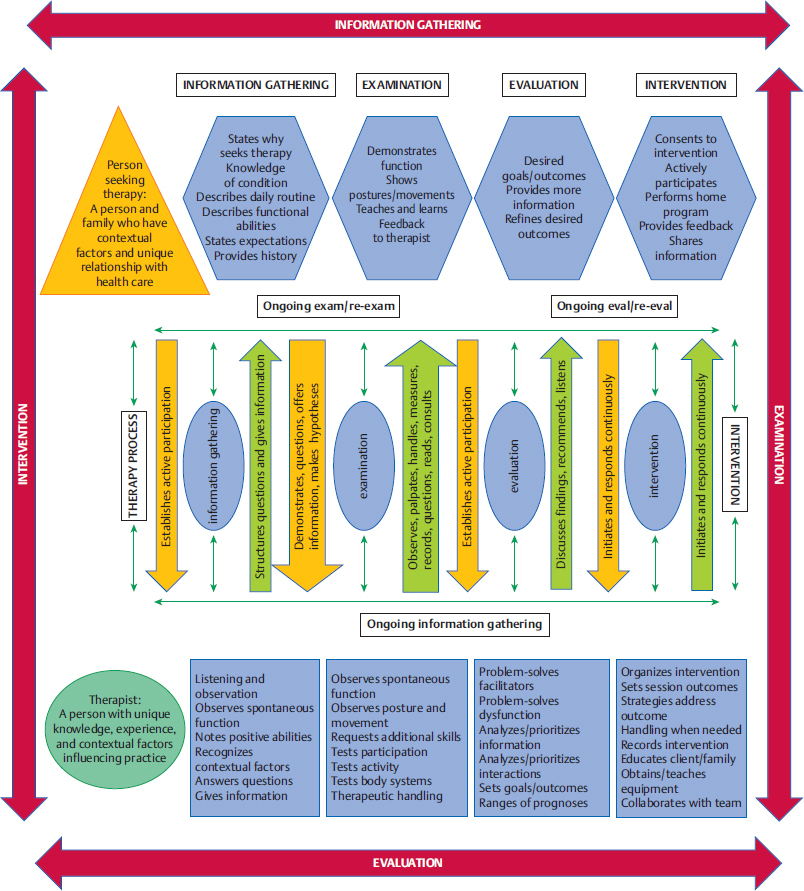
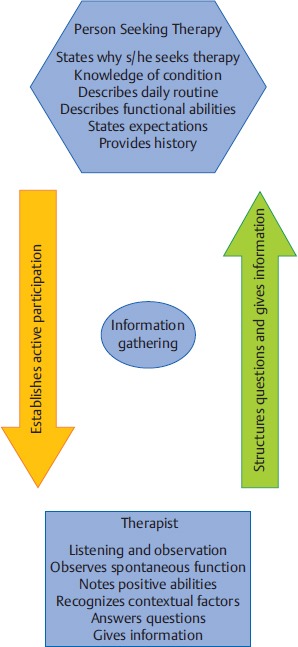
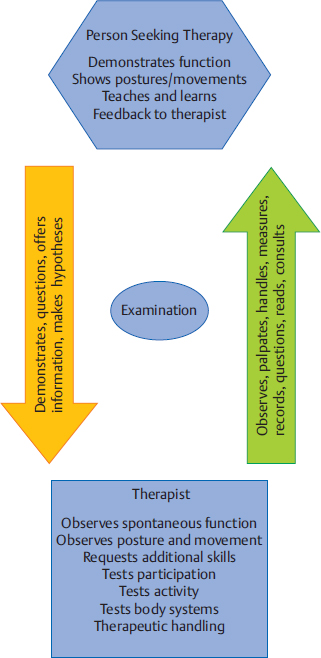
5 Neuro-Developmental Treatment Practice Model This chapter introduces and defines the Neuro-Developmental Treatment (NDT) Practice Model. It emphasizes the difference between models for clinical practice and theories that inform practice. The NDT Practice Model is unique in its emphasis on communication between the client/family and the clinician during all phases of the therapeutic relationship. It is also unique in its emphasis on the interweaving of all portions of the model. Learning Objectives By the end of this chapter the reader will be able to do the following: • Describe the purpose of the NDT Practice Model. • Define the difference between a practice model for clinical application and theories that inform practice. • Describe the client/family and the clinician’s roles in the therapeutic process using the NDT Practice Model during the following: • Describe the meaning of the statement, “The NDT Practice Model depicts the interwoven process between the client/family and clinician during all aspects of the therapeutic relationship.” • Describe what is meant by the statement, “Information gathering, examination, evaluation, and intervention often occur simultaneously and interweave.” Practice models provide a written description of the complexity of clinical practice for the purpose of analyzing, problem solving, and predicting functional outcomes of intervention. They describe and explain practice.1 Neuro-Developmental Treatment (NDT) is a philosophy with direct clinical applications to intervention; therefore, a practice model can be created. The NDT Practice Model (Fig. 5.1) shows how therapists who use the NDT philosophy gather, synthesize, and analyze information relevant to management of their clients. The practice model illustrates the complexity of clinical practice and the interrelationships of each component of the process. This model also shows descriptive and procedural knowledge that therapists need in their problem-solving process, including specific NDT philosophy. The explicit depiction of the relationship between a person seeking therapy and the therapist emphasizes the importance of collaboration in clinical practice using NDT. The NDT Practice Model illustrates the constant interrelationships of communicating, observing, thinking, analyzing, and actions that can move in any direction as the clinician and client interact. Information gathering, examination, evaluation, and intervention are components of practice that are interwoven processes rather than discrete and separate ones. All of these components occur in every session, not just initially or with formal updates. This model provides a constant interconnection among the client/family and therapist at all times. NDT also emphasizes that information gathering, examination, evaluation, and intervention occur simultaneously and constantly influence one another. Processes are not linear or even cyclical; rather, all information gathered during any part of practice informs all other processes. Clinicians who practice using the NDT Practice Model are licensed in the speech and language pathology profession or the physical or occupational therapy professions. Clinicians practice according to their state licensure practice acts in the United States and are governed by ethics codes and statements of practice from their professional associations. Canadian therapists are licensed in their provinces, and each profession also has practice laws and guidelines. The American Speech and Hearing Association (ASHA), the American Occupational Therapy Association (AOTA), the American Physical Therapy Association (APTA), the Canadian Physiotherapy Association, the Canadian Association of Occupational Therapists, and the Speech-Language & Audiology Canada organization all have statements about practice scope, guidelines, or frameworks. All currently recognize the International Classification of Functioning, Disability and Health (ICF) in their organization of these practice scopes, frameworks, and guidelines. In addition, the APTA Guide to Physical Therapist Practice2 shows a cycle of information gathering, examination, evaluation, and intervention as the means for interacting with patients and clients. The AOTA’s Occupational Therapy Practice Framework3 states that there is ongoing interaction among evaluation, intervention, and outcomes during the therapy process, and relates that to clients as individuals. The scope of practice described by ASHA4 follows the ICF model in its application to practice. However, none of these practice guidelines shows the constant interweaving of the information gathering, examination, evaluation, and intervention to the extent that the NDT Practice Model does. Theories relevant to clinicians who treat clients with neurological impairments