, Wolfgang Pirsig2 and Joachim T. Maurer3
(1)
Department of Otorhinolaryngology Head and Neck Surgery, Asklepios Clinic Harburg, Eissendorfer Pferdeweg 52, 21075 Hamburg, Germany
(2)
Department of Otorhinolaryngology Head and Neck Surgery, Mozartstrasse 22/1, 89075 Ulm, Germany
(3)
Department of Otorhinolaryngology Head and Neck Surgery, Sleep Disorders Center University Hospital Mannheim, 68135 Mannheim, Germany
Abstract
(Adeno)tonsillar hypertrophy occurs much more frequently in children than it does in adults. Therefore, this issue is discussed separately. Concerning simple snoring, only a few studies investigate the influence of adenotonsillectomy (ATE) on breathing sounds. Data originate in part from controlled studies; these studies document an efficiency of ATE for simple snoring. (Adeno)tonsillar hypertrophy is the most common etiology for pediatric obstructive sleep apnea (OSA). Accordingly, (adeno)tonsillectomy is often performed as first-line treatment of OSA in children. Cure rates are high. With tonsillotomy (TT) and interstitial radiofrequency treatment (RFT), less invasive surgical alternatives for ATE are available (see Sects. 6.1.2 and 6.1.3). Substantial tonsillar hypertrophy is a rare condition in adulthood. Data for simple snoring do not exist. In contrast, a strong correlation between tonsillar hypertrophy and severity of OSA has recently been described.
6.1 Tonsils
Thomas Verse
Core Features
(Adeno)tonsillar hypertrophy occurs much more frequently in children than it does in adults. Therefore, this issue is discussed separately.
Concerning simple snoring, only a few studies investigate the influence of adenotonsillectomy (ATE) on breathing sounds. Data originate in part from controlled studies; these studies document an efficiency of ATE for simple snoring.
(Adeno)tonsillar hypertrophy is the most common etiology for pediatric obstructive sleep apnea (OSA). Accordingly, (adeno)tonsillectomy is often performed as first-line treatment of OSA in children. Cure rates are high.
With tonsillotomy (TT) and interstitial radiofrequency treatment (RFT), less invasive surgical alternatives for ATE are available (see Sects. 6.1.2 and 6.1.3).
Substantial tonsillar hypertrophy is a rare condition in adulthood. Data for simple snoring do not exist. In contrast, a strong correlation between tonsillar hypertrophy and severity of OSA has recently been described.
6.1.1 Tonsillectomy and Adenotonsillectomy
It seems certain that one of the main reasons for obstructive sleep apnea (OSA) in children is obstructive tonsillar hypertrophy [382, 765, 837]. It has been demonstrated previously that adenotonsillectomy (ATE) during childhood cures OSA with high efficiency. In adults, a strong correlation between tonsillar hypertrophy and the severity of OSA has been demonstrated as well [220, 846, 847]. However, it is not as clear to what extent tonsillectomy (TE) is effective in these latter cases. For this reason, the issue will be discussed separately for children and adults.
Furthermore, surgical techniques such as tonsillotomy (TT) [309], intracapsillary TE, and different interstitial thermal ablation techniques [495] have recently been (re)introduced into the field of sleep surgery. These new developments give this issue new topicality. As interstitial radiofrequency surgery is a completely different operative technique, it will be discussed separately in Sect. 6.1.3.
6.1.1.1 Children
Effectiveness of Treatment
Effectiveness for Simple Snoring
Surprisingly, there are only a few studies focusing on the efficacy of tonsilar surgery for simple snoring. This might be due to the reason that sleep studies are much more difficult to perform in children than in adults. Many studies do not precisely differentiate between simple snoring and OSA. Another problem consists in the lack of established and validated objective measurement techniques to analyze snoring sounds. Table 6.1.1 summarizes the data and quality of studies focusing on (adeno)tonsillectomy for simple snoring (Table 6.1.1).
Table 6.1.1
Efficiency of pediatric tonsillar surgery for simple snoring
Author | N | Follow-up [495] | Surgery | Method | No more snoring | EBM |
|---|---|---|---|---|---|---|
Ahlquist et al. [4] | 85 | 1-12 | TE | Q | 90.5% | 4 |
Swift [732] | 20 | 1 | ATE | Q | 95% | 4 |
Agren et al. [3] | 20 | 12 | ATE | Q | 95% | 4 |
Hultcrantz et al. [309] | 20 | 12 | TT (N = 21) vs. TE (N = 20) | Interview | All: 95.1% 90.5% vs. 100% | 2b |
Helling et al. [274] | 99 | 2-24 | Laser-TT | Q | 88% | 4 |
Coticchia et al. [125] | 10 | 1 | ATE (N = 10) vs. AT + RFT tonsils (N = 13) | VAS 0 -10 | VAS pre: 7.4 VAS post: 1.0 | 2b |
All | 254 | 1-24 | 91.0 | B |
What to be mentioned especially is the work by Hultcranz and colleagues [309] who, in a randomized study, investigated the efficacy of TT compared to TE. In both study arms, snoring had not reappeared in the majority of children postoperatively after a year. Only two of the children continued snoring after the TT, both 6 and 12 months postoperatively. This would seem to point to an advantage of the conventional TE compared to TT. But the difference was not statistically significant. Yet the postoperative morbidity rate in children who underwent TT was significantly lower in comparison with those who received conventional surgery.
Coticchia et al. [125] compared TE with interstitial radiofrequency treatment (RFT) of the tonsils, both groups combined with adenoidectomy (AT). Results in regard to snoring were similar, but the TE group suffered from significantly more postoperative pain and body weight loss
In a third controlled study, Stradling et al. [711] examined 61 children before and 6 months after ATE, as well as 31 healthy, age-matched children at the beginning of the study and 6 months later. In the group of the children having received surgery, the oxygen saturation and the movement time during sleep, as well as various subjective parameters, were normalized to the level of the untreated, healthy children. An improvement of intellectual performance and – in the case of a preexisting developmental deficiency – an acceleration of the maturing process were also found [107, 247].
Interesting in this context is the finding of Tzifa and colleagues [753] that TE during childhood does not reduce the likelihood of becoming an adult snorer.
Effectiveness for OSA
The number of childhood adenotonsillectomies performed in Europe and the United States has declined over the last two decades. At the same time, the indications for ATE have undergone a transition: while fewer operations have been performed for recurrent inflammation, there has been a percentual increase in ATE performed for relief of obstructive symptoms [627, 628]. The spontaneous resolution of OSA secondary to adenotonsillar hypertrophy without surgery has been reported at only 9% [4] within a 1-year observation period [4].
Therefore, ATE is the most common major surgical procedure performed on children [364, 544]. The number of papers providing data of sleep studies as well pre as postoperatively are to many to abstract them well arranged in a table. Various recent reviews underline the importance of ATE as first-line treatment for pediatric OSA [67, 391, 470, 668]. In the first edition of this book we calculated the mean surgical success rate in otherwise healthy children with pediatric OSA as 85.8%.
In 2003, in the form of a Cochrane evidence-based medicine (EBM) review [415], Lim and McKean reviewed 196 references concerning ATE for OSA in children. They did not find one single randomized trial, which means that they could not verify any results. Today there is more information; Table 6.1.2 summarizes all controlled studies available (deadline 1.1.08).
Table 6.1.2
Controlled trials investigating the effect of ATE on the severity of obstructive sleep apnea (OSA) in children
Author | N | Follow-up [415] | Age (years) | surgery | AHI pre | AHI post | Success (AHI< 5) | EBM grade | Control group |
|---|---|---|---|---|---|---|---|---|---|
Stradling et al. [711] | 61 | 6 | 2-14 | ATE | 3.6 | 1.5 | No data | 3b | N = 31 no treatment |
Ali et al. [8] | 12 | 3-6 | 6-12 | ATE | 3.0 | 1.4 | No data | 3b | N = 11 no treatment |
Nieminen et al. [507] | 27 | 6 | 2-10 | ATE | 6.9 | 0.3 | 77.8 | 3b | N = 30 no treatment |
Montgomery-Downs et al. [477] | 19 | 4 | 4.4 | ATE | 10.1 | 1 | 100 | 2b | N = 19 no treatment |
Chervin et al. [107] | 78 | 12 | 5-13 | ATE | 7.3 | 1.1 | No data | 3b | N = 27 no treatment |
Coticchia et al. [125] | 10 | 3 | 2.6-12.5 | ATE | 7.7 | 0.3 | No data | 2b | N = 13 RFT tonsils+ AT |
Tauman et al. [735] | 110 | 1-15 | 1-16 | ATE | 22 | 6 | 71 | 3b | N = 20 no treatment |
Mitchell and Kelly [472] | 39 | 5.1 | 3.1-15.6 | ATE | 17.1 | 2.4 | 72.0 | 3b | N = 33 obese ATE |
All | 356 | 1-15 | 1-15.6 | ATE | 12.3 | 2.7 | 75.0 | B |
All in all, we found raw data of 356 otherwise healthy children who underwent ATE as an isolated procedure for OSA. All selected studies showed significant improvements in respiratory parameters postoperatively. In mean the apnea hypopnea index (AHI) fell from 12.3 to 2.7 after surgery. Apart from the data assembled in Table 6.1.2, it has been shown that craniofacial deformities are common in children with adenotonsillar hypertrophy, and improve significantly with surgical treatment of the airway obstruction [3]. Görür et al. [239] illustrated that adenotonsillary disease with OSA symptoms leads to right and/or left ventricular enlargement and hypertrophy which resolved after ATE. In addition, ATE was shown to have a long-term effect on quality of life in pediatric patients with sleep disordered breathing (SDB) (review worth reading: [229, 473]).
Guilleminault et al. [249] compared different pediatric surgeries for OSA in a retrospective investigation of 400 consecutively seen children. ATE turned out to provide the best results.
However, in those studies in Table 6.1.2 that provide corresponding figures, the success rate of isolated ATE is “only” 75%. Risk factors for persisting OSA are high baseline AHI [669, 735], overweight [471, 669, 735], and other morbidities like Prader Willi syndrome [549].
In some children, obstructive symptoms reoccur years later. Postoperative increase of body mass index (BMI) and overweight were recently identified as risk factors for recurrent disease [21]. In this context, Guimaraes et al. [254] described increased lingual tonsils after prior TE. In a follow-up study performed after an average 7.5 years, Guilleminault found radiocephalometric evidence of anatomic anomalies, particularly behind the tongue (PAS) and in the mandible, as an explanation for recurrence of OSA [247]. Another reason contributing to the recurrence of OSA may be AT in conjunction with unilateral TE. In these cases, the remaining tonsil may undergo hyperplasia, as adenoids may regrow [671]. Guilleminault [251] reported recurrent OSA during the pubertal growth spurt in adolescents who as children had undergone ATE for relief of adenotonsillar hyperplasia and OSA and who had been free of obstructive symptoms over several years.
These findings show that children treated successfully with ATE for OSA should continue to be monitored, particularly those in families with a history of bite abnormalities, which reach their full manifestation during puberty.
6.1.1.2 Postoperative Care and Complications
In general, TE seems to be a procedure with low morbidity in the otherwise healthy child [810]. However, there are some reports suggesting that there may be an increased perioperative morbidity in some children with OSA after ATE [392, 455, 628, 640]. Risk factors are obesity, age below 3 years, Down’s syndrome, congenital heart defect, asthma bronchiale, craniofacial anomalies, and cerebral deficiencies [669, 691, 701, 715, 733]. These children require intense postoperative monitoring for at least 24 h [392, 455, 626]. In some of these cases, a postoperative bilevel positive airway pressure ventilation within the immediate postoperative period has been shown to avoid the risk of reintubation and mechanical ventilation [220].
As minor complications, laryngospasm, nasopharyngeal hemorrhage, and transient airway obstruction have been described after ATE for OSA in children [631].
Indications and Contraindications
After several studies have demonstrated that children who suffer from snoring perform weaker in school than their nonsnoring peers [57, 240, 470, 758], and that these deficits can be eliminated with an ATE [108, 209, 210, 471, 477], a reevaluation process has begun in relation to when an ATE is indicated. Today, we receive far more referrals for an ATE than several years ago.
Based on the available data, we continue to regard ATE principally indicated for children with primary snoring.
In the treatment of pediatric OSA, TE, often in combination with adenotomy, belongs to the most successful surgical procedures, despite a lack of sufficiently large randomized studies. The cure rate of ATE as an isolated procedure in normal weight children lies at approximately 85-95%. We consider surgical indication given in the case of verified OSA even if no clinical evidence of hypertrophy of tonsils and/or adenoids impresses, since the clinical findings correlate only weakly with the extent of the functional obstruction [4, 72, 387]. Children with OSA suffering from trisomy 21 [436] or sickle-cell anemia [639] also profit from an ATE.
In a retrospective analysis of 400 cases of pediatric OSA persistent SDB was found in 14.5% after various treatment modalities [249]. Adenotonsillectomy was performed in only 68% of the cases, but showed the best results. Nevertheless, after ATE, there also remained some nonresponders. In a second prospective survey, the same working group [250] proved that multidisciplinary evaluations of the anatomic abnormalities (i.e., mandibular deficiencies, etc.) before surgery lead to better overall treatment results.
6.1.1.3 Adults
Effectiveness for Simple Snoring
Still no sufficient data exist in the literature documenting any positive effect of isolated TE on simple snoring in adults. Fairbanks reported one single case of complete resolution of snoring in an adult patient [188]. On the other hand, Tzifa et al. [754] considered whether TE could affect snoring, no matter what age and the indication of surgery are. One thousand people took part in their study and filled out questionnaires. The prevalence of snoring was 12.5-48% depending on age, mainly in men. In 19.8% of the cases, TE had already been performed, usually in childhood. TE did not at all reduce the likelihood of becoming an adult snorer.
Effectiveness for OSA
Since substantial hypertrophy of the palatine tonsils is rare in adults, there are only a few studies available (Table 6.1.3).
Table 6.1.3
Effect of TE on the severity of OSA in adults
Author | N | Follow-up (months) | AHI pre | AHI post | Success (%) | EBM grade |
|---|---|---|---|---|---|---|
Orr and Martin [526] | 3 | 1-30 | 55.5a | 9.8a | 100 | 4 |
Rubin et al. [629] | 5 | 2-6 | 50.9a | 26.6a | 40 | 4 |
Aubert-Tulkens et al. [28] | 2 | 1-15 | 31.1a | 18.9a | 50 | 4 |
Moser et al. [486] | 4 | 2-43 | 20.1a | 7.5a | 75 | 4 |
Houghton et al. [297] | 5 | 1-3 | 54.6 | 3.6 | 100 | 4 |
Miyazaki et al. [474] | 10 | No data | 14.0 | 3.0 | 4 | |
Verse et al. [769] | 9 | 3-14 | 46.6 | 10.1 | 88.9 | 4 |
Martinho et al. [440] | 7 | 3 | 81.0 | 23.0 | 85.7 | 4 |
Nakata et al. [491] | 30 | 6 | 69.0 | 30.0 | No data | 4 |
Nakata et al. [489] | 20 | 6 | 55.7 | 21.2 | 4 | |
All | 95 | 1-43 | 49.5 | 7.8 | 80.0 | C |
All of the studies listed in Table 6.1.3 are case series and furnish raw data. All in all, there are 95 complete sets of data of sleep apnea patients who exclusively underwent TE. Counting all ten studies together, the average number of breathing events per hour of sleep sank from preoperative 49.5 to postoperative 7.8. This difference is statistically highly significant (p < 0.0001). In accordance with the success criteria of Sher [665], this amounts to a healing rate of 80.0% in this selected patient pool.
Although the EBM grade of recommendation is low, it can be inferred from these data that a massive tonsillar hyperplasia is rarely seen in adults, but if it exists, TE for the treatment of OSA is almost as successful as in childhood.
6.1.1.4 Postoperative Care and Complications
TE is a standard procedure. The complications and the specific aftercare are sufficiently described in otolaryngological surgery handbooks. Specific aspects in the peri and postoperative management of patients with SDB will be discussed in Sect. 13.
