with Lesions at Different Locations in the Neuraxis
*With corticospinal lesions, DTRs acutely may be normal or decreased (neural shock)
**Extremity weakness in a corticospinal tract distribution
DTR, deep tendon reflex; Y yes; N, no; INCR, increased; DECR, decreased.
Weakness may be focal or generalized. When focal, it may follow the distribution of some structure in the peripheral nervous system, such as a peripheral nerve or spinal root. It may affect one side of the body in a “hemi” distribution. A hemi distribution may affect the arm, leg, and face equally on one side of the body, or one or more areas may be more involved than others. The CST preferentially innervates certain muscle groups, and these are often selectively impaired (see Chapter 25). When weakness is nonfocal, it may be generalized, predominantly proximal, or predominantly distal.
Generalized Weakness
The term generalized weakness implies that the weakness involves both sides of the body, more or less symmetrically. When a patient has truly generalized weakness, bulbar motor functions—such as facial movements, speech, chewing, and swallowing—are involved as well. Weakness of both arms and both legs with normal bulbar function is quadriparesis or tetraparesis. Weakness of both legs is paraparesis. When weakness affects all four extremities, the likely causes include spinal cord disease, peripheral neuropathy, a neuromuscular junction disorder, or a myopathy.
When spinal cord disease is the culprit and the deficit is incomplete, more severe involvement of those muscles preferentially innervated by the CST can frequently be discerned. Reflexes are usually increased (though in the acute stages they may be decreased or absent); there is usually some alteration of sensation; sometimes a discrete spinal “level”; superficial reflexes disappear; and there may be bowel and bladder dysfunction. Generalized peripheral nerve disease tends to predominantly involve distal muscles, although there are exceptions. There is no preferential involvement of CST innervated muscles; reflexes are usually decreased; sensory loss is frequently present; and bowel and bladder function are not disturbed. With a neuromuscular junction disorder, the weakness is likely to be worse proximally; sensation is spared; reflexes are normal; and there is usually involvement of bulbar muscles, especially with ptosis and ophthalmoplegia. When the problem is a primary muscle disorder, weakness is usually more severe proximally; reflexes are normal; sensation is normal; and with only a few exceptions, bulbar function is spared except for occasional dysphagia.
Amyotrophic lateral sclerosis (ALS) causes a characteristic pattern of weakness. The weakness and wasting due to lower motor neuron involvement is accompanied by weakness and hyperreflexia due to upper motor neuron involvement.
Focal Weakness
Weakness of the arm and leg on one side of the body is hemiparesis. Monoparesis is weakness limited to one extremity. Diplegia is weakness of like parts on the two sides of the body; the term spastic diplegia refers to weakness of both legs that occurs in cerebral palsy; and facial diplegia is weakness of both sides of the face. Spastic weakness of one arm and the opposite leg is referred to as cruciate or crossed paralysis, or hemiplegia alternans.
Certain patterns of muscle weakness point to a peripheral nerve, plexus, or root lesion. With a peripheral nerve lesion, all muscles below the level of the lesion are at risk. It is increasingly recognized, however, that not all muscles distal to a peripheral nerve lesion are necessarily equally affected. When multiple muscles of an extremity are weak, localization depends on recognizing the common innervating structure. In cervical radiculopathy, the muscles involved are innervated by different peripheral nerves and different brachial plexus components, but all by the same root. For instance, lesions of the middle trunk of the brachial plexus are exceedingly rare, so weakness of the triceps (radial nerve) and the pronator teres (PT) (median nerve) always means a lesion of the C7 root.
A focal neuropathy, such as a radial nerve palsy, or a spinal root lesion, such as from a herniated disc, causes weakness limited to the distribution of the involved nerve or root. A complete plexopathy, such as a traumatic brachial plexopathy, may cause weakness of the entire limb. Partial lesions may cause weakness only in the distribution of certain plexus components. With such lower motor neuron pathology, reflexes are typically decreased, and there is often accompanying sensory loss. Localization of focal weakness due to root, plexus, and peripheral nerve pathology requires intimate familiarity with peripheral neuroanatomy. Anterior horn cell disease often begins with focal weakness that may simulate mononeuropathy, but it evolves into a more widespread pattern as the disease progresses, culminating in generalized weakness. Except for extraocular muscle involvement in myasthenia gravis, it is rare for a myopathy or neuromuscular junction disorder to cause focal weakness.
NONORGANIC WEAKNESS
Nonorganic weakness due to psychiatric disorders—such as hysteria, conversion disorder, malingering, or depression—is common. The first step in evaluating weakness is often deciding whether it is organic or nonorganic. This distinction is not always easy. Patients with nonorganic weakness are commonly thought to have neurologic disease, but just as often patients with real weakness are thought to be hysterical or malingering. Patients with real weakness may embellish the deficit and have a superimposed nonorganic component. A patient may have real weakness in one area and nonorganic weakness in another area. Some patients with organic weakness may allow resistance to collapse when the examiner begins to defeat a muscle so that real weakness may appear to be related to poor effort. For example, with a ruptured supraspinatus tendon (torn rotator cuff), the abducted arm may collapse suddenly with the application of minimal resistance (drop-arm sign). When a movement causes pain, resistance may be less than full and the effort may be erratic.
Coaching is often helpful. The examiner exhorts the patient not to give up, to keep pushing or pulling no matter what. Simple encouragement to keep trying even if the patient is losing may suffice to improve effort. Some patients, in spite of all, will simply not give full effort. Their efforts are erratic and variable. Some things are often useful in distinguishing organic from nonorganic weakness. Patients with bona fide organic muscle weakness will yield smoothly as the examiner defeats the weak muscle. The patient gives uniform resistance throughout the movement. If the examiner decreases his resistance, the patient will begin to win the battle. If the examiner drops the resistance level, the patient with nonorganic weakness will not continue to push or pull. Instead, the patient will also stop resisting so that no matter how little force the examiner applies, there is an absence of follow-through and the patient never overcomes the examiner. When there is nonorganic weakness, resistance is erratic and often collapses abruptly. The muscular contractions are poorly sustained and may give way suddenly, rather than gradually, as the patient resists the force exerted by the examiner. Some patients will give up entirely and allow the muscle or limb to flop; others will provide variable resistance throughout the range of motion with alternating moments of effort and no effort. At the peaks of contraction, strength is normal; in the valleys, there is little or no resistance. This pattern of variable strength is referred to as “ratchety,” “give way,” or “catch and give.” It is characteristic of nonorganic weakness. With nonorganic weakness, there may be an increase or a decrease in strength with repeated testing. Contraction of the apparently weak muscle may be felt when the patient is asked to carry out movements with synergistic muscles, or the antagonists may be felt to contract when the patient is asked to contract the agonist (e.g., the triceps muscle twitches when the patient is told to flex the elbow). Functional testing may fail to confirm weakness suspected during strength testing. For example, there may be apparent foot dorsiflexion weakness, yet the patient is able to stand on the heel without difficulty.
The patient with nonorganic weakness may make little effort to contract the muscles necessary to execute a particular movement. He may be calm and indifferent while demonstrating the lack of strength, showing little sign of alarm at the presence of complete paralysis, and smile cheerfully during the examination. If the examiner raises and drops an extremity, a limb with psychogenic paralysis may drop slowly to avoid injury, while an extremity with real weakness would drop rapidly, especially if the paralysis is flaccid. In psychogenic paralysis of the arm, the latissimus dorsi may appear paretic when tested by having the patient adduct the arm, but contract normally on coughing. In simulated hemiplegia, the patient may be unable to adduct either the affected arm or leg against resistance, yet if asked to keep both arms against the body or both legs close together, the adductors contract strongly on both sides because it is difficult to adduct one extremity without adducting its apparently paralyzed fellow. In testing paralysis of the finger muscles, the patient may be asked to pronate the forearms and interlock the fingers so that the left fingers are on the right and vice versa (Figure 36.6); the examiner then points to the individual fingers and tells the patient to move them. It is difficult for one to determine immediately whether the indicated finger is on the right side or on the left; if the patient attempts to respond promptly, he makes many mistakes. Similar tests may be carried out by asking the patient to perform individual movements with the hands behind the back.
The Hoover (automatic walking) sign is useful for evaluating suspected nonorganic leg weakness. When a normal supine patient flexes the hip to lift one leg, there is a downward movement of the other leg. The extension countermovement of the opposite leg is a normal associated movement (see Chapter 42). An extension movement of one leg normally accompanies flexion of the other leg, as in walking. In organic leg weakness, the downward pressure of the contralateral heel occurs when the patient tries to raise the weak leg, and the examiner can feel the extension pressure by placing a hand beneath the heel that remains on the bed. Downward pressure is also present, to a lesser degree, in the weak leg as the patient raises the normal leg. In nonorganic leg weakness, there is no downward pressure of the contralateral heel, but the extension movement of the “paralyzed” leg may be felt as the good leg is raised. Similarly, normally and with organic hemiparesis, if the patient presses down on the bed with the good leg, the opposite leg may flex slightly; this movement does not occur in nonorganic weakness. Hoover’s sign is absence of the expected associated movement. In the quest for ways to distinguish real from hysterical weakness at the turn of the 20th century, Hoover thought this maneuver was more useful than the Babinski sign (Chapter 40). Earlier authors described signs for distinguishing organic and nonorganic weakness based on the same principles. The abductor sign is similar and seeks synergistic movement of the nonparetic leg when the patient is asked to abduct the paretic leg. In nonorganic paresis, the paretic leg demonstrates synergistic abduction when the sound leg is tested, and the sound leg does not exert normal abduction power and can be moved into a hyperadducted position when the paretic limb is tested. It may be useful when relatively preserved hip extensor strength limits the utility of Hoover’s test. In the Spinal Injuries Center (SCI) test, patients unable to raise their knees spontaneously have a positive test, indicating nonorganic weakness, when their knees remain up after being lifted by the examiner. See LaFrance for video of the Hoover, abduction, and SCI tests. Looking for the presence or absence of other associated movements may sometimes help in the differentiation between organic and psychogenic weakness (Chapter 42). Investigators have developed a computerized, quantitative method for detecting nonorganic weakness based on these principles.
In psychogenic weakness, muscle tone may be normal, decreased, or variable, but it is often increased with pseudorigidity or pseudospasticity. Rigidity, if present, resembles voluntary resistance. The part may be held firmly in a bizarre position. Abnormalities in tone usually vary from time to time, especially under the influence of suggestion.
EXAMINATION OF MOTOR STRENGTH AND POWER
Evaluation of the strength of various muscle groups and movements can become complex, depending upon the degree of detail necessary. Isolated contraction of a single muscle is rarely possible because muscles with similar functions participate in almost every movement. Normal contraction of synergists and fixating muscles and relaxation of antagonists are also necessary. Still, the predominant action of a single muscle can usually be determined and tested. Some functions are carried out by many muscles acting synergistically (e.g., flexion and extension of the trunk), and the muscles must be tested as a group by assessing the movement rather than individual muscles. It is helpful to be fluent with the primary actions of the major muscles and their peripheral nerve, plexus, and root innervations. The strength of each major pertinent muscle group should be determined individually and its strength grade recorded.
Reliable strength testing requires proper patient positioning and avoidance of unwanted movements. Testing may be done in various positions, depending on the muscle to be tested and its power. Testing in the seated position suffices under most circumstances. It is important to fix the proximal portion of a limb when the movements of the distal portion are being tested. For instance, when testing forearm pronation strength, the patient must not be allowed to internally rotate the shoulder to compensate for lack of pronation power. When evaluating very weak muscles, gravity must be eliminated to detect residual power. A very weak biceps muscle (MRC grade 2/5), even when it cannot succeed against gravity, may be able to flex the elbow if the arm is raised to shoulder height so that the forearm can be moved horizontally. The wrist and finger drop of radial nerve palsy creates such a mechanical disadvantage for contraction that the patient may appear to have weakness of grip and finger abduction, but these functions are intact when the wrist and fingers are passively extended.
EXAMINATION OF SPECIFIC MOVEMENTS AND MUSCLES
The motor examination of the muscles supplied by those cranial nerves that have motor functions is discussed separately. For the trunk and extremities, the strength and power of the individual muscles and of movements is assessed as appropriate for the clinical circumstances. Many reference sources are available to assist in learning muscle examination techniques. There is some difference regarding the exact innervation of individual muscles among different reference sources, and occasionally there is variable or anomalous innervation. Table 27.4 through Table 27.7 give the most generally accepted spinal cord segment and peripheral nerve innervation of the more important muscles. Table 27.8 and Table 27.9 give the innervation by root.
TABLE 27.4 Innervation of Muscles Responsible for Movements of the Head and Neck
TABLE 27.5 Innervation of Muscles Responsible for Movements of the Shoulder Girdle and Upper Extremity
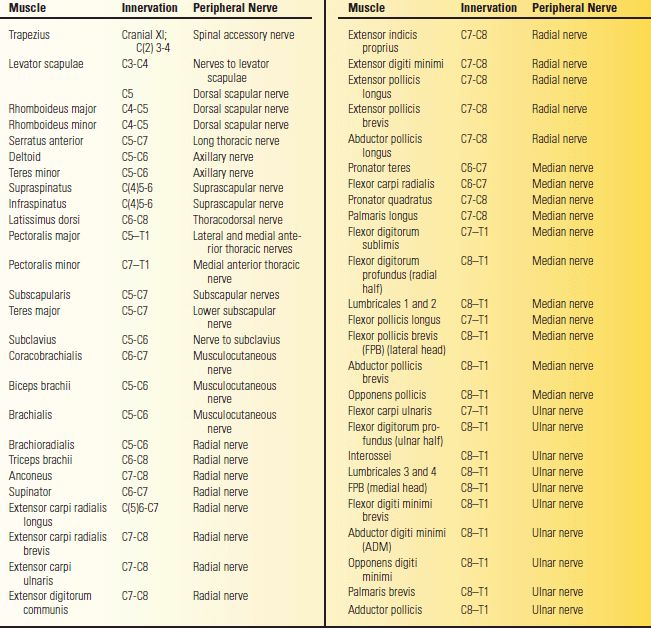
TABLE 27.6 Innervation of Muscles Responsible for Movements of the Thorax and Abdomen
TABLE 27.7 Innervation of Muscles Responsible for Movements of the Lower Extremities
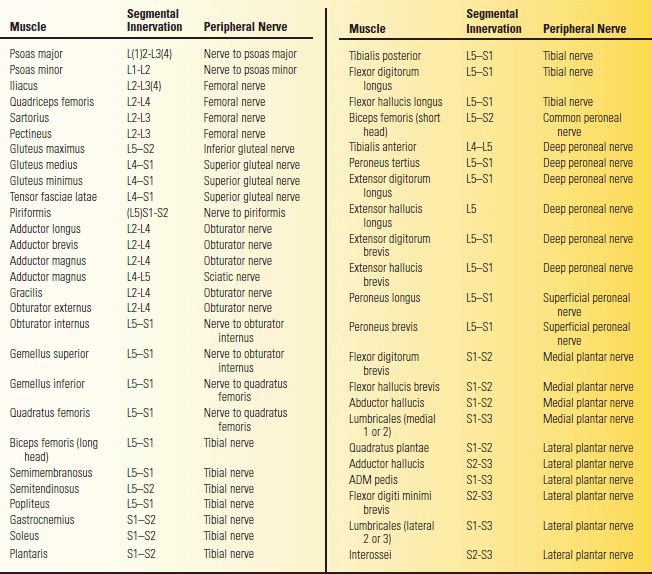
TABLE 27.8 Major Upper-Extremity Muscles Innervated by Different Roots
BR. brachioradialis; FCR, flexor carpi radialis; ECRL, extensor carpi radialis longus; EDC, extensor digitorum communis; ECU, extensor carpi ulnaris; EIP, extensor indicis proprius; FCU, flexor carpi ulnaris; EDS, flexor digitorum superficialis; FPL, flexor pollicis longus; EDP. flexor digitorum profundus; PQ. pronator quadratus;
APB, abductor pollicis brevis; APL, abductor pollicis longus; OP, opponens pollicis; AP, adductor pollicis; ADM, abductor digiti minimi.
TABLE 27.9 Major Lower-Extremity Muscles Innervated by Different Roots
TEL, tensor fascia lata; TA, tibialis anterior; EHL, extensor hallucis longus; EDL, extensor digitorum longus; EDB, extensor digitorum brevis; TP, tibialis posterior; EDL, flexor digitorum longus; EHL, flexor hallucis longus; ADMP, abductor digiti minimi pedis; AH, abductor hallucis.
The action of a muscle about a joint may vary depending on the part of the muscle activated and the position of the joint. Parts of some large muscles, such as the gluteus maximus, may have secondary actions that are different from other parts. For instance, the upper part of the gluteus maximus abducts the hip, whereas the lower part adducts it. Still, each muscle has a primary action in which all parts participate, in this instance it is hip extension. The angle of the joint about which a muscle acts may influence its leverage and angle of pull. In extreme cases, a muscle may move to the opposite side of the axis of rotation and have an action in one joint position that is different from its action in another joint position (inversion of action). For instance, the hip adductors act secondarily as hip flexors when the hip is extended, but as extensors when the hip is flexed; the piriformis externally rotates the extended hip, but internally rotates the flexed hip.
Examination of Movements and Muscles of the Neck
The principal neck movements are flexion, extension (retraction), rotation (turning), and lateral bending (tilting, abduction). Many different muscle groups contribute to the various neck movements. Except for the sternocleidomastoid (SCM) and trapezius, it is not possible to examine them individually, and the assessment is made of movement (e.g., neck flexion) rather than particular muscles. The spinal accessory nerve, along with the second, third, and fourth cervical segments, supplies the SCM and trapezius muscles. The SCM is a flexor and rotator of the head and neck; the trapezius retracts the neck and draws it to one side. Other muscles that contribute to neck flexion include the platysma, suprahyoid, infrahyoid, scalenes, and the prevertebral group of muscles (longus colli and capitis, rectus capitis).
Many muscles contribute to neck extension, including the trapezius and the paravertebral muscles. Many of these muscles when contracting unilaterally rotate the spine. The paravertebral musculature is a massive, complex amalgam of individual muscle groups that primarily serve to extend and rotate the neck and trunk. Four principal muscle subgroups combine to form the paravertebral muscles: the splenii, erector spinae, transversospinalis, and interspinal-intertransverse. All of these muscles lie deep and medial in the groove formed between the transverse and spinous processes of the vertebral bodies. They are further named for the vertebral segment in which they lie (e.g., transversospinalis cervicis). The splenius capitis is a powerful ipsilateral rotator of the head; the splenii contracting bilaterally extend the neck. The trapezii and splenii capitis are commonly injected with botulinum toxin to treat cervical dystonia. The paraspinal muscle complex generally receives its innervation from multiple levels. These muscles arise from a common embryologic precursor muscle mass, and their innervation shows extensive longitudinal overlap (Table 27.4).
Neck flexors are tested by having the patient try to place the chin on the chest as the examiner applies extension force to the forehead (Figure 27.1). Extensors are tested by having the patient extend against the examiner’s resistance applied to the occiput (Figure 27.2). Neck rotation is accomplished by the contralateral SCM and ipsilateral splenius capitis and trapezius; examination of the SCM and trapezius muscles is discussed in Chapter 19. Neck flexor strength may be tested with the patient sitting or supine, neck extension sitting or prone. The neck flexion test consists of measuring the time the supine patient can keep the head raised with the chin on the chest; most patients can keep their head in this position for at least 1 minute. This test is sometimes useful in the evaluation of myopathies and neuromuscular junction disorders, the principal conditions that cause neck flexor or extensor weakness. Abnormalities of neck position may occur in conditions in which there is no muscle weakness, and these can sometimes be confused with the effects of a weak muscle. The patient with meningismus may have the head retracted, whereas the patient with Parkinson disease may have it flexed. Cervical dystonia can cause an almost infinite number of abnormal head positions, including torticollis (head turned or tilted), anterocollis (head flexed), and retrocollis (head extended). Examination of the neck muscles must be done carefully in any patient at risk for cervical spine disease.
FIGURE 27.1 Examination of flexion of the neck. The patient attempts to flex his neck against resistance; the sternocleidomastoid, platysma, and other flexor muscles can be seen and palpated.
FIGURE 27.2 Examination of extension of the neck. The patient attempts to extend his neck against resistance; contraction of the trapezius and other extensor muscles can be seen and felt, and strength of movement can be judged.
Examination of Movements and Muscles of the Upper Extremities
The responsible muscles and their innervation are given in Table 27.5.
The Shoulder
Movements of the shoulder take place at the sternoclavicular, acromioclavicular, and glenohumeral joints. Because the scapula is firmly connected to the clavicle at the acromioclavicular joint, the two bones tend to move as a unit with the motion taking place primarily at the sternoclavicular joint. Movements of the scapula are elevation, depression, retraction (movement away from the chest wall), protraction (movement toward the chest wall), and rotation. The ventral surface of the scapula is a concavity known as the subscapular fossa that is filled mostly with the subscapularis muscle. The serratus anterior lies between the subscapularis and the chest wall and inserts into a thin rim of the scapula along the vertebral border and slightly expanded triangular areas at the superior and inferior angles (Figure 27.3). The serratus runs obliquely from its origination from the upper eight ribs along the lateral chest wall to its attachment to the scapula. The trapezius is a diamond-shaped muscle that attaches widely to the shoulder girdle. The superior fibers insert along the posterior border of the clavicle and scapular spine, the middle and lower fibers along the scapular spine. The upper and middle fibers insert laterally along the scapular spine, the lower fibers more medially. The rhomboids (major and minor) arise from the spinous process of the upper thoracic vertebrae and insert along the medial border of the scapula. The levator scapulae originates from the upper cervical vertebra and drops diagonally to insert along the upper medial border of the scapula.
FIGURE 27.3 The muscles of the scapula.
The upper fibers of the trapezius, assisted by the levator scapulae, elevate the scapula and the point of the shoulder, and rotate the scapula upward. The middle fibers rotate the scapula upward and assist the rhomboids in retraction. The lower fibers rotate and depress the scapula and draw it toward the midline. The rhomboids act primarily to retract the scapula, bracing the shoulder backward. The levator scapulae acts with the trapezius to elevate the scapula. The serratus anterior, assisted by the pectoralis minor, protracts the scapula, pulling it anteriorly. It is critical in all functions that involve reaching or pushing forward. The expanded insertion at the inferior angle helps to pull the inferior scapular angle forward around the chest wall. It also, along with the trapezius, rotates the scapula and raises the point of the shoulder to abduct the arm above horizontal. It helps to fix the scapula while other muscles abduct or flex the arm.
Elevation of the scapula, as in shrugging the shoulder, is carried out by the upper trapezius and levator scapulae muscles, assisted by the SCM. The levator scapulae is innervated by direct branches from C3 and C4 with a contribution from C5 via the dorsal scapular nerve. The levator scapulae draws the scapula upward and rotates it so that the inferior angle approaches the spinal column. Depression of the scapula is carried out primarily by the lower trapezius, pectoralis minor, and subclavius muscles.
Retraction of the scapula is carried out primarily by the rhomboids and the middle trapezius. The rhomboids also draw the scapulae together, as in standing at attention. The rhomboids are innervated by a twig directly from the C5 nerve root, and not via the brachial plexus. Examination of the rhomboids is important in the differentiation of C5 radiculopathy from upper trunk brachial plexopathy. In protraction of the scapula, the scapula moves forward as in throwing a punch. This movement is carried out primarily by the serratus anterior (long thoracic nerve, C5-C7). The serratus keeps the vertebral border of the scapula applied to the thorax and pulls the scapula forward and laterally. Rotation of the scapula is accomplished by the trapezius, serratus anterior, pectorals, rhomboids, and latissimus dorsi. Normal scapular rotation is essential to efficient shoulder abduction.
Scapulohumeral Rhythm
There are two motions involved in abducting the arm: scapulothoracic and glenohumeral. The scapulothoracic motion is the movement of the scapula in relation to the chest wall; the glenohumeral is the movement at the shoulder joint. These two motions normally occur in harmony to effect smooth arm movements. When the scapula does not move normally, the arm cannot raise normally. As abduction begins, the scapular muscles—especially serratus anterior—fix the scapula, so the pull of the deltoid is on the humerus and not the scapula. As the deltoid abducts the shoulder toward 90 degrees, the serratus anterior and trapezius rotate the scapula. The serratus pulls forward and laterally on the inferior angle, holding the scapula close to the chest wall, while the upper fibers of the trapezius pull up on the lateral end of the clavicle and the lower fibers pull down on the medial part of the scapular spine (Figure 27.4). The smooth interaction of scapula and shoulder joint movements is referred to as the scapulohumeral rhythm. For every 2 degrees of motion at the glenohumeral joint, there is 1 degree of scapular rotation. After the deltoid abducts the arm to the horizontal, further action by the upper trapezius elevates and rotates the scapula further to allow the arm to be raised overhead.
FIGURE 27.4 Upward rotators of the scapula. (Modified from Weibers DO, Dale AJD, Kokmen E, et al., eds. Mayo Clinic Examinations in Neurology. 7th ed. St. Louis: Mosby, 1998, with permission.)
The Scapular Muscles
The rhomboids can be tested by having the patient, with hand on hip, retract the shoulder against the examiner’s attempt to push the elbow forward (Figure 27.5). If the patient braces the shoulders backward as if standing at attention, the bulge of the rhomboids can be seen and palpated along the medial border of the scapula. Another test of rhomboid function is to have the patient place the back of the hand against the small of the back and to push backward with the palm against the examiner’s resistance. The rhomboid major contracts vigorously as a downward rotator of the scapula. Lifting the hand off the small of the back is also used to test the subscapularis. The levator scapulae is tested by observing elevation of the scapula; it is rarely possible to detect weakness of the levator scapulae on clinical examination.
FIGURE 27.5 Examination of the rhomboids. With hand on hip, the patient retracts the shoulder against the examiner’s effort to push the elbow forward; the contracting muscles can be seen and palpated.
The different parts of the trapezius must be tested separately. One test of the upper fibers is to have the patient shrug the shoulders against resistance (Figure 19.4). A better test is resisting the patient’s attempt to touch the occiput to the acromion. The middle fibers may be tested by having the patient retract the scapula against resistance (Figure 27.6) or having the patient hold the arm horizontally abducted, palm up, and attempting to push the elbow forward. With unilateral trapezius paralysis, the patient cannot retract the shoulder or abduct the arm above horizontal. Because of the weight of the arm, the upper portion of the scapula falls laterally, the inferior angle moves medially, and the vertebral border is flared. The sagging of the shoulder causes a drooping of the entire arm, and the fingertips on the involved side are at a lower level than on the normal side. With trapezius atrophy, the superior angle of the scapula may bulge beneath the skin. There is little loss of shoulder-shrug ability because the levator scapulae and rhomboids are able to elevate the scapula, but the normal slant from the base of the neck to the shoulder becomes squared off because of loss of trapezius bulk. The patient may be able to elevate the arms forward with little or no difficulty because the serratus anterior is primarily responsible for scapular fixation and rotation in that plane.
FIGURE 27.6 Examination of the trapezius. On retraction of the shoulder against resistance, the middle fibers of the muscle can be seen and palpated.
The serratus anterior can be tested by having the patient make movements that involve forward reaching or pushing, and observing for evidence of scapular winging (see next section). When there is significant weakness, abnormalities may be apparent when the patient simply tries to raise the arm overhead. More subtle degrees of weakness may be brought out by having the patient push forward against resistance. The classical test is to have the patient push against a wall, comparing how well the scapulae remain against the chest wall on the two sides (Figure 27.7).
FIGURE 27.7 Examination of the serratus anterior. The patient pushes against a wall with his arms extended horizontally in front of him; normally, the medial border of the scapula remains close to the thoracic wall.
Winging of the Scapula
Normally, the medial border of the scapula remains close to the chest wall when the arms are raised. However, with weakness of either the serratus anterior or the trapezius, the vertebral border or the entire scapula protrudes posteriorly, away from the thoracic wall. This causes the deformity known as “winging” (Figure 27.8). The trapezius is a rotator and retractor of the scapula and functions primarily during abduction of the arm to the side in the coronal plane of the body. When the trapezius is weak, scapular winging is more apparent on attempted abduction of the arm than on forward elevation. Trapezius winging may be made more conspicuous by having the patient bend forward at the waist so the upper body is parallel to the ground, then raise the arms to the sides, as if beginning a swan dive. This requires strong action by the trapezius to retract the scapula and accentuates the posterior displacement of the shoulder girdle.
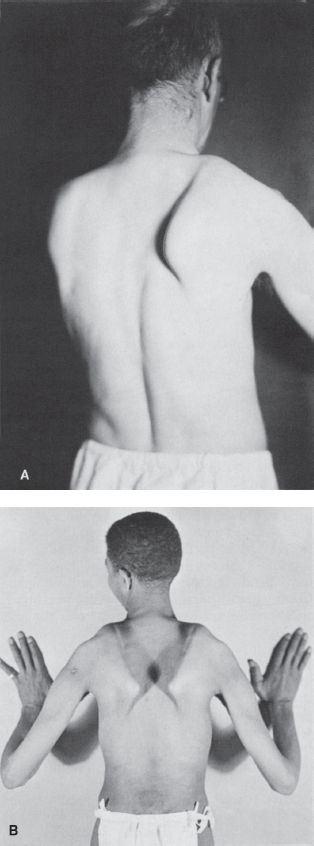
FIGURE 27.8 “Winging” of the scapula. A. Unilateral winging secondary to paralysis of the right serratus anterior. B. Bilateral winging in a patient with muscular dystrophy.
The serratus anterior is primarily a protractor of the scapula and functions during forward arm elevation. When the serratus is weak, the inferior angle is shifted medially and the entire vertebral border rides up from the chest wall. Serratus anterior weakness causes winging that is more obvious when trying to elevate the arm in front, in the sagittal plane of the body; it is less obvious when the arms are abducted to the sides. This difference aids in differentiating serratus anterior winging (as from a long thoracic nerve palsy) from the flaring of the scapula that occurs with trapezius weakness (as from a spinal accessory nerve palsy). Serratus winging may be accentuated by having the patient protract the scapula against resistance (Figure 27.7). Another method to bring out mild serratus winging is to have the patient slowly lower the outstretched arms. This downward movement may exacerbate the winging, and at a certain point as the arms descend the scapula will suddenly snap backward. Scapular winging is also discussed in Chapter 19. For a video of scapular winging, see http://www.youtube.com/watch?v=dfTeOnPclDE.
In the muscular dystrophies, particularly facioscapulohumeral (FSH) dystrophy, there is often weakness of all the shoulder girdle muscles, with prominent scapular winging, typically bilateral. If the examiner attempts to lift the patient by hoisting the elbows, upper arms, or axillae, the shoulders are pushed upward, alongside the head, while the trunk stays put; the patient is lifted “through the shoulder blades.” This is a useful method of demonstrating shoulder girdle weakness in children who cannot cooperate with formal muscle testing. Another manifestation of shoulder girdle weakness, seen most often in patients with myopathy, is a change in the position of the arms. Normally, as the arms hang at the sides, the thumb faces to the front. With shoulder girdle weakness, the scapula tends to slip laterally so that even at rest the shoulders tend to turn slightly anteriorly. This causes the entire arm to rotate internally, making the back of the hand rather than the thumb face anteriorly. Another effect, especially if there is also pectoral muscle atrophy, may be to produce a crease running diagonally from the anterior axillary fold toward the neck.
The Glenohumeral Joint
The principal movements at the glenohumeral joint are abduction, adduction, external and internal rotation, flexion, extension, and elevation of the arm. These movements are best appreciated as taking place in the plane of the body of the scapula rather than in the body as a whole.
The deltoid is the most prominent muscle in the shoulder region. It is supplied by C5 and C6 through the axillary nerve, a branch of the posterior cord of the brachial plexus. The deltoid has three portions: anterior, middle, and posterior. The middle deltoid and supraspinatus muscles, aided by the subscapularis and the upper part of the infraspinatus, abduct the shoulder. With deltoid contraction, the arm is abducted (raised laterally) to the horizontal plane. Further abduction, or elevation above the horizontal plane, is carried out by the associated action of the trapezius and the serratus anterior, which rotate the scapula and tilt the angle of the glenoid fossa upward. In the first 15 degrees, the abduction motion by the deltoid is aided by the supraspinatus, and the synergistic actions of the subscapularis, infraspinatus, and teres minor prevent the humeral head from translating upward. The posterior fibers of the deltoid also assist in extension and external rotation of the arm and the anterior fibers in flexion and internal rotation; but electromyography shows the deltoid is not very active in these movements.
The major function of the deltoid is tested by noting the ability of the patient either to abduct the arm through the range up to 90 degrees against resistance (Figure 27.9), or to hold the arm in abduction to the horizontal level, either laterally or forward (the elbow may be either flexed or extended), and to resist the examiner’s attempt to push it down. Testing both sides simultaneously helps the patient maintain balance and also helps in the comparison of strength on the two sides. With MRC grade 3/5 weakness, the patient can abduct the arm against gravity but not against significant resistance. With more severe weakness, the patient may lean in the opposite direction and raise the tip of the shoulder to aid in the attempt (trick movement). When active elevation to the horizontal plane is impossible, the passively abducted arm may be held up against gravity. With grade 2/5 weakness, the patient may be able to abduct the arm when lying flat but not when erect. In complete paralysis, no contraction of the muscle is possible. When weakness of the deltoid is due to a lesion of the anterior horn cells, brachial plexus, or axillary nerve, atrophy appears promptly and may be severe. This leaves the bulge of the acromion visible through the atrophic muscle belly, which simulates the appearance of shoulder dislocation. Because of myotomal overlap, isolated cervical root lesions do not cause the same degree of atrophy. In ALS or cervical spondylosis, fasciculations are often noted.
FIGURE 27.9 Examination of the deltoid. The patient attempts to abduct his arm against resistance; the contracting deltoid can be seen and palpated.
The supraspinatus helps abduct the shoulder through the first 15 degrees. The muscle belly lies in the supraspinous fossa of the scapula; its contraction can be palpated and sometimes seen when the arm is abducted less than 15 degrees against resistance (Figure 27.10). The supraspinatus is innervated primarily by C5 and C6 and by the suprascapular nerve, which arises directly from the upper trunk of the brachial plexus. Its tendon crosses over the shoulder joint to attach to the greater tuberosity of the humerus, forming one component of the rotator cuff (Chapter 47).
FIGURE 27.10 Examination of the supraspinatus. Contraction of the muscle fibers can be felt during early stages of abduction of the arm.