consist of explanatory statements that make predictions about human functioning from many branches of science and the humanities. Theories take shape from research study results, experience, and creative thinking. Therapists use knowledge originating from motor control, motor learning, motor development, neuroplasticity, compensations in body systems, rehabilitation practice, cognition theories and development, language theories and development, psychology, and sociology theories to assist them with problem-solving skills related to intervention. Base knowledge from many theories, both descriptive and procedural, changes continuously with the knowledge we gain from research, experience in our professions, each person we treat, and our successes and failures with intervention. How a clinician understands and integrates the ever-changing base knowledge into daily practice depends on the practice model or models that the therapist uses. All clinicians use a philosophy and practice model, whether they are able to articulate it or not. Base knowledge informs their interactions with clients and is the basis for clinical hypotheses, outcomes identified, and how therapists interact with their clients. Those who practice using practice models other than NDT may interpret descriptive knowledge derived from theories and research studies or apply it procedurally in a different way than those who use the NDT Practice Model. Theories that support clinical practice are often confused with a clinical practice model. Changes in our understanding of human functioning derived from theories generated in disciplines of study may be viewed as an abandonment of a practice model rather than the necessary adjustments to changing information. A person may say, “You can’t just absorb every new thing that comes along and call it NDT. NDT isn’t everything, you know.” The mistake is that the speaker or writer is confusing a practice model with knowledge of the theories of human functioning that inform the base knowledge of any clinical practice. Current knowledge in the fields of motor control, motor learning, motor development, and neuroplasticity is found in Chapters 12 through 15. Therapists realize that information from these areas of study will undergo changes in theoretical understanding, refinement of ideas, and evidence from research studies. Therapists who practice using NDT seek constant information and evidence in the basic and applied sciences to integrate into the larger picture of the NDT Practice Model. In this text, case reports will serve the purpose of assisting therapists to deepen their knowledge of the hands-on application of NDT practice. Therapists learn procedural knowledge in many ways, beginning in their university education, and proceeding through NDT certificate courses, working with mentors, and through peer discussions and cotreatment sessions. However, the procedural knowledge specific to NDT is useful only within the entire scope of the NDT Practice Model. Procedures are tools only and can be used well only within the entire practice of NDT. The problem solving, synthesis, analysis, and relationship with the client and family are all critical in determining the selection and ordering of procedural knowledge (intervention strategies). The NDT Practice Model depicts the relationship of the person seeking therapy with the therapist along the continuum of the therapy process. There is a partnership in the communication between the client, family, and therapist at all times, with each having responsibility in the relationship of working toward meaningful outcomes. Information gathering (Fig. 5.2) may start prior to meeting directly with the person seeking therapy with verbal or written information provided by referral or by the client or other team members. If that is not the case, information gathering begins the moment the therapist meets the client, family, and other care providers. They provide their perspectives on why they seek services and what they hope the therapist can offer them. They may state their understanding and perspectives of the conditions for which they seek assistance. By listening carefully to the client and family, the therapist gathers this information in a nonjudgmental manner. This information is important to the therapist who uses the NDT philosophy of individualized care because the client’s reasons for seeking services apply directly to setting individualized outcomes. This active and reactive listening also helps establish rapport between the client and therapist. The therapist deepens an understanding of the client’s daily routine by asking questions that will enhance an understanding of the environmental conditions in which each activity is performed and how much and what type of assistance or support is required for daily activities. The therapist directs questions according to the profession he/she belongs to, while staying attuned to information that may lead to referrals to other team members. This attention to referral to other team members is a key component of NDT practice. An example of information gathering shows the interaction of a speech-language pathologist with a 10-month-old baby and her parents. The therapist might ask how often the baby nurses and how long each nursing session typically lasts, or how many ounces the baby drinks from a bottle. Who bottle-feeds the baby? Is there choking or coughing? What sounds does the baby make when awake? Do the sounds mean anything particular to the family? Are there positions or ways the family holds and supports the baby for these sounds or times of the day when the baby is more vocal? Does the baby use nonvocal communication with family members? How does the baby respond to unfamiliar people and situations? What would the family like the therapist to do to help the baby eat or communicate better or more? As the therapist asks specific questions and listens to the answers, as well as to spontaneous offerings of information, the therapist begins to formulate priorities about how to best examine the client. This assessment is based on many sources during information gathering—what the client has shown and described as abilities and inabilities in functioning, the emphases that the client and family place on desired outcomes, and the knowledge and beliefs about the conditions to be addressed during intervention. The therapist who uses the NDT Practice Model brings a context and background to intervention and other management, just as the client does. Although each therapist has his or her unique knowledge, therapists who practice using the NDT Practice Model value common sources of knowledge. During information gathering, they rely on the following: • Knowledge of the NDT philosophy, and the history and changes in NDT practice over the years. This knowledge includes the belief that people with disabilities and those living with conditions that impair functioning have value and worth. It also includes the belief that therapeutic intervention can positively influence life skills of people with disabilities and conditions that impair function. • Knowledge of theories of motor control, motor learning, and motor development. Knowledge of the causes and effects of compensatory postures and movements originating in various body systems. • Knowledge of a model of human functioning. Currently, the most widely used model is the ICF created and endorsed by the World Health Organization.5 • Knowledge and experience with a variety of neurological conditions that may impact functioning. Stroke, cerebral palsy, traumatic brain injury, and genetic disorders are historically the most common conditions NDT was developed to address. • Knowledge of growth, development, skill acquisition and loss over the life span, and how participation, activity, and body systems change both functionally and dysfunctionally as a result. • Knowledge of cultural diversity, family dynamics, human beliefs diversity, human values diversity, and ethics. • Knowledge of human behavior, specifically reactions to disability and illness. • Knowledge of human learning styles and how these may be affected by neurological impairments. • Skilled observation of participation, activity, posture and movement, and body systems within the typical contexts used by each client. The examination portion of the NDT Practice Model (Fig. 5.3) continues the communication process among the client, family, and therapist. Now the focus is on joint discovery and learning more about the specifics of the client’s functional participation and activity abilities and limitations. This individualized understanding of each client is one of the distinguishing hallmarks of NDT and is considered of utmost importance. A model of human functioning, such as the widely accepted ICF model (Fig. 5.4), is a useful tool for organizing the examination. The therapist records observations of the client’s participation abilities and restrictions and activity abilities and limitations; examines body structures and functions (i.e., single systems, such as neurological, musculoskeletal, integumentary, respiratory, sensory, cognitive, behavioral) for integrities and impairments; and hypothesizes about the origins of impairments caused by the interaction of more than one body system, such as posture and movement.
 Information gathering.
Information gathering.
 Examination.
Examination.
 Evaluation.
Evaluation.
 Intervention.
Intervention.
5.1 What Is a Practice Model?
5.2 The NDT Practice Model and Theories That Support It
5.3 Current Descriptive Knowledge Used in NDT Practice
5.4 Procedural Knowledge Used in NDT Practice
5.4.1 The NDT Practice Model: Overview
5.4.2 The NDT Practice Model: Information Gathering
5.4.3 The NDT Practice Model: Examination
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree