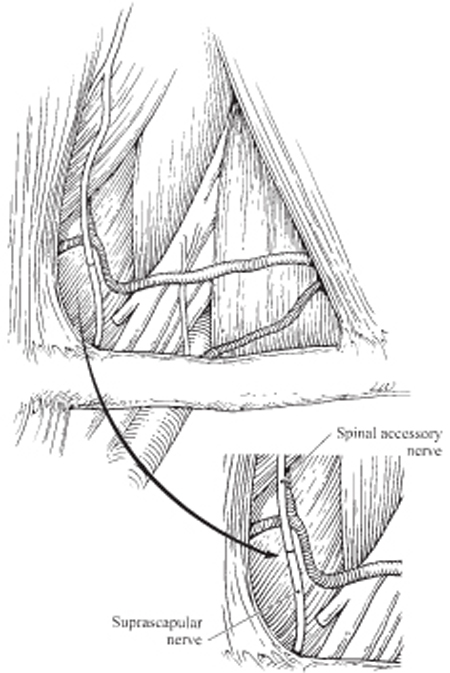
11 Neurotization in Brachial Plexus Injury The patient is a 19-year-old male student who was involved in a motor vehicle accident 8 months prior to evaluation. The patient was a front-seat passenger with seat belt restraint and suffered a left brachial plexus injury. No other significant injuries were sustained by the patient; the driver of the car suffered minor contusions only. The patient was initially managed at a local emergency room elsewhere and after stabilization released to the care of a neurologist. The brachial plexus injury was diagnosed as a pure C5/C6 root and/or upper trunk injury, and conservative management with physical therapy was instituted. Initial electrical studies confirmed the diagnosis of a complete upper root injury. Four months after injury, the patient’s neurological status and electrical studies were unchanged, and the patient was referred to a neurological surgeon in the Northwest for management. The evaluation at this time added magnetic resonance imaging (MRI) of the left brachial plexus that showed pseudomeningoceles of C5 and C6 roots. In conjunction with ongoing complete denervation electrically and on physical examination, the patient was advised that he had avulsions of the C5 and C6 nerve roots, which were unreconstructable. He was discharged with a prognosis of permanent paralysis of deltoid, biceps, and spinati muscles. Three months later, 7 months following injury, the patient was referred to us for evaluation and management. The patient presented with a primary complaint of left shoulder and biceps paralysis 8 months following a traumatic injury to the brachial plexus. General physical examination showed a healthy-appearing white male with obvious deformity of the left upper extremity but no other injuries. Severe wasting of spinati, deltoid, and biceps muscles was apparent. Muscle strength grading was 0/5 British Motor Grade (BMG) for left supraspinatus and infraspinatus, deltoid, and biceps. Triceps graded at 4+/5, and results below the elbow were 5/5 throughout. Sensory examination was significant for numbness in the C5 distribution and decreased sensibility in the C6 area of the forearm. A Tinel sign was present in the left supraclavicular fossa. Upper brachial plexus injury, with C5 and C6 nerve root avulsions The supraclavicular brachial plexus consists of five spinal nerves (C5 to T1) and three trunks (upper, middle, and lower). C5 and C6 combine to form the upper trunk, C7 continues as the middle trunk, whereas C8 and T1 contribute to the lower trunk. Just above and behind the clavicle, each trunk branches off to an anterior and posterior division. In addition to the divisions, the branches of the upper trunk include the suprascapular nerve, which innervates the supra- and infraspinatus. The posterior division of the upper trunk provides primary input to the posterior cord that is destined for the axillary nerve, hence deltoid muscle innervation and sensory input from the lateral upper arm. It also supplies (via the radial nerve) innervation to the brachioradialis and supinator muscles. The anterior division of the upper trunk provides the essential contribution (via the lateral cord) to the musculocutaneous nerve and therefore biceps innervation and sensation to the lateral forearm and thumb. Although the clinical picture was consistent with brachial plexus root avulsions, there are no definitive noninvasive testing procedures to confirm this diagnosis. The differential diagnosis therefore must include lesser degrees of nerve injury from Sunderland grades 1 through 5. Grades 1 through 3 will typically show some return of function, either clinically or on electrical testing, by 3 to 4 months and therefore were not applicable to this case. The situation of an extraforaminal injury or rupture grade 4 or 5 was still possible, and definitive management would therefore include operative exploration and testing of the injured brachial plexus at the supraclavicular and infraclavicular levels. The presence of pseudomeningoceles on MRI, in our experience, has not been equal to intraoperative somatosensory evoked potential (SEP) measurement in confirmation of nerve root avulsion injury. The working diagnosis in this patient therefore was rupture or avulsion injury of the C5 and C6 nerve roots with a plan of surgical exploration and definitive reconstruction of the nerve injuries. Electromyographic (EMG) testing throughout the postinjury period consistently showed denervation of muscles supplied by C5 and C6. Fibrillation potentials were observed and no motor units were seen. MRI testing revealed pseudomeningoceles at C5 and C6. All testing was confirmatory of root avulsions of C5 and C6 following traumatic injury to the left brachial plexus. The patient was brought to the operating room for exploration and functional reconstruction. The exposed upper plexus was scarred but no large neuromas were identified. Intraoperative EMGs revealed no continuity of the C5 and C6 nerve roots through the musculocutaneous, axillary, and suprascapular nerves to the corresponding muscles. SEP testing revealed no conduction through the contralateral cerebral cortex, supporting the diagnosis of a preganglionic injury (avulsion). Middle and lower plexus anatomy was essentially normal. Although there have been a few descriptions of surgical reconstruction of brachial plexus avulsions by reimplantation of the stumps directly to the spinal cord, the results have been poor to modest, and alternative functional reconstructive methods are preferred by us. After completion of intraoperative nerve testing, execution of planned nerve transfers proceeded. The suprascapular nerve was isolated at the distal upper trunk and internally neurolysed within the upper trunk to gain length for the transfer. The spinal accessory nerve was then dissected within the loose connective tissue anterior to the trapezius muscle and followed distally as it supplied the lower two thirds of the trapezius. The surgical transfer was then completed with microsurgical repair using 10–0 nylon epineurial stitches (Fig. 11–1). The use of distal spinal accessory nerve as donor for suprascapular function is conceptually sound because synergistic function is transferred and minimal morbidity is seen. The nerve supply of the upper third of the trapezius, however, must be carefully protected to avoid significant shoulder dysfunction. The next element for reconstruction, the axillary nerve, is best approached through an axillary approach, which allows exposure in the area of the quadrangular space. Direct electrical stimulation confirmed complete absence of conduction in the three elements of the axillary nerve. A vessel loop was placed around the nerve and attention was turned to the roof of the axilla where the branches of the brachial plexus are in transition from the cords. After the posterior cord/radial nerve was exposed in its entirety, examination of its structure clearly revealed two groups of fascicles that corresponded to functional units of the radial nerve. The more inferior group supplied the triceps muscle and these were now separated by careful intrafascicular microdissection. One triceps fascicle was selected as donor to the axillary motor nerve and protected with a vessel loop. The selected triceps fascicle was sufficient to cover the deltoid and teres minor components of the axillary nerve (Fig. 11–2). Coaptation was performed with 10–0 nylon epineurial stitches.
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Anatomy
Anatomy
 Differential Diagnosis
Differential Diagnosis
 Diagnostic Tests
Diagnostic Tests
 Surgical Treatment
Surgical Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



