Nonoperative Management and Treatment of Spinal Injuries
Mark L. Prasarn
Glenn R. Rechtine II
The morbidity and mortality of injuries to the spine have been known since antiquity. Nonoperative methods have been a mainstay of care for such injuries since ancient Egypt. Even with modern-day surgical techniques available, the majority of spinal injuries should be managed nonoperatively with the expectation of healing of the spine without any of the inherent risks of surgery. In most spinal injuries, a good functional outcome and no long-term disability can be expected with nonoperative care.
Nonsurgical treatment is used in all cases of spinal injuries. Nonoperative treatment techniques are employed at the initial evaluation and management of a patient at the scene of the accident. In the vast majority of cases, nonsurgical principles are extended as a definitive treatment plan. In addition, during every step of diagnosis and treatment, strict adherence to principles of immobilization must be followed to minimize motion to the injured spine and prevent neurologic injury or deterioration.
The objectives of nonoperative management of spinal injuries are the same as those of operative treatment. These include (a) preservation of neurologic function, (b) improvement in neurologic deficit if already present, (c) reduction of spinal deformity and maintenance of acceptable alignment, (d) minimize loss of spinal mobility, and (e) achieving a healed and stable spinal column.
AT THE SCENE
According to advanced trauma life support (ATLS) protocol, life-threatening compromise to airway, breathing, and circulation should be promptly addressed. Although the greatest risk for spinal cord injury occurs at the time of high-energy impact, neurologic deficits can develop thereafter during treatment. In 1983, Podolsky reported that up to 25% of spinal cord injuries had been caused by or aggravated after the patient had come under medical care (1). Immobilization of the injured spine is the key to preventing such catastrophic decline.
The on-scene care of spine trauma patients has dramatically improved over the past several decades. Extrication and transport of trauma patients with immobilization techniques and adherence to ATLS protocols for resuscitation have been credited for this improvement. ATLS protocol mandates that injured patients be assumed to have a spinal injury and rigid immobilization employed. At the scene, the patient should be immobilized with a cervical collar, head immobilization device, and spine backboard.
AT THE HOSPITAL
The patient will arrive in the emergency department on a backboard with a cervical collar in place. In the face of a global instability, motion will still occur in spite of all attempts at rigid immobilization. The patient should be moved on and off the backboard as few times as possible until the stability of the spine can be adequately assessed. For most injuries, the collar provides an increased level of stability. However, it does not provide complete immobilization (2). With a complete ligamentous disruption, there is minimal effect of the collar itself. The person stabilizing the spine is much more significant in restricting motion (3).
Moving the patient off the backboard for computerized tomography should be coordinated so that the brain, spine, chest, abdomen, pelvis, sinus, orbits, or any other appropriate study is obtained in one trip to the scanner and one movement off and on to the backboard.
The risk of decubitus is directly proportional to the length of time on a backboard. In a spinal cord injury patient, 8 hours on a back board is associated with a 100% likelihood of a decubitus (4). The patient should be moved from the board as soon as possible. At all times, appropriate spine immobilization must be continued.
Contrary to all available evidence suggesting that the log roll is an ineffective and potentially dangerous technique for spine immobilization, it is still used almost universally. In fact, studies conducted prior to 2004 showed dramatic and unacceptable motion with a log roll (5). Recently, many studies have reevaluated this controversial subject. When compared to any other method of transfer, the log roll maneuver has been shown to cause more segmental
motion at the unstable, injured segment (6, 7, 8, 9, 10, 11, 12 and 13). Lift and slide techniques are far superior since they tend to create less motion at the injured segment (10).
motion at the unstable, injured segment (6, 7, 8, 9, 10, 11, 12 and 13). Lift and slide techniques are far superior since they tend to create less motion at the injured segment (10).
IMAGING STUDIES
Following the review of the initial CT scan, another assessment of spinal stability can be performed. If there is a need for closed reduction of a dislocated segment, this should be performed expediently in the awake and alert patient. Serial neurologic exams are performed during such a reduction maneuver. If the patient is obtunded or reliable neurologic exams are impossible, then an emergent MRI should be obtained prior to attempted reduction to rule out significant disk herniation (14).
In the absence of a facet dislocation and presence of significant spinal injury, the appropriateness of an MRI scan must be determined. The spinal motion necessary to transfer the patient on and off the MRI table must be kept in mind when deciding how necessary this imaging modality is. The strongest argument for an MRI is a neurologic deficit that is not explained by the injury seen on the CT scan. If the patient has an unstable injury that requires surgery identified clinically or by other imaging studies, it is not necessary to obtain an MRI just to assess the dorsal ligamentous complex.
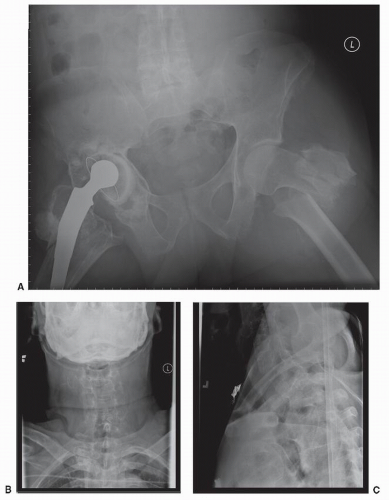
Anteroposterior and lateral radiographs of the cervical, thoracic, lumbar, and sacral spine are standard imaging studies obtained in the high-energy impacted patient with suspected spinal injury. Distracting injuries can often mask symptoms secondary to significant spinal injury, and meticulous assessment of the spine must always be performed (Figs. 44.1, 44.2 and 44.3). It is necessary to image the entire spinal column due to a 10% incidence of noncontiguous spinal injuries (15). Specific injury mechanisms
and fracture patterns should trigger the treating team to search for commonly associated nonspinal injuries. Flexion-distraction injuries are highly associated with potentially life-threatening intra-abdominal injuries, and these must be ruled out. Patients with transverse process fractures at L5 have a 61% incidence of a pelvic fracture (16). Falls from a height with resulting burst fractures are often associated with significant lower extremity fractures, in particular those of the tibia and calcaneus.
and fracture patterns should trigger the treating team to search for commonly associated nonspinal injuries. Flexion-distraction injuries are highly associated with potentially life-threatening intra-abdominal injuries, and these must be ruled out. Patients with transverse process fractures at L5 have a 61% incidence of a pelvic fracture (16). Falls from a height with resulting burst fractures are often associated with significant lower extremity fractures, in particular those of the tibia and calcaneus.
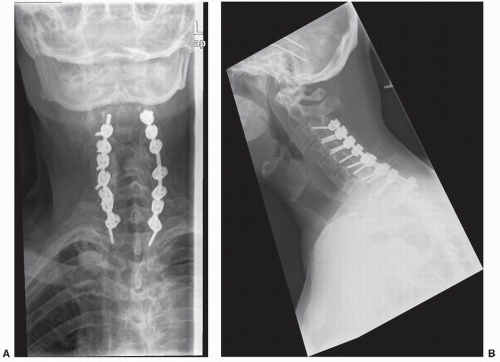
 Figure 44.2. Further imaging of the cervical spine in the same patient. A,B: Sagittal and coronal computerized tomography (CT) images demonstrating the ankylosed cervical spine and injury at C6-C7. |
CLOSED REDUCTION OF THE CERVICAL SPINE
Decompression of the spinal cord through closed reduction should be performed as soon as the patient can medically tolerate it. Closed reduction is a means of reducing cervical spine deformity, indirectly decompressing neural elements, and providing stability. It has been shown to be safe and can lead to dramatic improvement in neurologic status if performed within the first few hours following injury. In animal studies, Carlson showed that decompression within 3 hours showed better and quicker neurologic recovery (17). There have been small series of patients with no cord function who were reduced in an emergent manner and immediately began to recover (18). Although this is anecdotal, it is extremely important. The timing question is answered after consideration of the risk-benefit ratio between waiting to obtain a prereduction MRI and proceeding directly with reduction.
There is considerable controversy regarding the order of the reduction and obtainment of an MRI in an acute cervical spine dislocation. Eismont et al. reported on a series of six patients who demonstrated, roentgenographically, herniation of an intervertebral disk with marked protrusion of disk material into the spinal canal following subluxation or dislocation of a cervical facet. In the first patient in this series, no myelogram or CT scan was performed, and the patient awoke with complete quadriplegia following dorsal open reduction and internal fixation. The etiology identified following a myelogram and ventral decompression surgery was an extruded intervertebral disk. The authors recommended obtaining an MRI in all patients prior to attempted closed reduction and definitive surgery (19, 20 and 21). Several other cases with neurologic deficits after open reduction under general anesthesia have been reported (20,21). There have also been reports of progression of neurologic deficits during traction, while the patient was awake and participating, that resolved (22).
The group from Thomas Jefferson University advocates performing immediate closed reduction in the patient that is awake and can facilitate reliable serial neurologic examinations. Vaccaro et al. published their series of 11 patients who underwent successful awake closed reduction without any neurologic worsening. In their series, it was demonstrated that two patients had herniated disks prior to reduction, and another five had herniated disks following reduction (14). An attempt to determine the effect of disk herniation during closed reduction was put forward by Darsaut et al. with a series of 17 patients who had a cervical dislocation reduced under MRI monitoring. They demonstrated that at least as a research tool this was possible (23).
A commonly used algorithm is based on the patient’s neurologic status. If the patient is unable to participate reliably in the physical examination, then an MRI is obtained as expediently as possible. If the patient has a mild radicular deficit, the disadvantage of getting an MRI is the time required to get the study. If the patient has a significant spinal cord injury, the risk is that the cord compression will remain present for a longer period of time. Therefore, if the patient has minimal or no neurologic dysfunction, an MRI should be obtained. If the patient has an ASIA A, B, or C injury and is able to cooperate with the reduction and serial neurologic exams, consideration should be given to an immediate, rapid reduction. In this situation, the MRI would be obtained after reduction.
REDUCTION TECHNIQUES
Reduction of a cervical spine dislocation must be performed under image guidance and in a very controlled manner. Gardner-Wells tongs are applied with the pins placed 1 cm above the pinna of the ear just below the equator of the head. Pins are tightened to 3.6 kg of pressure. This is indicated once the precalibrated indicator pins protrude a measured amount. If using weights over 25 kg, titanium pins and MRI-compatible tongs will not be sufficient. Weights of over 60 kg have been used safely for closed reduction of such injuries (24). In such instances, stainless steel pins or two sets of tongs must be used. Another option includes the use of a halo that provides four titanium pins to distribute the forces over more pins. The major disadvantage of stainless steel pins is their MRI incompatibility.
It is recommended that the initial weight applied be no more than 4.5 kg. Initially, using more weight can be catastrophic if the patient has an unrecognized instability such as an occipital cervical dislocation. After applying the initial 4.5 kg, a neurologic examination should be performed followed by a radiograph. Additional weight should be added incrementally until reduction is obtained. Serial exams are performed to look for any neurologic deficit following each addition of weight, as are serial roentgenograms. After reduction, the weight should be decreased to a minimum needed to maintain the reduction. Continue routine exams and stabilize the instability when medically appropriate. Pulmonary and skin issues can be addressed with use of a kinetic treatment table until surgery.
DEFINITIVE TREATMENT
Closed treatment remains the standard of care for most spinal injuries. There are few situations where surgical intervention is clearly required. These include skeletal disruption in the presence of a progressive neurologic deficit and purely ligamentous injuries in a skeletally mature patient. Such ligamentous injuries require spinal fusion to obtain stability. It should also be noted that the presence of a neurologic injury is not an absolute indication for surgery. The remaining gamut of spinal injuries can be treated without surgery. Closed treatment options include bed rest, halo apparatus, external orthosis, or a cast. Many
unstable injuries can be treated with an initial period of bed rest in a kinetic treatment bed followed by bracing and mobilization once some early healing has been achieved. The absence of significant pain should be the clinical indicator of when the patient is ready to be cleared from the Rotorest bed and mobilized. Upright films in the external orthosis should be obtained to confirm that the spinal column is stable at this point (Tables 44.1 and 44.2).
unstable injuries can be treated with an initial period of bed rest in a kinetic treatment bed followed by bracing and mobilization once some early healing has been achieved. The absence of significant pain should be the clinical indicator of when the patient is ready to be cleared from the Rotorest bed and mobilized. Upright films in the external orthosis should be obtained to confirm that the spinal column is stable at this point (Tables 44.1 and 44.2).
TABLE 44.1 Treatment Options for Cervical Injuries | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TIMING OF SURGICAL INTERVENTION
In the face of acute spinal cord injury, there still remains ongoing debate over the appropriate timing of traction or surgery. It is difficult to demonstrate improvement in neurologic function from acute surgical intervention (25). Complete cord injuries and neurologically intact patients are very likely to remain neurologically unchanged with appropriate surgical or nonoperative care. Incomplete lesions typically improve with either surgical or nonsurgical care. Late surgery with decompression of the spinal canal in incomplete cord injuries has been shown to improve neurologic function even several years following the traumatic event (26,27). In the acute setting, there is sparse and unconvincing evidence supporting early surgery. Surgery for the purpose of spinal canal decompression in a neurologically intact patient is difficult to defend as there are several series showing dramatic spinal canal remodeling over time in patients with and without surgery (28, 29, 30, 31, 32, 33, 34 and 35).
TABLE 44.2 Treatment Options for Thoracic and Lumbar Injuries | |||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
UPPER CERVICAL INJURIES
Occipitocervical injuries are most often fatal and are typically found postmortem. When a patient is encountered with such an injury, the treating physician must be vigilant to make the diagnosis and ensure the patient’s survival. Initially, such injuries should be meticulously immobilized on a backboard with a collar and the head secured with sandbags and tape. Atlantooccipital disassociation is then stabilized with a halo vest until definitive surgical stabilization is performed (36). It should be noted that traction for type II injuries (axial distraction) can be catastrophic and is strictly contraindicated. The injury is treated with dorsal occipital-cervical fusion with at least 3 months of halo vest immobilization. Occipital condyle fractures and Jefferson’s or atlas ring fractures are typically managed with an orthosis or a halo (37).
Odontoid fracture treatment depends on the injury itself. Many can be treated with a rigid orthosis or halo vest. Type I and type III fractures typically heal uneventfully and have a good prognosis without surgery. Transverse type II fractures through the waist of the odontoid have a high associated nonunion rate and are therefore the ideal fracture for surgical treatment. A dorsally displaced odontoid fracture is more likely to be treated with surgery (38, 39, 40, 41, 42 and 43). Polin reported a series of patients treated with a rigid collar as opposed to a halo. There were more nonunions with the type II fractures. However, there was no statistically significant difference between the orthosis used (43). Chronic odontoid nonunions in the elderly can often be followed and may not require surgical intervention. In a series of persistent nonunions, there was no progression of atlantoaxial instability or neurologic deficit or myelopathic symptoms during the follow-up period (44).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree