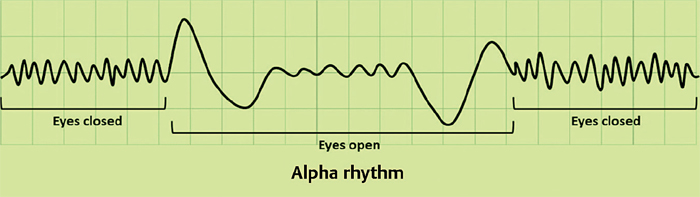
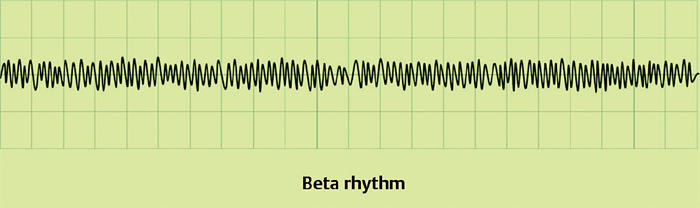
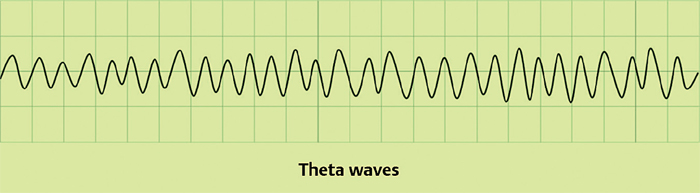
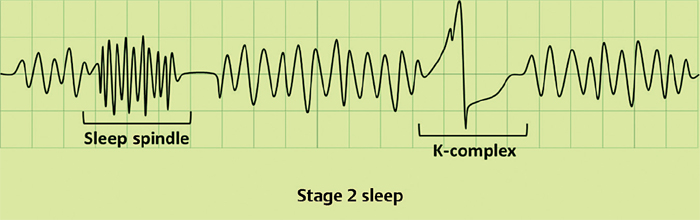
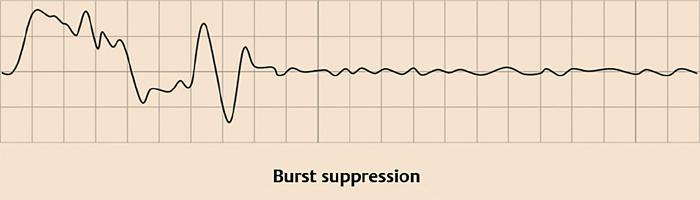
17 What is the normal rate of cerebral blood flow (CBF)? 50 to 55 mL/100 g/min1 Decreases in CBF below what level result in deficits of neural function? 23 mL/100 g/min2 What factors can increase CBF? Increases in paCO2 (acidosis) or serum H+, decreases in pH or paO2. How are body fluid levels regulated by the CNS? 1. ADH secreted from the supraoptic nucleus of the anterior hypothalamus decreases renal excretion of water. 2. The lateral hypothalamus increases water intake by the sensation of thirst. Both ways are activated or inhibited in response to decreases or increases (respectively) in serum osmolarity sensed by two circumventricular organs: the subforniceal organ and the vascular organ of the lamina terminalis. What does an EEG measure? The difference in voltage between two electrodes at a given time. By using multiple electrodes placed on the head or within the brain the EEG is able to record variations in the normal sinusoidal electrical activity that characterizes the cerebral cortex. Which cells are the primary contributors of the synaptic potentials measured in an EEG? Pyramidal cells What are some examples of extracranial EEG artifacts? Electrical activity of the heart (artifact may be seen to coincide with QRG deflection on ECG), eye blinking or eye movements, frontalis muscle contractions, extraocular muscle contraction, temporalis contraction with chewing What are alpha waves (the alpha rhythm)? Observed in an awake and resting adult with eyes closed. The rhythm is suppressed by eye opening or thought. Consists of parieto-occipital dominant 8 to 12 Hz sinusoidal waves with 25 to 75 μV amplitude.3 Fig. 17.1 Alpha rhythm What are beta waves (the beta rhythm)? Seen primarily in the frontal region of the brain. Seen during drowsiness, light sleep, and with mental activation. Consists of low-amplitude waves at 14 to 30 Hz.3 Reduced velocities (>50%) may suggest a focal gray matter abnormality. Fig. 17.2 Beta rhythm Waves with frequencies <8 Hz, including: 1. Theta waves: 4 to 7 Hz, seen with drowsiness and sleep, also present in normal, awake young adults and with focused concentration 2. Delta waves: <4 Hz, seen during slow-wave sleep Fig. 17.3 Theta waves What are vertex waves? 200-ms diphasic, transient, synchronized waves seen bilaterally in sleep stages 1, 2 and 3 Describe the EEG changes observed during the different stages of sleep. Mnemonic is “BATS Drink Blood”: Awake, alert adult: Beta rhythm Awake, resting (eyes closed) adult: Alpha waves (and vertex waves) Stage 1 sleep: Theta waves Stage 2 sleep: Sleep spindles (and K complexes) Slow-wave sleep (stages 3 and 4): Delta waves rapid eye movement (REM) sleep: Beta rhythm Describe the EEG changes seen in stage 2 sleep. EEG background is similar to stage I sleep (progressive slowing of background frequencies is seen). In the foreground, sleep spindles (transient, sinusoidal 12- to 14-Hz frontal activity of varying amplitude) and K-complexes (high-amplitude, diphasic waves).4 Fig. 17.4 Stage 2 sleep Give some examples of focal EEG abnormalities. Focal slow wave activity (indicating focal neuronal damage), focal spikes or sharp waves (which imply excessive neuronal discharge and may indicate a focal seizure), or focal suppression of voltage (indicating focal damage of nonelectric tissue) Give some examples of generalized EEG abnormalities. 1. Diffuse slowing of background rhythm (nonspecific indicator of disturbance of cerebral function bilaterally such as in an encephalopathy) 2. Frontal intermittent rhythmic delta activity (FIRDA): encephalopathies due to toxic or metabolic etiologies5 3. Occipital intermittent rhythmic delta activity (OIRDA): may be seen with generalized epilepsy6 4. Synchronized spikes (seen in generalized idiopathic epilepsy), or complete absence of activity (seen in cortical death) What are epileptiform discharges? Epileptiform discharges may be seen between seizure episodes (interictally) or during an acute seizure episode (ictally) and may be divided into spikes and sharp waves. Spikes are single waves with duration <70 ms that stand out from background activity. A sharp wave is similar to a spike but with a duration 70 to 200 ms. Spikes and sharp waves are typically followed by a slow wave. As with other EEG abnormalities, epileptiform abnormalities may be generalized (as in the generalized 3-Hz spike and dome pattern seen in petit mal seizures) or focal (such as a focal single spike followed by a slow wave, which may be seen in focal or secondary generalized epilepsy). What are activation techniques? Give an example of an activation technique. Stimuli applied to the EEG subject in an effort to augment EEG abnormalities. Examples include photic stimulation, hyperventilation (causes cerebral vasoconstriction) and sleep deprivation. Other stimuli that may increase seizure frequency include emotion, fever, loud noises, and trauma. A pattern suggesting a severe bilateral cerebral dysfunction. May also be induced iatrogenically for neuroprotection. Consists of stereotyped bursts occurring every 2 to 10 seconds separated by intervals of suppression (where no electrical activity is seen). Fig. 17.5 Burst suppression What is an electromyogram (EMG)? A clinical study of the electrical activity of muscle fibers using surface or needle electrodes. Electrical activity is measured during needle insertion, during periods of muscle rest (spontaneous activity), and during periods of minimal or maximal voluntary muscle contraction.7,8 What criteria are used to evaluate the motor unit action potential? Maximum peak-to-peak amplitude, rise time of the initial positive spike/peak, duration of the action potential and number of phases What are the constituents of the motor unit? The alpha motor neuron whose cell body lies in the ventral horn of the spinal cord, its axon, and all motor fiber innervated by the cell.9 Between which diagnoses can EMG help differentiate? 1. Radiculopathy 2. Entrapment neuropathy 3. Neuritis 4. Nonneurological condition What are some common patient complaints for which EMG may be ordered? 1. Pain 2. Weakness 3. Numbness/paresthesia What is nerve conduction velocity? The speed of action potential conduction within a nerve, calculated by determining the distance from neuron cell body (ventral horn) to needle and dividing by the latency of response onset. What is insertional activity? Electrical activity measured during insertion of needle into muscle tissue. Also known as injury potentials due to their origin from disruption of cell membranes by the needle. This activity is normal up to 50 ms following needle movement. Continued burst firing after needle insertion or manipulation is abnormal and may indicate denervation (e.g., radiculopathy), myotonic, or inflammatory conditions. Decreased amounts of normal insertional activity may indicate atrophic, fibrotic or edematous muscle tissue. In what pathological situations would insertional activity be increased? 1. Hyperirritable muscle cell membrane due to inflammation (e.g., myositis) 2. Denervation 3. Electrolyte imbalance 4. Trauma to muscle tissue or ischemia Describe the electrical activity seen in normal resting muscle (spontaneous activity). Normal muscle does not exhibit electrical activity at rest, and thus any spontaneous activity at rest is considered pathologic (unless the needle is placed in an endplate area of a muscle, in which case normal spontaneous activity may be generated by irritation of terminal axons by the needle). Fig. 17.6 normal muscle: at rest (spontaneous activity)
Neurophysiology
17.1 Basic Concepts
17.2 EEG Interpretation
17.3 EMG Interpretation
Neurophysiology
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree






