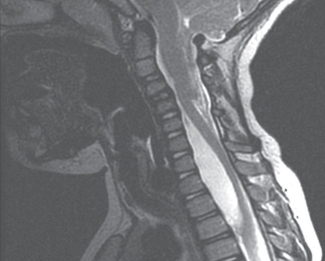
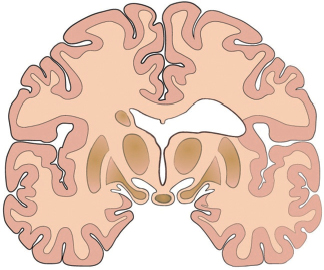
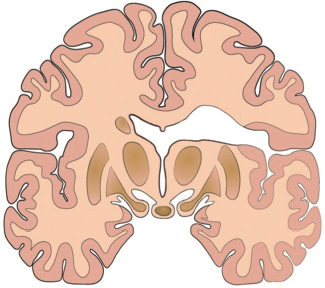
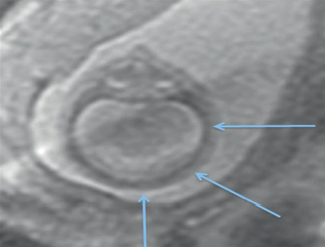
72 What are arachnoid cysts composed of? CSF-like fluid surrounded by an arachnoidal membranous wall What do they look like? In general, they are unilocular, transparent or translucent, and the adjacent dura is blue-tinged from the CSF. Are there different types? Yes; congenital, or “true,” cysts are located in the loose trabecular layer of the arachnoid, whereas those following trauma, or “secondary,” are mostly in the subarachnoid space. Why do they form? Abnormal CSF flow during development causes cyst formation. Where are they most commonly located? Sylvian fissure and middle fossa Do they appear in other locations? Yes, cerebellopontine (CP) angle, quadrigeminal cistern, retrocerebellar area, sellar and suprasellar areas True or false: Arachnoid cysts have high malignant potential. False; most are asymptomatic and benign. They account for what percentage of nontraumatic intracranial mass lesions? ≤1% What is the male-to-female ratio? 2:1 What is the most commonly diagnosed scenario? A left-sided middle fossa cyst in a young male What are some neuroanatomical characteristics of suprasellar cysts? Hypoplasia of the corpus callosum, optic nerves, optic chiasm, and fornix. Note: Large cysts can cause compression of the pituitary stalk and gland, and on imaging can seem to originate from inside the third ventricle due to invagination. What are the neuroanatomical characteristics of middle fossa cysts? Optic hypoplasia, microphthalmia, medial displacement of the ICA, medial and superior displacement of the MCA, venous aberrations What are some neuroanatomical characteristics of giant posterior fossa cysts? Elevation of the tentorium, straight sinus, and torcular Herophili When do they present? Usually in childhood (around 6 years of age), sometimes in adulthood What is the presentation of midline and posterior fossa cysts? Usual signs and symptoms of hydrocephalus What is the presentation of middle fossa cysts? Bulging skull, proptosis, visual loss, extraocular movement palsies, facial numbness, seizures, EEG abnormalities, developmental delays, behavioral and memory problems, subdural hematomas What is the presentation of suprasellar cysts? Isosexual precocious puberty, growth hormone deficiency, various visual field defects, neurobehavioral defects, “bobble-head doll” syndrome (uncommon, associated with cysts in close proximity to third ventricle) What is the presentation of intrasellar cysts? Headache, endocrine imbalances, visual field defects, older average age of presentation What is the presentation of convexity cysts? Seizures, dysphasia What is the presentation of CP angle cysts? Tinnitus, hearing loss, vertigo, facial motor and sensory loss, ataxia (can be mistaken for Meniere’s disease) What is the presentation of retroclival or cervicomedullary arachnoid cysts? Progressive spastic quadriparesis What complications can arise in association with arachnoid cysts? Subdural hygroma, intracystic, and subdural hematomas True or false: The associated anomalies are the result of pressure exerted by the cyst on the surrounding structures. True How do arachnoid cysts differ from Dandy-Walker malformation? Arachnoid cysts are not usually associated with systemic syndromes EXCEPT for autosomal-dominant polycystic kidney disease. What imaging modalities are best to study the cysts? Noncontrast CT, MRI (especially for smaller cysts and posterior fossa lesions), CT ventriculogram and cisternography (gold standard to show communication between arachnoid cysts and subarachnoid spaces), ultrasound (for in utero diagnosis and postnatal monitoring), PET and SPECT, EEG (for correlation of seizure foci with cyst location) How do you treat them? No treatment (just observation) for most cysts, especially if they are small and asymptomatic What are the considerations for treatment? Asymptomatic versus symptomatic, risk of subdural hematoma, risk of repetitive head trauma (athletes), developmental delays and behavioral disorders (adverse developmental effects from pressure exerted by cyst) What are the main surgical treatment options? Cyst shunting, open fenestration, endoscopic fenestration What types of cyst shunting are available? Cystoperitoneal shunting, cystoventricular shunting (if there is no hydrocephalus), cyst-subdural shunting What are the advantages and risks of shunting? Advantages: facility, short operative time, minimally invasive, low blood loss Risks: infection, shunt failure, shunt dependency What is an open fenestration? A craniotomy with open cyst fenestration into the basal cisterns Should open fenestration be the first option if there is a reasonable chance of success? Yes Which types of arachnoid cysts are best treated with open fenestration? Middle fossa, CP angle, and retrocerebellar cysts True or false: As much of the outer cyst wall as possible should be resected in open fenestration. True; this increases the chances of permanent free communication with the subarachnoid space. What are the advantages and risks of open fenestration? Advantages: controlled bleeding, visualization (and thus protection) of structures Risks: postoperative hematoma, neurological deficit, adhesion and inflammation, subdural hygroma Which types of arachnoid cysts are best treated with endoscopic fenestration? Deep arachnoid cysts (quadrigeminal, suprasellar) and intraventricular cysts What are the advantages and risks of endoscopic fenestration? Advantages: less invasiveness, shorter operative time, no long-term complications and risks associated with shunting Risks: uncontrolled bleeding, smaller fenestration than with a craniotomy (should aim for at least 1 cm) Are there any other surgical techniques to treat arachnoid cysts? Yes; stereotactic drainage, stereotactic instillation of intracavity radioisotopes What are the pertinent surgical considerations? If hydrocephalus accompanies the cyst, do not perform ventricular shunting without decompressing the underlying arachnoid cyst. Fenestration should be established in two locations because it allows for a second patent fenestration should one of them close. What are the possible outcomes? • No change in size (asymptomatic patients usually stay asymptomatic; symptomatic patients usually stay symptomatic) • Spontaneous diminution in size or disappearance in the presence or absence of trauma • Increase in size • Resolution of acute symptoms following surgery • Persistence of chronic symptoms due to longstanding compression • Complete eradication of the cyst not accompanied by clinical improvement of symptoms What does the word neurenteric signify? That the cyst is endodermal in origin True or false: Neurenteric cysts are a common congenital lesion. False; they rarely account for spinal masses (1%) and are even rarer intracranially. True or false: Neurenteric cysts are more common in males than in females. True; the male-to-female ratio is 2:1.1 Where along the spine do they most commonly occur? Lower cervical and upper thoracic Are they extradural or intradural? Most are intradural and extramedullary, though some are extradural and some intramedullary. Are they associated with any other spinal malformations? Yes; spina bifida (anterior or posterior), fused vertebrae, and hemivertebrae What do they look like? Light colored with varying wall thickness, filled with clear or white liquid or mucin Are there any pertinent histologic stains? Yes; mucin-secreting epithelial cells result in a positive periodic acid-Schiff (PAS) What is the pathogenesis behind the formation of neurenteric cysts? Possibly the split notochord theory, though it cannot be applied to intracranial neurenteric cysts Are they benign or malignant? Benign Irritability, neonatal syncope, infantile paraplegia, torticollis; in adolescence, localized or diffuse pain in the back, neck, or trunk exacerbated by positional changes and increased intrathoracic pressure What is the best imaging study option? MRI What are the typical MRI findings? On T1 the cyst is hypointense with possible high-intensity contents. On T2 the cyst is hyperintense. What is the preferred treatment? Surgical removal of the cyst Why is complete resection unlikely for neurenteric cysts? Because of adhesion to the spinal cord or nerve roots What is the postoperative pharmacological management? • IV morphine and midazolam for pain management • Perioperative antibiotics Are there any alternative treatments options? Broad fenestration of the cyst wall Can a remaining portion of the cyst lead to recurrence? Yes, although symptoms manifest after several years What are the special considerations for laminectomies performed on pediatric patients? Replacement of the laminae and possible use of a back brace to discourage kyphosis What are neuronal migration disorders (NMDs)? A group of developmental brain disorders that arise from disrupted migration of neurons during development, leading to cortical dysplasia2 What is the normal process of neuronal migration? After differentiation from stem cells into neurons or glials cells in the lining of the ventricular zones, they migrate radially (using radial glial fibers as guides) toward the pial surface and organize themselves in an “inside-out” fashion (older neurons deeper in the cortex and younger neurons located more superficially) according to an intricate signaling pathway.2,3 What are the different types of NMDs? • Lissencephaly/subcortical band heterotopia • Cobblestone complex (lissencephaly type II) • Heterotopia • Schizencephaly • Polymicrogyria (late neuronal migration/early cortical organization) What are the main clinical manifestations of NMDs? Mental retardation and seizures2 What are the cortical abnormalities in lissencephaly? • Diffuse cortical thickening (10–20 mm instead of the normal 2.5–4 mm) • Four layers instead of six • Agyria (no convolutions) or pachygyria (some convolutions) True or false: Subcortical band heterotopia (SBH) is considered to be a mild form of lissencephaly. True; the white matter contains bands of gray matter of differing widths that run parallel to both hemispheric cortices. Mutations in what genes are associated with lissencephaly? • LIS1 → autosomal, most cases of classic lissencephaly • DCX (XLIS) → x-linked, most cases of subcortical band heterotopia (SBH) What is the incidence of lissencephaly? 12 in every 1 million births What determines onset and severity? Which brain lobes are involved and the quantity and magnitude of misplaced gray matter What is the clinical presentation of lissencephaly? • Normal head size at birth → microcephaly within the first year • Mental retardation • Epilepsy • Hypotonia → hypertonia How is lissencephaly treated? • Proper nutrition • Management of aspiration episodes • Control of seizures What is the prognosis of a patient with lissencephaly? Most succumb to aspiration pneumonia and sepsis within 10 years. How is cobblestone dysplasia (lissencephaly type II) different from classic lissencephaly? Instead of neurons failing to migrate to the cortex, they go through the cortex into the subpial space and form “cobblestones” on the surface of the brain. Although there is cortical thickening, there is no cortical lamination as in classic lissencephaly. How does this happen? α-Dystroglycan is not glycosylated, so there are gaps in the glia limitans (pial surface lamina) that let the neurons pass through. This loss of function is thought to underlie which three genetic disorders? • Walker-Warburg syndrome • Fukuyama-type congenital muscular dystrophy • Muscle-eye-brain disease How are neuronal heterotopias characterized? Pockets of normal neurons located anywhere between the germinal zones and subcortical white matter caused by disturbances of neuronal migration along the radial glial cells True or false: Subependymal, or bilateral periventricular nodular, heterotopia (BPNH) is manifested by gray matter nodules deposited along the lining of the lateral ventricles and projecting into the ventricular spaces. True False; it is seen mostly in females because BPNH is transmitted in an X-linked fashion and is therefore lethal in males. What gene has been linked to BPNH? FLNA; it encodes filamin A, which connects actin filaments to glycoproteins and is a vital component of neuronal migration. How does BPNH present? Epilepsy, intractable seizures, higher likelihood of normal development How are the three types of subcortical heterotopia differentiated? Differentiated based on the form that the ectopic tissue takes: • Multiple nodules • Curvilinear ribbons • Mixture of deep nodular regions with curvilinear areas in the periphery When and how do patients with subcortical heterotopia present? Within the first decade of life: weakness, spasticity, hyperreflexia, seizures True or false: Intelligence is at the normal level in patients with heterotopia. True, except for those with marginal glioneural heterotopia How is heterotopia treated? Antiepileptics and surgical removal of seizure foci for intractable seizures What is known about the etiology of schizencephaly? Not established, but theories include: • Loss of neuronal and glial proliferation • No induction of neurons to migrate from the ventricular zone • Ischemic damage to glial fibers • Disorders of early cortical organization By what abnormality is schizencephaly characterized? Cerebral clefts (lined by polymicrogyric cortex) in the perisylvian region resulting in direct communication between the lateral ventricle and subarachnoid space. Clefts are either • open-lipped (walls separated) or close-lipped (walls apposed), and • unilateral or bilateral. Fig. 72.2 Unilateral closed-lipped (type I) schizocephaly (coronal view). Fig. 72.3 Unilateral open-lipped (type II) schi zocephaly (coronal view). Which type of cleft has the worse prognosis? Bilateral and open-lipped: • Severe developmental delays • Microcephaly • Hydrocephalus • Spastic tetraparesis What about patients with close-lipped schizencephaly? Hemiparesis or motor delay, but mild/moderate to no cognitive problems4 What other conditions are often seen with schizencephaly? • Gray matter heterotopia • Absent septum pellucidum • Agenesis of corpus callosum • Septo-optic dysplasia 80% of schizencephaly patients develop what kind of seizures? Focal seizures True or false: Open-lipped schizencephaly presents earlier than close-lipped schizencephaly. True, at around 3 years old How does the cortex appear in polymicrogyria? Thick, zero to four layers, many small irregular gyri with shallow sulci True or false: Most cases of polymicrogyria are familial. False; most are sporadic. Is polymicrogyria commonly associated with other developmental brain disorders? Yes, and it often coexists with schizencephaly. What is the most common polymicrogyria syndrome? Bilateral perisylvian polymicrogyria • X-linked • Cognitive impairment • Epilepsy • Pseudobulbar signs (dysarthria, dysphagia) In syndromic polymicrogyria, why are the clinical symptoms more predictable than in isolated polymicrogyria? Because in syndromic polymicrogyria both hemispheres are affected symmetrically and the topology of the affected brain areas is discrete and continuous, so the resulting clinical symptoms are similar in affected patients True or false: The clinical signs and symptoms in isolated polymicrogyria do not correspond to the affected brain region. False What is the prognosis of a patient with polymicrogyria? Depends on severity and location What is it? It is a cephalic disorder in which the forebrain of the embryo fails to develop into two hemispheres. What is the incidence rate? 1 out of 250 conceptions5 What is the live birth survival rate? 1 out of 16,0005 Is there a gender preference? Yes; females have twice the birth survival rate of males. What is the pathogenesis? Disruption of the prechordal mesoderm during neurulation in turn interrupts normal neural induction and regional patterning True or false: Environmental factors influence the occurrence of HPE. True; such teratogens include smoking, alcohol, CMV infection, antiepileptics, retinoic acid, and maternal diabetes Is there a genetic component? Yes; autosomal dominant with a penetrance of 80%, although manifestation is most likely multifactorial requiring several hits5 Have any relevant genes been identified? Yes; sonic hedgehog, TGIF, ZIC2, and SIX3, among others How is the spectrum of HPE classified? From most to least severe: Alobar HPE—absence of hemispheric midline division, leading to the existence of a single ventricle and the absence of the corpus callosum and olfactory bulbs and tracts.4 It is usually associated with severe facial anomalies such as cyclopia. Semilobar HPE—the anterior hemispheres are fused, whereas the posterior hemispheres have some degree of separation; only the splenium of the corpus callosum is identifiable. Lobar HPE—midline cleavage is absent only in the rostral-ventral forebrain with a normal or hypoplastic corpus callosum. *MIH (middle interhemispheric variant, or syntelencephaly)—midline cleavage is absent only in the posterior frontal and parietal areas, and variable portions of the corpus callosum are present.6 *There is some debate as to whether this is a form of HPE because those affected with MIH tend to have a better prognosis and intact olfaction.7 Fig. 72.4 MRI of a fetus with alobar holoprosencephaly in utero. Note the lack of hemispheric division (blue arrows).
Other Craniofacial and Spinal Malformations
72.1 Arachnoid Cyst (Intracranial)
72.2 Neurenteric Cyst (Intraspinal)
72.3 Neuronal Migration Disorders
 Subependymal (periventricular)
Subependymal (periventricular)
 Subcortical
Subcortical
 Marginal glioneuronal
Marginal glioneuronal
 Posterior region of brain more affected
Posterior region of brain more affected
 Anterior region of brain more affected
Anterior region of brain more affected
72.4 Holoprosencephaly (HPE)
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree