73 Myasthenia Gravis
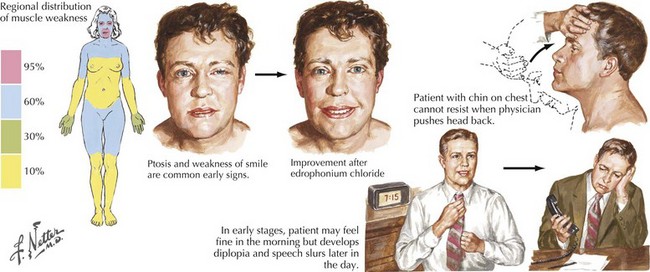
This vignette is typical of a myasthenia gravis (MG) patient with fatigable and fluctuating muscle weakness. MG almost always begins with ocular muscle weakness manifesting as ptosis, dysconjugate gaze, and eye closure weakness (Fig. 73-1). The symptoms of MG often spread to involve “bulbar” muscles, causing fatigable and fluctuating dysarthria, chewing weakness, and dysphagia. Respiratory, neck, and limb muscles can also become weak. An autoimmune basis for MG has been recognized since 1960. Overall, women are more commonly affected. Peaks of onset are seen in women in the second and third decades and for men in the fifth and sixth decades. The overall prevalence, estimated at 1 per 10,000, has increased over the past 40 years because of improved recognition, treatment, and survival.
Etiology And Pathogenesis
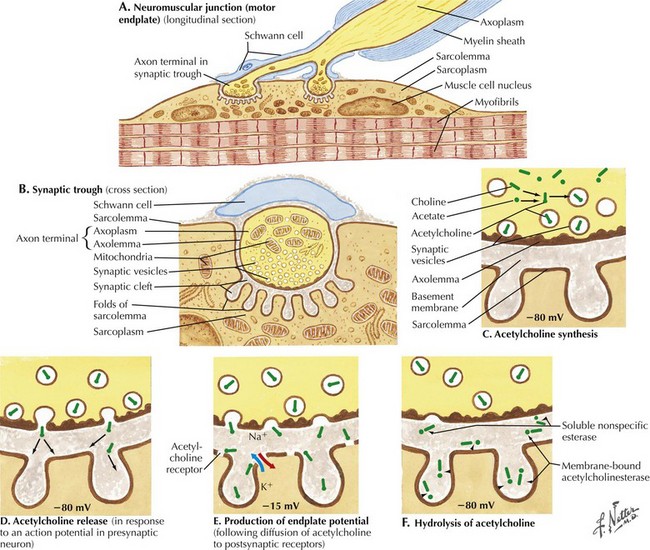
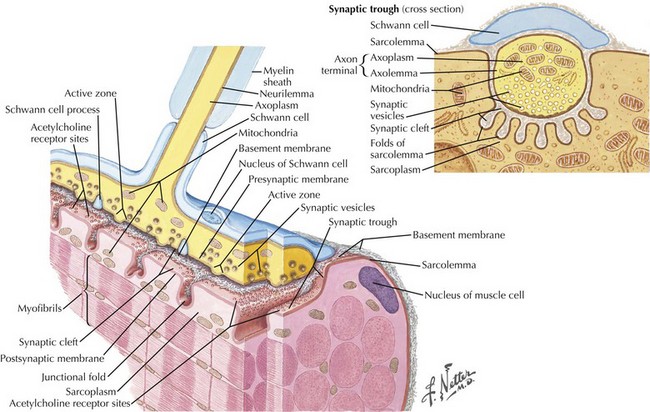
The most common cause of acquired MG is the abnormal development of antibodies to immunogenic regions (epitopes) on or around the nicotinic AChR of the postsynaptic endplate region at the neuromuscular junction (NMJ) (Figs. 73-2 and 73-3). These AChR antibodies trigger immune-mediated degradation of the AChRs and their adjacent postsynaptic membrane. The loss of large numbers of functional AChRs decreases the number of muscle fibers that can depolarize during motor nerve terminal activation, resulting in a decreased generation of muscle fiber action potentials and subsequent muscle fiber contraction. Blocking of neuromuscular transmission causes clinical weakness when it affects large numbers of fibers.
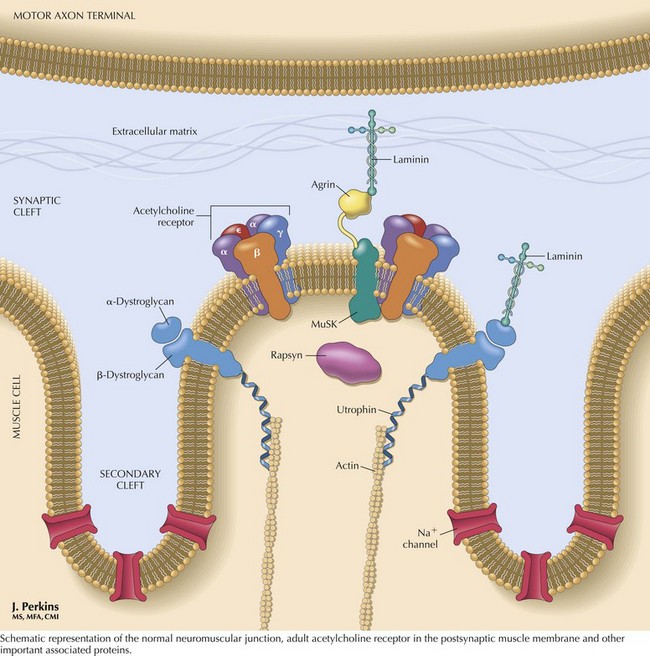
The nicotinic AChR contains five subunits arranged radially around a transmembrane ion channel (Fig. 73-4). The antibodies generated in MG are usually directed against the alpha subunit of the AChR. These antibodies may bind at or near the acetylcholine-binding site, directly preventing acetylcholine binding, or may alter receptor function through other mechanisms, such as increased receptor degradation or complement-mediated receptor lysis.
Clinical Presentation
Myasthenia gravis is typically classified as ocular, generalized, neonatal, congenital, or drug-induced. At presentation, weakness is confined to the ocular muscles in 80% of patients. Within 1–2 years, more generalized weakness develops in 85–90% of these individuals (see Fig. 73-1). In those few patients with primary ocular MG in whom bulbar or generalized weakness do not develop during the first 2 years, further progression to generalized MG is significantly less likely although it may occur as late as 8–10 years later (these patients are classified as having ocular MG).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree