Chapter 109 Oral Appliances for Sleep-Disordered Breathing
Abstract
In 2006, the American Academy of Sleep Medicine published updated practice parameters on the use of oral appliance therapy in the treatment of OSAH.1 These guidelines stated that oral appliances are indicated as therapy in patients with simple snoring and mild to moderate OSAH in patients who prefer oral appliances, or those who refuse or have failed CPAP. Oral appliances may also have a role as an alternative therapy for severe OSAH when other therapies have failed. Many prospective studies have been published, including randomized, controlled clinical trials with comparisons with continuous positive airway pressure (CPAP), different oral appliance designs, surgery, and placebo.2–17 With evidence of effectiveness from such studies, there is a growing basis for expanding the indications for oral appliance therapy in the management of OSAH.
Types of Appliances
There are two main appliance groups in common clinical use: mandibular repositioning appliances (MRAs) and tongue-repositioning devices. MRAs, also known as mandibular advancement splints (MASs) or mandibular advancement devices (MADs), are the focus of this chapter because they are more widely used in clinical practice and have a greater evidence base. These devices are anchored to part or all of the dental arch so as to induce protrusion of the mandible (Fig. 109-1). Many designs are available, but they generally fall into either one-piece (monobloc) or two-piece (dual-bloc) configurations (Figs. 109-2 to 109-5). They are usually customized to the dentition, although off-the-shelf varieties also exist. Tongue-advancing appliances hold the tongue in a forward position without advancing the mandible. Some tongue-advancing appliances, such as the tongue-retaining device (TRD), hold the tongue forward in a bulb, using suction created by displacement of air when the tongue is advanced into it (Fig. 109-6). TRDs may also be custom made or off the shelf.

Figure 109-2 The Klearway adjustable oral appliance.
(Courtesy of Great Lakes Orthodontics, Ltd, Tonawanda, NY.)

Figure 109-3 An adjustable Herbst appliance.
(Courtesy of Great Lakes Orthodontics, Ltd, Tonawanda, NY.)

Figure 109-4 The Monobloc appliance.
(Courtesy of Dr. Konrad Bloch, University of Zurich, Switzerland.)

Figure 109-5 The SomnoDent mandibular advancement splint.
(Courtesy of SomnoMed Ltd, Crows Nest, Australia)
Mechanism of Action
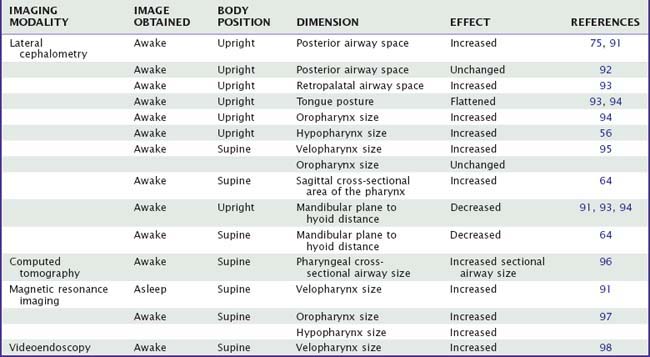
Current evidence suggests that the pathogenesis of OSAH reflects reduced upper airway size and altered upper airway dilator muscle activity. Oral appliances can improve upper airway patency during sleep by enlarging the upper airway, by decreasing upper airway collapsibility (e.g., improving upper airway muscle tone), or through both mechanisms.17a The effects of oral appliances on upper airway size vary among studies, and these differences are likely related to variations in imaging techniques used (e.g., cephalometry versus computed tomography [CT]), the study methods (evaluation during wakefulness versus during sleep), the subject’s body position (supine versus upright), the different types of appliances, and the amount of protrusion. However, they are consistent in that most imaging studies suggest that MRAs have a direct effect on position of the mandible and increase upper airway cross-sectional area. Furthermore, such studies have generally observed more-complex changes in airway shape and size than might be initially predicted from simple anterior displacement of the mandible. For example, many studies have identified a predominant change in the lateral dimension, at the level of the velopharynx, highlighting the complex anatomic and functional linkages between segments of the pharynx. The effects on upper airway size are summarized in Table 109-1.
Simple anterior movement of the tongue or mandible during wakefulness can increase cross-sectional airway size at all levels in persons with and without OSAH.18 Passive mandibular advancement during general anesthesia (achieved by a jaw thrust maneuver) stabilizes the upper airway by increasing airway cross-sectional area in both the retropalatal and retroglossal area and reducing its collapsibility (i.e., more-negative intraluminal pressure is required to close the upper airway).19 Similarly, mandibular advancement with an MRA reduces closing pressure (e.g., more-negative intraluminal pressure is required to close the upper airway), reflecting decreased upper airway collapsibility.20
Effects of MRAs on upper airway muscle activity have not been well studied. A study using an MRA reported that upper airway muscle tone increased except in the postapnea period, when genioglossus tone was lower.21 Another study also found augmentation of genioglossus tone with mandibular advancement during wakefulness in adults without OSAH.22 Although the presence of MRA in the mouth has effects on upper airway tone through stimulation of oral afferent pathways, these effects are insufficient to reduce apnea, and mechanical mandibular advancement is required for the appliance to improve OSAH.7
TRDs appear to affect genioglossus muscle activity in patients with OSAH (either awake or asleep),23,24 but effects of this type of device on other upper airway muscles have not been evaluated. A TRD worn during sleep reduced the apnea–hypopnea index (AHI).24 When the TRD was worn without tongue advancement (no bulb), the AHI decreased and there was increased peak genioglossus activity, measured just before the airway opened at the end of residual obstructive events. The mechanism for this effect and its significance is not certain, but increased genioglossus tone might contribute to upper airway reopening.
Clinical Outcomes
Since the turn of the century there has been a substantial increase in the quantity and quality of research evaluating the efficacy and effectiveness of oral appliance therapy.25,26 The strengths of these newer studies include the use of inactive oral devices or tablets (placebo) as the control treatment, more-stringent definitions of treatment outcome, direct comparisons to CPAP, and an increased focus on health outcomes. A comprehensive review of oral appliance therapy was published in 2006,25 along with updated practice parameters for their use.1
Polysomnographic Variables
There is strong evidence from randomized, controlled trials that MRAs are effective in preventing or significantly reducing the number of obstructive breathing events and arousals and in improving arterial oxygen saturation across the full spectrum of OSAH severity. Oral appliances have been associated with a reduction of the AHI to fewer than 5/hr in 36% to 50% of patients,7,27,28 and the proportion of patients achieving an AHI less than 10/hour has ranged from 30% to 70%.25 Using the most liberal definition of success, namely a reduction of more than 50% in AHI, an average of 65% of patients achieve this outcome.25 With regard to oxygen saturation parameters, the improvements noted with oral appliances are of a smaller magnitude than the changes in AHI. In general, studies have identified improved minimum oxygen saturation, but rarely to normal levels. Some studies have reported improved sleep architecture, with increases in rapid eye movement (REM) sleep.7 Similarly, reductions in arousal index have been reported.7,27,28 It seems likely that differences in oral appliance designs have an impact on the extent to which these parameters are affected. Although these differences are yet to be fully established, it is thought that minimization of bite opening and impingement on tongue space are important design features.
Upper airway resistance syndrome (UARS) is part of the spectrum of sleep-disordered breathing in which subtle degrees of inspiratory flow limitation leads to sleep fragmentation and OSAH symptoms.29,30 The role of oral appliance therapy in this specific subgroup of patients has received little attention. In a prospective trial on 32 patients with UARS, Yoshida found statistically and clinically significant improvements in arousal index (average number of arousals per hour slept), oxygen saturation, sleep efficiency, and subjective and objective sleepiness, suggesting that MRAs may be helpful in the treatment of UARS.31
Efficacy of the TRD has been less well studied than efficacy of the MRA. In 1982, Cartwright and Samelson reported their initial experience with the TRD in 20 patients.32 Among the 14 of the 20 patients who underwent polysomnography before and with the TRD, there was a reduction in AHI of approximately 50%, even though patients wore the TRD only half the night.32 Subsequent uncontrolled studies of the TRD reported a 69% to 80% success rate.33,34 The TRD was found to be more effective in patients who were younger, who were less obese, and those with positional apnea (apnea that is more severe in the supine position).33 A tongue-stabilizing device was assessed in a pilot study of six patients and was found to reduce snoring, but the reduction in AHI was of borderline statistical significance.35 This device is based on the bulb component of the TRD, and because it does not cover the dentition, it is an off-the-shelf product.
Snoring
Snoring, with or without coexistent OSAH, is prevalent, and oral appliances have a potentially important role in the management of this problem. Uncontrolled studies, using bed-partner reports, suggest that snoring is reduced in the majority of patients.36 Similarly, a placebo-controlled study also reported improvements in subjective snoring.17 Studies using objective measures of snoring frequency and intensity confirm a reduction in both parameters, compared to an inactive oral control device.7,27 Reductions in snoring frequency are of the order of 40% to 60%, and mean snoring intensity reduces by about 3 dB.7,27 This represents a clinically important reduction in noise level and is reflected by the resumption of co-sleeping in a significant percentage of couples after oral appliance treatment.37
Daytime Sleepiness
The majority of studies suggest that oral appliance therapy improves subjective daytime sleepiness as measured by validated questionnaires such as the Epworth Sleepiness Scale (ESS),38 with evidence from placebo-controlled studies indicating a modest reduction in the ESS score in the order of 2 points.27,39 The effect on objective sleepiness has received limited attention. In one placebo-controlled, study the mean sleep latency on the multiple sleep latency test (MSLT) after 4 weeks of MRA treatment was significantly improved by an average of 1.2 minutes compared with an inactive control oral device.27 Two other randomized, controlled studies evaluated objective sleepiness using the maintenance of wakefulness test (MWT) over treatment periods of 8 to 12 weeks and found no difference in treatment response between CPAP and oral appliance. One study13 showed similar improvement and the other found no change with either treatment.39 In the latter study, Barnes and coworkers did observe improvements in subjective sleepiness despite the lack of improvement in MWT, and poor treatment compliance may have been a factor.39 In summary, successful oral appliance therapy clearly improves subjective sleepiness, although the impact on objective sleepiness is less clear. Nevertheless, the outcomes are similar to those reported for CPAP.
Neurocognitive Outcomes
Only a few studies have addressed the impact of oral appliance therapy on neuropsychological functioning. Engleman and colleagues compared CPAP to oral appliance intervention in a randomized study and found no significant difference between treatments in effect on cognitive performance.13 A randomized, controlled study using an inactive oral device as a control found that active treatment with the MRA resulted in small to moderately enhanced psychomotor speed but no significant change in other neurocognitive measures.40 In another randomized, controlled study comparing oral appliance, CPAP, and tablet placebo for mild to moderate OSAH, oral appliance therapy improved tension anxiety, divided attention, and executive functioning, but CPAP was superior in improving psychomotor speed and other aspects of mood state.39 These somewhat divergent results highlight the difficulty of directly comparing neurocognitive outcomes between different studies due to differences in methodology and interpretation.
Driving performance is an important neurocognitive outcome that may be adversely affected by OSAH. A number of studies have examined the effect of CPAP treatment on driving simulation performance, but there has been little assessment of oral appliances in this regard. A randomized parallel study comparing an oral appliance and CPAP reported similar improvements in driving simulator performance over a period of 2 to 3 months.41
Cardiovascular Outcomes
Randomized controlled and uncontrolled studies have identified a modest reduction in blood pressure with oral appliance therapy.39,42–44 In one study, compared with a placebo oral device, 4 weeks of active MRA treatment produced a mean reduction in awake systolic blood pressure of 3.3 mm Hg and diastolic blood pressure of 3.4 mm Hg.42 In another study, comparing 3-month treatment periods with CPAP, oral appliance, and tablet placebo in patients with mild to moderate OSAH, oral appliance therapy, but not CPAP, was associated with a small reduction in nocturnal diastolic blood pressure (approximately 2 mm Hg).39 More recently, intermediate cardiovascular endpoints have also been explored. A 1-year follow-up study using a Herbst MRA found normalization of endothelial function and markers of oxidative stress, despite incomplete resolution of OSAH,45 calling into question the notion that cardiovascular benefits are only achieved with complete resolution of OSAH. These early data suggest that the control of OSAH by an oral appliance produces a beneficial effect on blood pressure and intermediate cardiovascular endpoints (e.g., endothelial function) similar to that of CPAP.
Quality of Life
Data regarding the effects of oral appliance therapy on quality of life are somewhat conflicting. A randomized, controlled study found that compared to a tablet placebo, MRA treatment improved quality of life as measured by the Functional Outcomes of Sleep Questionnaire (FOSQ) mean score and social outcome domain, and also by the SF-36 overall health score. The magnitude of improvement was similar to that found with CPAP.39 In contrast, another randomized, controlled study reported that well-being as assessed by the SF-36 scores for health transition and mental component were significantly better with CPAP compared to oral appliance therapy.13 In both studies, the assessment included treatment intervals that were shorter than 3 months.
In a longer-term study, Walker-Engstrom and colleagues evaluated quality of life in a randomized, controlled trial of an MRA versus uvulopalatopharyngoplasty (UPPP).46,47 After 1 year of follow-up, vitality, contentment, and sleep scores were significantly improved in both groups, but the UPPP group demonstrated significantly greater contentment than the oral appliance group. Further work is required to clarify the impact of long-term oral appliance therapy on quality of life.
Comparison of Oral Appliance Designs
A number of studies have compared different MRAs or MRA designs. One study evaluated a fixed-position appliance and a modified device in 24 patients with mild OSAH and found that the device that protruded the mandible was more effective in reducing the AHI than the device that minimally opened the vertical dimension without mandibular protrusion.4 Some patients had an increase in AHI using either device. In a randomized, controlled crossover study the AHI was less than 10 in 75% of patients with a monobloc appliance (see Fig. 109-4) and in 67% of patients with the dual-bloc appliance (see Fig. 109-3). Both devices reduced sleepiness and snoring, but patients preferred the monobloc. One randomized crossover study specifically evaluated the effect of vertical opening on the efficacy of a MRA by comparing 4 mm or 14 mm of interincisal opening at the same degree of mandibular advancement.8 Both MRAs had similar efficacy in terms of reducing snoring and AHI and improving sleepiness, but there was a trend to more jaw discomfort with the greater (14 mm) incisal opening. Overall, the patients preferred the appliance with less incisal opening for treatment.8
In another randomized crossover study of two distinct MRAs (appliances differed in materials, the amount of vertical opening, and the type of retention) set at approximately 75% of maximum protrusion found that both MRAs improved symptoms including snoring, sleepiness, and sleep quality. The MRA made of hard material with more vertical opening had more side effects and was less effective at improving OSAH.11
In a crossover study comparing two types of MRA with differing coupling mechanisms for 3 months each, similar improvements in AHI and subjective daytime sleepiness were noted.48 Another study evaluated two different amounts of mandibular protrusion, 75% or 50%, with an MRA in 86 men with severe OSAH.15 There were no more side effects with further protrusion. The MRA set at 75% reduced the AHI to less than 10 in 52% of patients, whereas the MRA set at 50% reduced the AHI to less than 10 in 31% of patients.
A study comparing the efficacy of an off-the-shelf thermoplastic (boil and bite) MRA versus a custom-made monobloc MRA found the latter to be far superior, suggesting the need for caution in using off-the-shelf thermoplastic devices as a therapeutic option or as a screening tool to find good candidates for MRA therapy.49
Comparison with Nasal CPAP
In the first randomized, controlled crossover study of oral appliance therapy, the investigators compared the efficacy, side effects, compliance, and preference between a fixed-position boil-and-bite MRA and CPAP in patients with mild to moderate OSAH (AHI 15 to 40).2 Treatment success (defined as reduction in AHI to 10 events or fewer with relief of symptoms) for the MRA was 48% and for CPAP was 62%. The MRA was well tolerated, with fewer side effects than CPAP, but some patients (24%) were unable or unwilling to use the MRA because of poor retention (ability to keep the oral appliance in place in the oral cavity) or discomfort. The MRA reduced snoring in most patients in reduced daytime sleepiness. Compared with the oral appliance, patients were less satisfied with CPAP. The authors concluded that a simple fixed-position appliance was an effective treatment in some patients with mild to moderate OSAH and was associated with fewer side effects and greater patient satisfaction than CPAP.
Since then, there have been a growing number of randomized, controlled trials comparing oral appliances to CPAP.18,39,50–52 These studies vary in their design, inclusion criteria (including severity of OSA), definitions of severity and treatment response, treatment interval, number of dropouts, the MRA’s design, and the measurement techniques used (e.g., portable home monitoring versus in-laboratory polysomnography). Collectively however, they indicate that CPAP is superior in reducing the AHI and improving oxygen saturation, but not arousal index, sleep architecture, or objective sleepiness.53,54
Despite the overall superiority of CPAP over oral appliances, patients in most of the studies preferred the oral appliance, raising important implications for adherence to treatment and effectiveness in the clinical setting. In terms of symptoms, particularly daytime sleepiness (subjective and objective), no substantial differences have been identified between CPAP and oral appliance treatments.53,54 This raises the important possibility that the health effects of both treatments are similar in magnitude, as a result of the superior efficacy of CPAP being offset by its inferior compliance relative to oral appliances. Further research is required to evaluate this possibility.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree