46 Multiple Sclerosis
Pathology
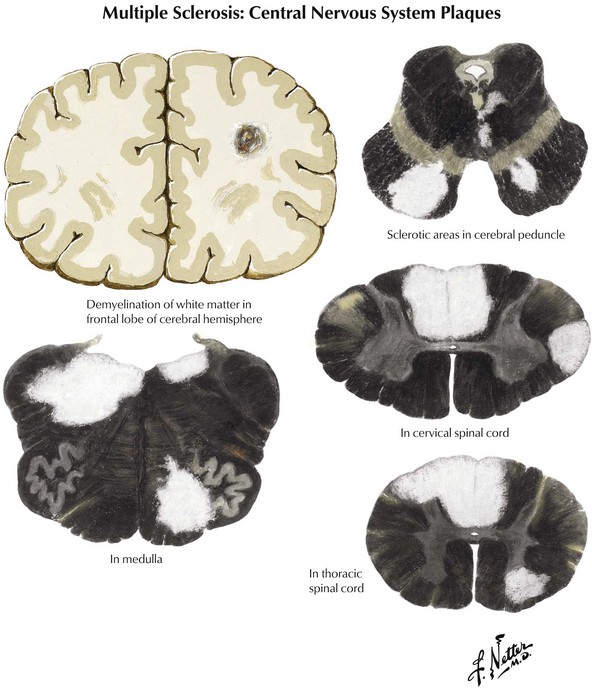
Coronal brain sections reveal changes similar to those noted on MRI, where variously sized MS plaques are apparent. Recently acquired lesions are pink and soft, whereas chronic MS lesions are gray, translucent, and firm (Fig. 46-1). It is often difficult to correlate the multiple lesions found at autopsy or by MRI throughout the neuraxis with a patient’s history. Sometimes classic MS plaques exist in patients who were never clinically suspected of harboring it.
Clinical Subtypes
Differential Diagnosis
Ocular
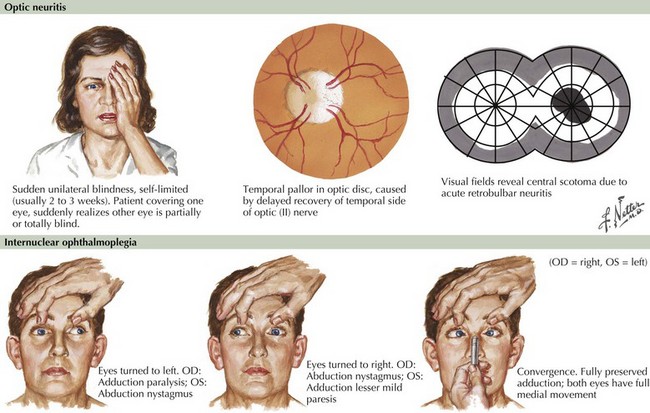
Blurred vision, likely a manifestation of acute optic neuritis, is a very common initial symptoms of MS. This may have great variability in degree from gross total unilateral blindness to a subtle change in visual acuity. Vision changes may also be related to a poorly expressed diplopia secondary to an INO, one of the most common neuro-ophthalmologic manifestations of MS (Fig. 46-2). In the first instance, the differential diagnosis includes any process affecting the retina or cornea, and in the second, the diplopia may be related to a pseudo-INO, mimicking MS. This is typical of myasthenia gravis. Sometimes a true INO secondary to a stroke may occur in older hypertensive patients.
When temporally associated with a myelopathy, this clinical presentation is referred to as Devic syndrome, or neuromyelitis optica (NMO). This is a humorally mediated autoimmune demyelinating disorder that is immunologically distinct from MS. It is characterized by an autoantibody that recognizes aquaporin 4 (AQP4), a water channel expressed on astrocyte podocytes. NMO may sometimes have a poorer prognosis than MS although on occasion it is more acutely responsive to immunosuppression or chemotherapy. This Devic syndrome does not typically benefit from first-line long-term MS disease modifiers (Chapter 47).
Inner Ear or Cerebellum
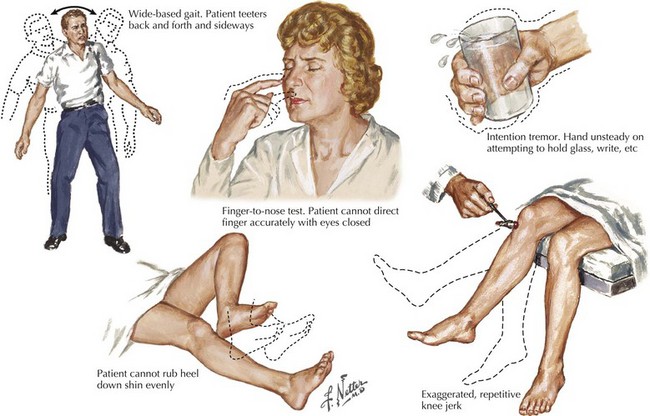
A vague feeling of unsteadiness, dizziness, and sometimes a whirling vertigo with nausea are frequent symptoms of MS. Precise definition of exactly what patients mean by “dizzy” is essential. Frequently, patients are in fact reporting a sense of dysequilibrium likely representing cerebellar dysfunction and less commonly reflecting vestibular pathways. Such patients typically demonstrate a broad-based gait, various signs of dysmetria, a tremor not seen in patients with a primary vestibular lesion, and often vertical nystagmus (Fig. 46-3).
Myelopathies
Sensations of tingling, tightness, pins and needles, and electric shocks are common MS symptoms. Relatively early in the disease course, some of these patients report an electric shock–like sensation that usually radiates down the back or arms, occurring spontaneously when the patient bends his or her neck. This is known as Lhermitte’s sign (Fig. 46-4). This most commonly occurs with MS patients but often the patient does not report this per se. Rather the skilled examiner is trained to ask about such as it is pathognomonic and indicative of spinal posterior column dysfunction. Lhermitte’s sign can be reported with almost any form of spinal cord disease, including spondylosis with significant cervical spinal stenosis, a space-occupying lesion, vitamin B12 (cobalamin) deficiency, or copper deficiency syndromes, especially in individuals who have had major gastrectomies or unusual diets, such as excess zinc that blocks copper absorption.