Anyway one problem is worth mentioning. TE patients suffer from substantial pain within the first 10 days after surgery. Therefore, a sufficient pain treatment is mandatory. In this context, Thorneman and Kervall [744] showed significant advantages of a basic oral pain treatment with paracetamol (750 mg × 6) and diclofenac (50 mg × 3) compared to a regimen in which patients received analgetics only on demand. On the other side, a potentially increased risk of postoperative hemorrhage after TE is discussed with the use of nonsteroidal anti-inflammatory drugs (NSAID). Recently, Krishna et al. [373] published a meta-analysis concerning this topic. Data of seven prospective, controlled trials including 1,368 patients were analyzed. Apart from aspirin there appeared no significant increased risk of postoperative bleeding for nonaspirin NSAIDs in this meta-analysis.
6.1.1.5 Indications and Contraindications
As already mentioned, unfortunately no evidence exists in the literature for the efficiency of TE in the treatment of primary snoring. Nevertheless, every otolaryngological surgeon is familiar with individual cases, in which a socially disruptive snoring has disappeared after solitary TE. In contrast to this stands a significant postoperative morbidity. Our own analyses have shown that on average our patients need analgetics for 12 days after a conventional TE. The literature reports a risk of postoperative bleeding of up to 6.1% [819]. We have become extremely cautious with the indication of conventional TE in the case of primary snoring as radiofrequency surgery and TT procedures with a lower morbidity rate are available today.
In adulthood, a massive tonsillar hyperplasia is rare. If it does occur, a TE (without any additional procedures) will be helpful in any case. From the presented data, we have come to the conclusion that we always recommend a TE in the case of a medium-to-severe form of OSA. Also, in the case of mild OSA, we see an indication for a tonsillar procedure if one site of obstruction on the level of the oropharynx is suspected.
Take Home Pearls
ATE is a highly effective treatment for pediatric snoring and OSA, justifying its use as first-line treatment.
Main risk factors for persistent or recurrent disease are substantial overweight, Down’s syndrome, craniofacial deformities, and age below 3 years. This patient population requires intense follow-up care and postoperative monitoring.
In adults with OSA, TE is always indicated if the site of obstruction is suspected to be at the level of the soft palate.
In adults suffering from simple snoring, less invasive surgical procedures are recommended in order to minimize postoperative morbidity and complication rates.
6.1.2 Tonsillotomy
Thomas Verse
Core Features
With tonsillotomy (TT), a less invasive surgical alternative to ATE is available. Terms such as partial tonsillectomy, intracapsular tonsillectomy, or subtotal tonsillectomy describe individual techniques of tonsillotomy.
The technique employed (laser, radiofrequency, bipolar scissors, cold steel, or others) does not seem to be relevant with regard to effectiveness and postoperative morbidity.
In comparison with conventional (adeno)tonsillectomy (ATE), (adeno)tonsillotomy (ATT) causes less pain, less postoperative weight loss, and less disturbance to quality of life.
Preliminary results assume comparable effectiveness for both ATE and ATT with regard to sleep-disordered breathing.
The most important and frequent contraindication for ATT is chronic tonsillitis. As this condition rarely occurs in young children, TT is of particular interest in pediatric SDB.
Within the last 10-15 years, a significant amount of research in tonsil surgery has focused on postoperative pain and recovery times [362]. Of growing interest are the recent reports about tonsillotomy (TT), specifically for those patients suffering from SDB due to adenotonsillar hypertrophy. There is no standard technique for TT so far. Various surgeons recently described their individual surgical technique. All of these techniques require significantly less pain medication and allow the patient to return far more quickly to normal oral feeding as compared with conventional tonsillectomy. Within the following chapter, we abstract the available data using the umbrella term TT.
6.1.2.1 Surgical Technique
The basic principle of all these techniques consists in saving the pseudocapsula of the tonsils by performing the resection strictly within the tonsillar tissue. As a consequence, more or less tonsillar tissue remains in the patient. Technical aids such as bipolar electrosurgical scissors [786], radiofrequency ablation [96, 174, 176, 306], argon-plasma supported monopolar surgery [302], various lasers [138, 149, 274, 308, 315, 322, 756], and the microdebrider [120, 150, 363, 418, 692, 694, 696] have been recommended so far.
Sobol and colleagues [692] compared microdebrider-assisted TT with monopolar electrocautery tonsillectomy. The former turned out to take over 4 min longer (16.9 vs. 20.9 min).
6.1.2.2 Effectiveness for Simple Snoring
Ericsson et al. [174] restudied 92 children 1 and 3 years after radiofrequency-assisted TT (N = 49) and conventional tonsillectomy (N = 43). The authors describe comparable effects for both techniques with regard to snoring, quality of life, infections, and long-term changes in behavior. After 3 years, two children of the TT group were tonsillectomized, one because of peritonsillitis and the other of increased snoring.
Hultcrantz et al. [307] conducted the first controlled study comparing laser-assisted TT (N = 21) with conventional tonsillectomy (N = 20) in 41 children with SDB focusing on postoperative pain and effectiveness. Results in respect of snoring and breathing obstruction were almost the same in both groups after a 1-year follow-up. The same patients were reevaluated after 6 years [308]. The number of children who remained free from snoring decreased from 40 after the first year to 25 after 6 years (11 TT vs. 14 TE). The authors conclude that both surgical techniques show comparable results with regard to snoring both in the short and the long term. In a similar controlled study [149], comparable results concerning snoring were achieved 3 months and 2 years after laser-assisted TT and conventional tonsillectomy. Another noncontrolled series of 36 children [315] described a successful release of snoring after laser-assisted TT in 91% of the cases. Follow-up time varied between 4 weeks and 4 years.
Koltai and colleagues [363] conducted a retrospective case series including 107 children after tonsillectomy and 243 children after microdebrider-assisted TT. Both operations turned out to be equally effective in relieving SDB.
6.1.2.3 Effectiveness for OSA
Today there is some evidence that TT increases quality of life in children and in teenagers with OSA both in the short and the long term. Smith et al. [689] used the OSA-18 questionnaire [693] and the Brouilette Score [76] to measure quality of life in 30 age-matched controls and 92 children with OSA before and after adenotonsillectomy (ATE; N = 30), isolated adenoidectomy (AT; N = 30), and adenotonsillotomy (ATT; N = 32) (EBM 3b). Quality of life parameters improved postoperatively in all three patient groups after surgery. ATE and ATT improved quality of life parameters similarly, resulting in a quality of life comparable with the healthy control group. AT, however, was less effective than ATE and ATT in this trial. Ericsson and co-workers confirmed comparable large improvements in quality of life in adolescents and young adults (age 16-25 years) after both tonsillectomy and TT in the short-term as well as in the long-term follow-up [175, 176]. The most recent study used the OSA-18 questionnaire 3 months and 1 year after microdebrider-assisted TT in 50 children [120]. The total and individual domain scores were significantly improved at both postoperative intervals.
Vlastos et al. [786] conducted a 2-year prospective study including 243 children after TT and 780 children after tonsillectomy (EBM 3b). Data on weight, patient satisfaction, and recurrence of obstructive symptoms were studied in each of 60 randomly selected subjects. Short-term satisfaction was comparable in both groups. Interestingly, in the long term the authors found that twice as many children in the TT group developed obstructive symptoms again, resulting in 3.5% of the patients who were offered a tonsillectomy. In this context a regrowth of tonsillar tissue after partial tonsillectomy (tonsillotomy) was recently estimated at 3.2-17% [96, 696, 756] in groups of 42-278 children (all studies EBM 4).
The only study so far [140] to provide polysomnographic data includes 29 normal weight children with OSA (age: 2-9 years). Exclusion criteria were obesity, craniofacial abnormalities, or other pulmonary, cardiac or metabolic diseases as well as a positive history for recurrent tonsillitis. All children underwent a laser-assisted tonsillotomy with adenoidectomy (ATT). The mean AHI decreased from 14.9 ± 8.7 (± standard deviation) before surgery to 1.1 ± 1.6 twelve months after surgery. All children fulfilled the criteria of surgical success (AHI <5).
6.1.2.4 Postoperative Care and Complications
In a retrospective analysis the overall major complication rate after TT in 870 children was calculated as 0.009%, whereas the overall major complication rate (0.9%) was much higher in 1,121 children after conventional tonsillectomy [694].
The techniques employed (various lasers, coblation, radiofrequency, cold steel, or others) seem to be secondary factors in relation to the observed lowered postoperative morbidity. It seems assured that TT causes much less pain and weight loss as compared with conventional tonsillectomy in the postoperative period [139, 149, 150, 176, 306, 307, 363, 692, 786]. In this context Lister et al. [418] conducted a prospective, randomized, double-blind, matched pair, clinical trial. In 25 children the authors performed a TT on one side and a conventional tonsillectomy on the other side. There was a 100% correlation between the side of otalgia and the side of conventional tonsillectomy.
Ericsson et al. [177] examined presurgical child behavior ratings and pain management after conventional tonsillectomy and laser-assisted TT. SDB influenced children’s behavior, but there was no relation to postoperative pain. The surgical method used predicted pain better than the child’s behavior rating did. Interestingly, the nurses underestimated the pain experienced by the child. In this context, the reduction of postoperative morbidity and pain after TT is very important.
It remains to be seen in how far TT also reduces the risk of postoperative hemorrhage. The current trend points in this direction [149, 302, 315, 786].
Helling et al. [274] did not observe severe complications such as scarred tonsillar crypts and tonsillar abscesses in a survey compassing 826 children after laser-assisted TT with a follow-up of up to 11 years.
6.1.2.5 Indications and Contraindications
Yet at present TT is only indicated in the case of noninflammatory tonsillar hypertrophy. Chronic tonsillitis is still considered to be a contraindication [140, 242, 274, 696]. Randomized studies show comparable results with regard to quality of life for both TT and conventional tonsillectomy. The only trial providing polysomnographic data [140] as well points to a comparable success rate of TT measured against conventional tonsillectomy for pediatric OSA.
Apart from those for adolescents and very young adults (age <25 years), no studies exist investigating the effectiveness of TT in adults. Because of this fact TT does not play a significant role in the treatment of adult SDB.
Owing to the advantages mentioned above the author strongly prefers TT over conventional tonsillectomy in pediatric SDB. This applies to both diagnoses: simple snoring and OSA.
Take Home Pearls
Tonsillotomy (TT) shows a similar effectiveness with regard to pediatric SDB as compared with conventional tonsillectomy.
The intra- and postoperative morbidity after TT is much less than after conventional tonsillectomy, especially in children.
Unless the patient’s history is unsuggestive for chronic tonsillar inflammation, the author always performs a TT for pediatric SDB.
Data on the use of TT in adults are rare.
In adults we prefer conventional tonsillectomy due to the higher incidence of chronic tonsillitis and other affections of the tonsils.
6.1.3 Interstitial Radiofrequency Treatment (RFT)
Boris A. Stuck and Thomas Verse
Core Features
Interstitial radiofrequency treatment (RFT) uses high-frequency alternating current to induce thermal lesions and tissue necroses. Bipolar and monopolar systems exist.
In sleep surgery, RFT is used within the nasal turbinates, the soft palate, the base of tongue, and the tonsils. Submucosal scarring results in a stiffening of the soft palate and tongue base. Within lymphatic tissue (tonsils) and within the nasal conchae, RFT achieves an additional reduction in tissue volume.
RFT of the tonsils can easily be performed under local anesthesia. Sedation and a perioperative antibiotic prophylaxis are recommended.
RFT of the tonsils achieves a 40-75% reduction of tonsillar volume. Preliminary results are comparable to tonsillectomy in regard to reduction in AHI and subjective snoring.
Within the first days after surgery, a swelling of the tonsils occurs. Pain killers are needed for 1-2 days. Complications are minimal.
RFT of the tonsils meet our criteria of minimally invasive surgery.
Radiofrequency techniques use high-frequency alternating current to either cut or coagulate tissue. If used as an interstitial treatment, a needle electrode is inserted submucosally into the soft tissue. By applying radiofrequency energy, a thermal lesion is created followed by scar formation. Depending on the tissue that has been treated, this results in either stiffening or shrinking. To differentiate this kind of surgery from cutting radiofrequency procedures, we will use the term interstitial radiofrequency in the following.
Within the scope of sleep surgery, interstitial radiofrequency treatment (RFT) has been established in the treatment of the inferior turbinates [406, 759], the soft palate [577], and the base of tongue [575, 576]. Little is known about its use in the treatment of tonsillar hypertrophy.
The analysis of the current literature is complicated because of the lack of standardization in surgical techniques and its nomenclature. In terms of surgical approaches to the palatine tonsils, radiofrequency surgery is frequently used not only for interstitial treatment but also for partial (tonsillotomy) or total tonsillectomy (e.g., coblation). Those techniques will be discussed in the corresponding chapter of this book, while in the following sections, only interstitial thermotherapy with radiofrequency energy will be presented.
6.1.3.1 Principles of Interstitial Radiofrequency Surgery
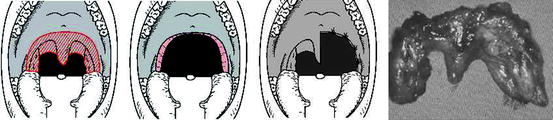
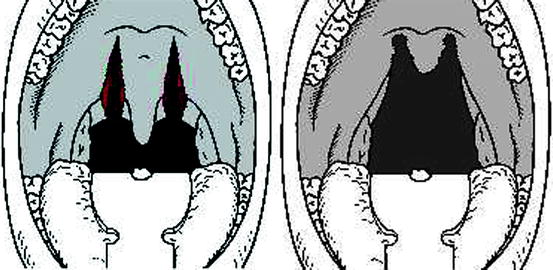
The principle of interstitial radiofrequency surgery lies in the submucousal application of radiofrequency energy (low frequency radio waves) via a mono- or bipolar application needle. This induces thermal lesions and tissue necroses (Fig. 6.1.3.1).


Fig. 6.1.3.1
Interstitial application of radiofrequency energy via a bipolar needle electrode (turkey hen meat). System Celon (RFITTR, Celon, Teltow, Germany)
In vivo, this results in a tissue necrosis and a perifocal edema, which can be nicely imaged in the MRI (Fig. 6.1.3.2).
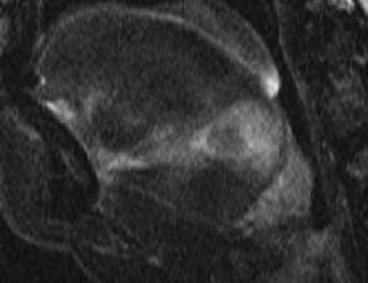
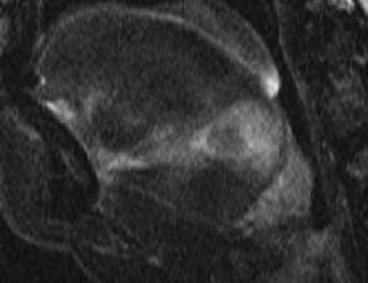
Fig. 6.1.3.2
Radiofrequency lesion and perifocal edema in the MRI (TIRM-sequence)
Currently, a limited number of systems is available using different methods of energy application (mono vs. bipolar). The energy application can furthermore be either controlled or uncontrolled. The controlled procedures include among others somnoplasty (temperature controlled – Somnus, Gyrus ENT, Bartlett, IL), the Celon system (resistance controlled – Celon AG Medical Instruments, Teltow, Germany), and the reusable devices provided by Sutter (resistance controlled – Sutter Medizintechnik, Freiburg, Germany).
The Somnus system is the system that has by far received the most evaluations as it was the first system to be introduced in sleep surgery. Radiofrequency energy is delivered at 465 kHz using a specially constructed needle electrode and monopolar delivery system (Fig. 6.1.3.3). A thermo element is integrated into the tip of the electrode that continuously measures the surrounding tissue temperature. The tissue target temperature is set by the surgeon. While in the case of electrocoagulation, tissue temperatures of above 500°C are reached; with Somnoplasty, it is possible to generate temperatures significantly below 100°C. The lesion size can be regulated via power setting and energy input.
Fig. 6.1.3.3
Mono (i.e., Somnus) and bipolar (i.e., Celon, Sutter) systems for interstitial radiofrequency surgery
The Celon system regulates the energy input by means of the tissue resistance. It consists of a bipolar system (Fig. 6.1.3.3) with both electrodes in the needle tip, separated by an isolating element (Fig. 6.1.3.1). A neutral electrode is not necessary. With the help of the applied radiofrequency energy (300 kHz to 2 MHz), the water is thrust out of the tissue. As a result, the tissue resistance increases. If the system is used on a high power level, resistance increase rapidly, resulting in a smaller lesion. This means that for larger lesion, e.g. at the tongue base or the tonsils, lower power levels need to be set compared to the nasal concha or the soft palate, where smaller lesions are needed. A comparable method of energy control is used by the reusable bipolar probes of the Sutter system, using two separate probes in one needle.
Furthermore, a multitude of uncontrolled systems are available for interstitial radiofrequency surgery wherein the energy is applied under manual control only. This means that for these systems a certain measure of surgical experience is needed in order to determine the ideal energy input. Popular instances of this type of systems are for example the Plasma Coblation System (ENTec, Arthrocare, USA) or the Ellman system (Ellman International, Oceanside, CA). Unfortunately, almost no studies exist which evaluate the safety level of these systems.
6.1.3.2 Surgical Technique
In adults, surgery is usually performed under local anesthesia as an outpatient procedure (these systems can also be used to treat hypertrophic tonsils in children). Surgery is performed in a sitting position. In order to treat potential complications, an intravenous line is established. The patient may be sedated according to the patients or the surgeons’ choice. We prefer Midazolam i.v. for sedation under monitoring with pulse oximetry and ECG.
A superficial disinfection may be performed, and then local anesthesia is executed. We use Prilocaine 2% with suprarenine (1:200,000). According to size, each tonsil is infiltrated with approximately 5 mL local anesthetic. In our opinion, due to the frequent hypersalivation, the use of a surface anesthetic delivered as a spray has not proven to be advantageous.
The technique is similar to that used at other sites. A needle electrode is inserted into the lymphatic tissue of the tonsil. Depending on the size of the tonsil and the technical device used, four to eight lesions are created per side (Fig. 6.1.3.4).
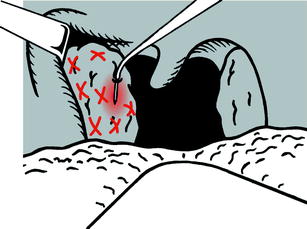
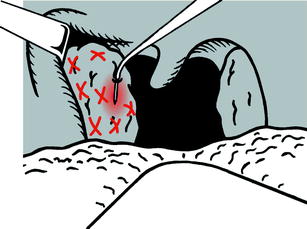
Fig. 6.1.3.4
Application pattern for RFT of the tonsil
We regularly used the Celon system for tonsil reduction (Celon AG medical instruments) applying 7 W per lesion with a total amount of 4-8 lesions per side.
Regardless of the system used, the amount of swelling in the initial postoperative period exceeds the initial reduction, which means that tonsil size may be equal or larger than the preoperative size. Therefore, we do not recommend using radiofrequency techniques on an outpatient basis in patients with kissing tonsils. Tonsil shrinkage occurs between the first and third week after surgery. A view at 3 weeks postoperatively is shown in Fig. 6.1.3.5.


Fig. 6.1.3.5
RFT of the tonsils. Right tonsil: preoperative situation. Left tonsil: situation 3 weeks after surgery
6.1.3.3 Effectiveness for SDB
The calculated reduction of the tonsil size is specified as ranging from 51.1 [215] to 75.0% [497]. Pfaar et al. measured tonsil size with sonography and found a volume reduction of 40% [560]. Nelson described improvements in daytime sleepiness (79%), subjective snoring (81%), and in the Epworth Sleepiness Scale (70%) 3 months after surgery in 12 patients. These results remained constant after 6 and 12 months in the same population [496]. In children the same author found an improvement in quality of life parameters up to 1 year after surgery.
Concerning the effectiveness of isolated radiofrequency surgery of the tonsils for obstructive sleep apnea (OSA), only a small number of studies are available. Nelson performed an interstitial RFT of the tonsils, combined with an adenoidectomy, in 10 children [497]. The apnea hypopnea index (AHI) decreased not statistically significant from 8.8 to 4.2 one year after surgery. Additionally, he found improvements in daytime sleepiness and in the obstructive sleep apnea-18 questionnaire score. A recent randomized controlled trial compared effectiveness and postoperative morbidity between temperature-controlled radiofrequency surgery and standard tonsillectomy (in both cases including adenoidectomy) in a group of 23 children with OSA [125]. The authors reported comparable results in terms of clinical efficacy. The mean RDI improved from 7.7 to 0.3 in the tonsillectomy group and from 7.6 to 1.6 in the radiofrequency group (total amount of energy: 13,681 J per treatment). Improvement of daytime sleepiness was comparable in both groups. Postoperative morbidity was less in the radiofrequency group, especially with regard to the return to normal diet.
Fischer et al. [201] performed multilevel interstitial radiofrequency therapy of the soft palate, base of tongue, and tonsils in 15 sleep apneics. All patients received 16 treatment sites with a total dose of 9,750 J (somnoplasty). The AHI significantly decreased from 32.6 to 22.0 after surgery. Using Sher’s criteria, 20% were regarded as cured after the procedure. Nevertheless, the specific effect of tonsil reduction in this population can not be established due to the combined approach.
6.1.3.4 Postoperative Care and Complications
To avoid infections, we recommend a perioperative (e.g., cephazolin i.v.) and a postoperative oral antibiotic prophylaxis for 5 days (i.e., penicillin). In some cases, corticosteroids are needed to reduce postoperative swelling; nevertheless, we discourage the regular use of corticosteroids in radiofrequency surgery. There is no specific postoperative care. Patients are recommended to consume ice cream or to suck ice cubes to reduced postoperative swelling. Postoperative morbidity has been estimated by Nelson [495] and by Friedman et al. [215]. The patients reported pain for up to 2 days after surgery. Pain killers were needed for 1-2 days. On average, the patients returned to normal activity within 1-2 days or after 2.4 days respectively. Friedman et al. compared postoperative morbidity of radiofrequency surgery, tonsil coblation, and with standard tonsillectomy in terms of pain days, narcotic-days, and days before return to normal diet and activity and found a substantial reduction in postoperative morbidity in the radiofrequency and coblation group compared to “cold” dissection [215]. In a randomized prospective study of Pfaar et al. [560], postoperative morbidity, blood loss, and procedure time were compared between bipolar interstitial radiofrequency surgery and standard tonsillectomy in a group of 137 patients. The amount of tonsil reduction assessed with sonography was reported as 40%. Postoperative pain, dysphagia, speech problems, and intraoperative blood loss were significantly less in the radiofrequency group compared to the standard tonsillectomy group, and the procedure time was less in the radiofrequency group. Nevertheless, as clinical efficacy was not assessed, the significance of the study is limited.
Interstitial radiofrequency surgery of the tonsils is a safe procedure. Intraoperative blood loss ranges from minimal (<20 mL) to none. Up to now, other working groups and the authors have not seen any postoperative bleedings after radiofrequency of the tonsils [215, 495, 497]. Only Fischer et al. [201] described the formation of a tonsillar abscess. Admittedly, the lymphatic tissue tends to develop postoperative edema and the upper airway may be obstructed immediately after surgery. Therefore, overnight observation is recommended in cases of kissing tonsils and especially in children.
6.1.3.5 Indications and Contraindications
Interstitial radiofrequency surgery of the tonsils is a minimally invasive procedure with low postoperative morbidity resulting in a substantial shrinking of tonsillar tissue. In children, the technique competes with different tonsillotomy techniques. Both techniques, interstitial radiofrequency and tonsillotomy, have to be performed under general anesthesia. Both techniques require overnight observation. Controlled interstitial radiofrequency surgery is still an expensive technique because the majority of applicators are single-use instruments. Therefore, we rarely perform interstitial radiofrequency surgery in children.
In adults, the procedure can easily be performed under local anesthesia on an outpatient basis. According to the underlying anatomy we regularly perform combined procedures on the tonsils, the soft palate and in selected cases the base of tongue in patients with simple snoring and mild OSA.
Exclusion criteria for interstitial radiofrequency procedures are asymmetrical tonsillar hypertrophy with suspected malignancy, a history of peritonsillar abscess, and patients with a clear history of repeated tonsillar infections [215], the latter being a relative contraindication to our understanding. In moderate or severe OSA in adults, interstitial radiofrequency surgery alone is in most cases not sufficient.
Take Home Pearls
Initial postoperative swelling may lead to upper airway compromise. There RFT of the tonsils should not be performed in kissing tonsils on an outpatient basis.
Volume reduction is substantial but less as compared to tonsillectomy and tonsillotomy.
Preliminary results in regard to sleep-disordered breathing are promising.
6.2 Uvulopalatopharyngoplasty (UPPP)
Wolfgang Pirsig and Thomas Verse
Core Features
Since 1963, UPPP has been performed for SDB. Since 1981, it is used to treat OSA.
The human soft palate has many physiological functions, which need to be preserved by a gentle surgical technique, saving the palatal muscles.
UPPP is effective for simple snoring. Long-term results (>3 years) show satisfaction rates of more than 70%. However, short-term success rates are even higher. This means that the effect of UPPP in regard to diminishing socially inacceptable snoring ceases within the first year after surgery.
For OSA, if the tonsils are still present, UPPP always with tonsillectomy is the surgical standard procedure. No other surgical technique has been investigated more intensively so far. As in primary snoring, the effect of UPPP ceases within the first year after surgery. Long-term success rates are about 50%.
UPPP with and without tonsillectomy causes postoperative morbidity. The pain requires analgetic drugs for a mean of 12 days.
Various complications have been described after UPPP. Most of them can be avoided by a careful surgical technique preserving the palatal muscles.
No surgical procedure for the treatment of SDB has received more research attention than uvulopalatopharyngoplasty (UPPP). Since the first UPPP for snorers by Ikematsu in 1963 [314] and the introduction of a more radical procedure for OSA by Fujita et al. [224], several modifications that aim at reducing the excessive tissue components of the soft palate mostly combined with tonsillectomy have been published. These early modifications of UPPP were mostly radical, indicated without patient selection, and did not address the often concomitant tongue base level and the lateral velopharyngeal segment collapse. This resulted in unsatisfying outcomes, several long-term side effects, and often a deterioration of the SDB. Recently, the first study of the long-term quality of life outcomes of a group of 49 unselected patients who underwent UPPP between 1980 and 1983 for OSA at Stanford University has been published [235].The details of the various complications and insufficiencies still present 17-20 years after a radical UPPP are rather shocking and will be discussed later.
In the last two decades of the twentieth century, most UPPP procedures (summary in: [186]) included the resection of too much velar tissue, which is important for functions such as phonation, and nonphonetic functions [199] as swallowing, lubrication, blowing, playing wind instruments, whistling, coughing, gagging, withholding a sneeze, or modifying the resistance of the mouth. To achieve these functions, a complex synergism of the palatal and pharyngeal muscles [300], of muscle spindles in the palatoglossus muscles and tensor palati muscle [375], of an intact sensory innervation of the palatal mucosa, and of small submucosal salivary glands is necessary. The velum with the uvula is especially needed for the transport of the mucus from the nasal septum into the pharynx [312].
In the last 15 years, histological research of the palatal tissues revealed an irreversible polyneuropathy in patients with OSA, and functional studies showed a significant impairment in sensory detection threshold for OSA vs. control subjects in the oropharynx, velopharynx, and at the larynx (summarized in [142, 504]). From these anatomico-pathological and functional data, one can conclude that any type of aggressive surgery to the velum in patients with OSA will enhance the preexisting polyneuropathy.
With this anatomico-pathological and physiological knowledge of the soft palate in mind, a tissue preserving technique of UPPP, partially based on Ikematsu’s procedure [314], is presented here, which we have successfully utilized since 1996 in selected patients with SDB and with a minimum of long-term side effects [75, 569]. This is achieved by protecting the anterior palatine arch and the uvula in its muscle containing part.
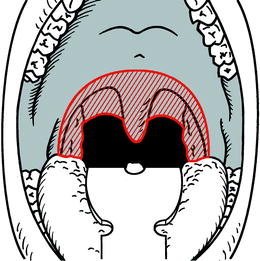
6.2.1 Surgical Technique
UPPP with or without tonsillectomy is performed under general anesthesia with the patient in the Rose’s position (supine with head hanging) and without an infiltration of the soft palate with vasoconstrictive additive and local anesthetic. Partial uvulectomy can be performed at the beginning or at the end of the operation. To do it at the end may mean to shorten a possibly edematous uvula. The uvula tip is grasped and pulled tonguewards. In this way, the muscle bellies can clearly be distinguished, and the excessive mucosa of the uvula tip can be cut off without touching the musculi uvulae. The uvula stump is sewed together with a 3-0 double Vicryl suture (Fig. 6.2.3).
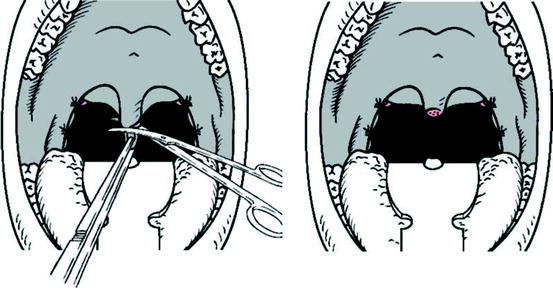
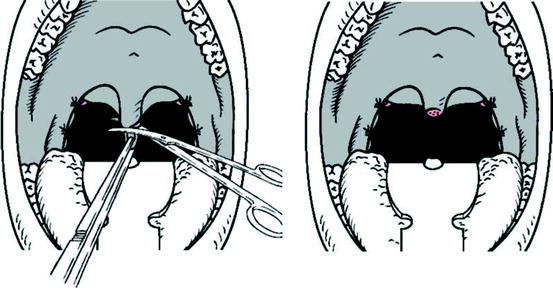
Fig. 6.2.3
Resection of the redundant mucosa of the uvula
The incision into the mucosa of the anterior pillar is performed with a semicircular movement in the oral fold of the palatoglossus muscle, approximately 2 mm away from the free edge, 1 cm to the uvula base. Then the fibers of the M. palatoglossus are dissected from the tonsil. Tonsillectomy follows, in which the posterior tonsilar pillar is initially preserved (Fig. 6.2.1).
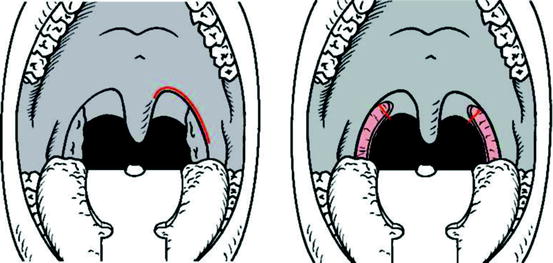
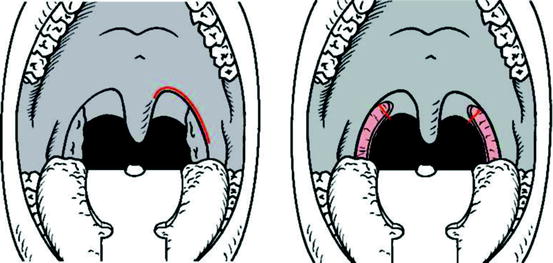
Fig. 6.2.1
Incision along the caudal edge of the left palatoglossus muscle, with scalpel No. 11 (left). Situation after tonsillectomy with preservation of the posterior pillar (right)
The posterior tonsilar pillar is partially incised (Fig. 6.2.2), precisely at the site of maximum tension of the palatopharyngeus muscle as felt by pulling the posterior pillar with a forceps toward the curvature of the anterior pillar. As a result, the posterior pillar opens up in a “V” shape, which produces a lengthened posterior pillar edge to be sewed together with the anterior pillar (Fig. 6.2.2). Now the two pillars can easily be sutured together without tension. This double suture combines mucosa and musculature of the anterior pillar (1), of the lateral pharyngeal wall (2), and of the posterior pillar (3) with braided, absorbable, atraumatic thread (e.g., VicrylR 2-0 SH or 2-0 SH1 or PolysorbR 2-0 X). Usually three sutures per side are sufficient to close the curvature of the joined pillars leaving open the inferior tonsillar fossa. With these sutures, the posterior tonsilar pillar is moved toward lateral and toward oral. This results in a semi-elliptical soft palate (Fig. 6.2.3) with a functioning uvula. Finally, redundant mucosa on both sides of the uvula is removed, and the mucosal wound is sewed (Fig. 6.2.4).
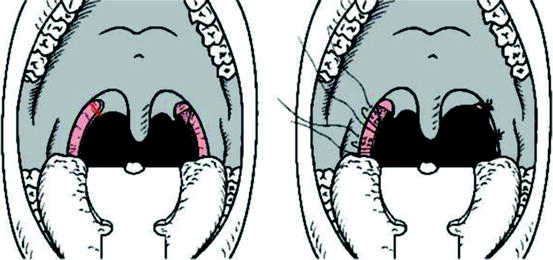
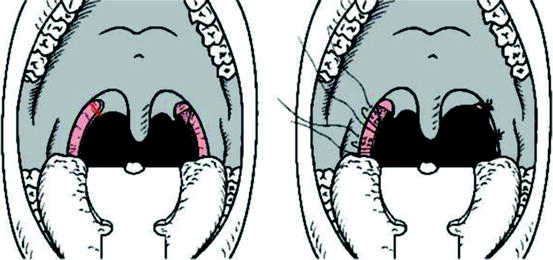
Fig. 6.2.2
Incision of the posterior tonsilar pillar laterally to the uvula (left). Suture of both tonsilar pillars with 2-0 absorbable, atraumatic thread (right)
Conclusion: This procedure of UPPP with tonsillectomy preserves all velar muscles and sacrifices only a minimum of velar mucosa. The careful adaptation of the mucous membrane folds guarantees a controlled healing of the wound. A less vibrating new velum with a shortened functioning uvula has been created with a lateralized superior posterior pillar and the horizontal edge of the velum more in an anterior position. Together with the tonsillectomy an enlargement of the upper airway caliber at the velopharyngeal level has been achieved without adding more damage to the new velum with its preexisting polyneuropathy in patients with OSA. With this alternative procedure of UPPP there is no rationale for radical UPPP [568] (Fig. 6.2.4).
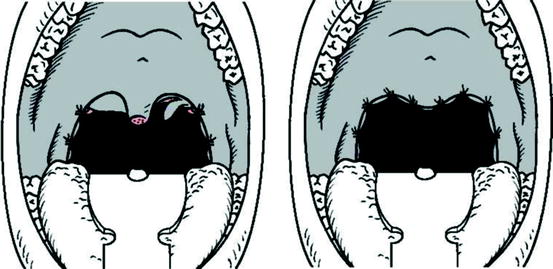
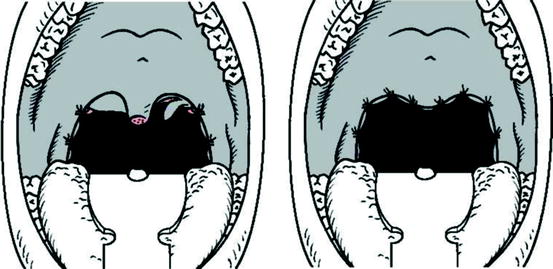
Fig. 6.2.4
Resection of minimal amounts of excessive mucosa on the left posterior pillar (left). Final result after adaptive suture (right)
In the meantime, UPPP plus tonsillectomy according to the above technique has been performed in Ulm, Mannheim, and Hamburg on more than 600 patients suffering from primary snoring and OSA. As the main postoperative complication, bleeding occurred in 0.7% of the patients. Up to now, no long-term velopharyngeal insufficiency or nasopharyngeal stenosis has been observed. For a bit over 10% of the patients a follow-up nCPAP therapy was necessary. In none of the cases was the therapy impaired by an oral air leakage.
When employing more radical techniques (Fig. 6.2.5), as they have still been suggested since the 1980s, permanent velopharyngeal insufficiencies in up to 24% of cases [257], nasopharyngeal stenoses in up to 4% [344], and nCPAP therapy failures as a result of oral leakage [262, 485] have been described. The permanent subjective complaints as sequelae of these radical UPPP techniques even after 17-20 postoperative years are described by Goh et al. [235] and support our opinion that no indication exists for a radical UPPP today.
6.2.2 Effectiveness for Simple Snoring
Numerous studies have been published regarding the efficacy of isolated UPPP for primary snoring. Here also the definitions of what constitutes surgical success differ immensely; in the following, we therefore have to restrict ourselves to the compilation of studies with long-term data. In our understanding, only follow-ups of at least 3 years can be regarded as long-term data. The existent data are summarized in Table 6.2.1.
Table 6.2.1
Long-term results of UPPP for primary snoring
Author | N | Follow-up (years) | No more snoring (%) | Snoring reduced (%) | No change (%) | Snoring worse (%) | EBM |
|---|---|---|---|---|---|---|---|
Macnab et al. [432] | 118 | 3-7 | 55 | 22 | 20 | 3 | 4 |
Levin and Becker [393] | 69 | 1.5-7 | 46 | 11 | 43 | 0 | 4 |
Chabolle et al. 1998 [97] | 39 | 3-7 | 44 | No data | No data | No data | 3b |
Hultcrantz et al. [307] | 30 | 5-7 | 8 | 77 | 15 | 0 | 4 |
Hagert et al. [259] | 254 | 1-8 | 18 | 73 | 9 | 0 | 4 |
Pasche et al. [547] | 100 | 4 | 52 | 26 | 22 | 0 | 4 |
Hicklin et al. [282] | 201 | 2-10 | 19 | 25 | 36 | 19 | 4 |
Hassid at al. [270] | 57 | 5 | 12 | 68.5 | 19.5 | No data | 4 |
All | 868 | 1.5-10 | 29.8 | 43.1 | 29.4 | 8.1 | C |
Two studies [282, 393] also include short-term results from the identical patient pool. Respectively 87% and 76% were classified as responders. This percentage fell in the long-term follow-up to respectively 46% and 45%. Accordingly Hassid et al. [270] recently described decreasing success rate with increasing follow-up periods.
Combining the values for “snoring reduced” and “no snoring” results in a long-term success rate of 73% for isolated UPPP in the treatment of primary snoring, based on the data of all 868 patients included in Table 6.2.1. But this figure has to be considered with caution, due to the fact that the diverse evaluation criteria are extremely heterogeneous. Accordingly, the success rates vary in the cited studies between 44 and 91%.
It was possible to objectively corroborate a reduction of the alpha-EEG arousals after UPPP in the case of nonapneic snoring [62]. Janson and colleagues [327] found reductions in daytime sleepiness and fatigue in 155 nonapneic snorers following UPPP.
6.2.2.1 Comparison of Different Soft Palate Surgical Techniques
Chabolle and colleagues [97] included in the same follow-up study also patients after LAUP. The groups were comparable in regards to age, gender, and BMI. With 44%, the success rate (complete elimination or satisfactory reduction of snoring) was identical in both groups. But the general satisfaction with the surgery was significantly higher in the UPPP group than in the LAUP group. The reasons remained unclear. On average, in the LAUP group 4.2 treatment sessions (UPPP only one) were necessary, and the rate of unwelcome side effects was slightly higher. Nevertheless, the authors conclude that both procedures are suited for the treatment of primary snoring.
An objective analysis of the respiratory sounds during sleep furnished a similar success rate for UPPP and LAUP, both for short-term (2-11 months) and long-term (29-56 months) follow-up assessment [530, 531].
Lysdahl and Haraldson [430] prospectively performed UPPP or LUPP in 121 patients. Both techniques achieved significant improvement of subjective parameters such as snoring, awakenings, apneas, daytime sleepiness, and sleep spells driving at short-term follow-up (3 months). UPPP was superior to LUPP for all clinical effect parameters. Five to eight years after surgery, all subjective parameters except sleep spells while driving worsened with the years, with UPPP again showing better long-term results. Similarly, in the study of Hagert and coworkers [259] the conventional UPPP yielded significantly better results for snoring than LUPP.
6.2.3 Effectiveness for OSA
Only few prospective studies (with the level of evidence 4) exist covering long-term results of up to 9 years after UPPP. As with the other techniques, the comparability of these data is made problematic due to varying success criteria. Almost unanimously, all authors find a discrepancy between adequate subjective improvement of their symptoms and nearly unchanged objective sleep parameters after UPPP. Therefore, a polygraphic or polysomnographic postoperative evaluation is necessary after one to three years.
Every surgeon should study the excellent survey by Sher et al. 1996 [665]. The authors used as success criteria an AHI < 20 and a reduction of the AHI of at least 50% (or analogously: AI < 10 and AI < 50%). For the nonselected patient pool this meta-analysis yielded a surgery success rate of 40.7%. In the selected group with clinically suspected obstruction solely on the level of the soft palate, a success rate of 52.3% was found. For the most part, these data are based on short-term results.
Data concerning long-term success are summarized in Table 6.2.2 (worth reading review in [566]).
Table 6.2.2
Long-term results after UPPP for OSA using Sher’s criteria of success
Author | N short | N long | Follow-up short (months) | Follow-up long (years) | Success short (%) | Success long (%) | Criterion of success | EBM |
|---|---|---|---|---|---|---|---|---|
Larson et al. [385] | 50 | 48 | 6 | 3.8 | 60.0 | 50.0 | Sher | 4 |
Lu et al. [426] | 13 | 13 | 12 | 7.3 | 69.2 | 30.8 | Sher | 4 |
Perello-Scherdel et al. [556] | 57 | 6 | 5 and 10 | No data | 52.6 | AHI <10 | 4 | |
Janson et al. [326] | 25 | 25 | 6 | 4-8 | 64.0 | 48.0 | Sher | 4 |
Hultcrantz et al. [307] | 17 | 13 | 3 | 5-7 | 82.4 | 69.2 | Sher | 4 |
Boot et al. [60] | 38 | 29 | 6 | 1-6.2 | 42.1 | 31.6 | ODI <50% | 4 |
All | 200 | 185 | 3-12 | 3-10 | 60.5 | 47.6 | C |
Table 6.2.2 impressively demonstrates that the effect of UPPP on the severity of OSA decreases over the years. As a consequence of these findings, we and other study groups infer the necessity of a long-term sleep medical control of the patients after UPPP. The employed success criteria are again heterogeneous. If one combines those data from Table 6.2.2, which use Sher’s success criteria [665], this yields a long-term success rate of 49.5% for isolated UPPP including tonsillectomy in the treatment of OSA. Nowadays, one can rightly assume a positive long-term effect of isolated UPPP, possibly in connection with a tonsillectomy.
Recently Maurer [450] published a meta-analysis showing that a simultaneously performed tonsillectomy doubles the success rate of UPPP for OSA. Five studies including 269 patients (N = 155 with vs. N = 114 without tonsillectomy) were cited in this analysis [60, 279, 456, 653, 704]. The surgical success rate was 30% in the patients without tonsillectomy, while it was 59% in the group with concomitant tonsillectomy.
In accordance with these results, in a group of 400 patients with SDB who had received a UPPP or a laser UPP, no increase in mortality was found in comparison to a control group comprising 744 persons [429]. These data may indicate a positive survival effect of UPPP surgery. Keenan et al. [349] contacted their OSA patients treated with either UPPP (N = 149) or nasal CPAP (N = 126) over a 6-year period to compare long-term survival rates between these two treatments. There was no difference between the two treatment groups (Fig. 6.2.6). Furthermore, UPPP for SDB turned out to improve the patients’ stimulated long-term driving performance [265] and decreased the number of car accidents within a 5-year period after surgery [266].
6.2.4 Postoperative Care and Complications
UPPP is one of the most common operations performed for OSA. The anatomic and physiologic abnormalities associated with OSA pose independent risks of complications in the intra- and perioperative periods [135, 438]. Postoperative edema and respiratory depression enhance the risk of reintubation or emergent tracheotomy within the first few hours after surgery [122, 333]. The incidence of lethal complications is given as 0.2-0.03% [90, 356]. Serious cardiorespiratory complications other than death occur in 1.5% of the cases [356].
Intraoperatively, we administer an intravenous single-shot antibiosis with 2 g Cefazolin. Apart from this, antibiotics are only used in the case of relevant inflammatory complications. The severe pain occurring in almost all of the patients in the first postoperative days is treated with diclofenac and metamizol. However, frequently the administration of further, more potent analgesics becomes necessary. At any rate, basic pain treatments with fixed analgetic applications are superior as compared to regimen in which patients received analgetics only on demand [744]. Apart from aspirin there is no significant increased risk of postoperative bleeding for nonaspirin NSAIDs as recently published in a meta-analysis [373].
During the first postoperative day, the patients are fed via infusion, and take in tea and ice-cream as in the case of a tonsillectomy. From the second day on our patients receive a special tonsillectomy diet. The threads are removed between the 10th and 13th postoperative day. The in-patient time varies between 2 and 5 days, depending on the ability to eat and the extent of pain. Usually, a postoperative intensive care supervision is not necessary after isolated UPPP [82, 464]. Performing the above-mentioned technique of muscle-preserving UPPP, we observed nearly always a pronounced edema of the uvula stump which caused more snoring in the first postoperative nights.
Most patients are able to swallow liquids on the first postoperative day, albeit under pain. For approximately a third of the patients, the pain continues to be rather severe until the fifth day (Fig. 6.2.7); for another third, the pain is comparable to regular tonsillectomy, while the last third of patients receiving surgery experiences virtually no pain on the fifth day. In the context of follow-ups 6 months after UPPP, so far no patient has complained about pain during food intake.
Fig. 6.2.7
Pain after UPPP, UPPP+TE, and LAUP. x-axis: days postoperative. y-axis: pain sensation on a visual analog scale (VAS) with the endpoints 0 = no pain, and 10 = unbearable pain
On the whole, postoperative pain after UPPP and LAUP is comparable in respect to duration, intensity, and consumption of pain killers [747, 809]. Much less painful is radiofrequency surgery on the soft palate [623, 718, 748].
Obviously, the new movement pattern of the operated velum during swallowing needs to be trained from scratch. Strongly carbonated beverages may cause gas bubbles to rise into the nasopharynx. Using a technique that removes the oral mucosa of the whole uvula and sews the tip of the uvula muscle into the median soft palate [565] in the long-term, in the case of our own patients after over 4 years, 40% of the patients complained of an increased viscous mucous production in the pharynx because of the loss of the “drip-stone uvula” for transporting nasal secretions. Our more recent technique, described in Fig. 6.2.4, does not lead to an increased mucous production in the pharynx. Clinically, a dry pharynx is often found. Some patients also experience mildly distorted sensations in the area of the soft palate, but no pain.
As with any tonsillectomy, postoperative bleeding during the healing phase is a possibility; though as a result of a careful velum suture, this has become (0.7%) a rare occurrence in our own patient pool. Despite double suture, on the fourth to fifth day the suture often breaks in the descending suture area; yet it remains intact in the horizontal part, which is crucial for the stabilizing scarring. In previous years, we often administered antibiotics (e.g., amoxicillin) over a period of 5-7 days; we repeatedly observed a stomatitis aphthosa in these cases. This has become a very rare occurrence since we have begun applying the antibiotic only perioperatively. Also, the fetid mouth odor setting in with the third postoperative day, which is so typical for tonsillectomy without mucous membrane, is usually absent in our patients.
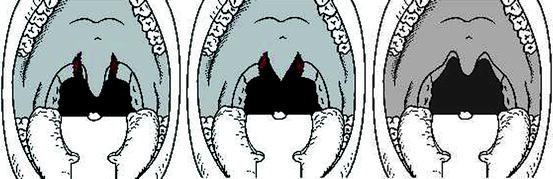
The dreaded velar insufficiency with rhinolalia aperta and/or entrance of food into the nose during swallowing (Fig. 6.2.8) have only been observed when the musculature of the anterior palatine arch is partially resected, which we could see in patients after velar surgery alio loco coming for revision surgery.


Fig. 6.2.8
Velopharyngeal incompetence after aggressive UPPP
Another reason for velopharyngeal insufficiency is a too short and too firm soft palate. Such patients can already be distinguished preoperatively by virtue of the fact that water flows into their nose during the so-called Finkelstein test [199]. Patients are asked to drink water with their heads protruded from under a running faucet. In the case of velum sufficiency no water enters the nose. We use this test pre- and postoperatively in order to document the velar sufficiency of the patient undergoing surgery.
Since OSA cannot be cured by surgery in every case and due to the fact that even after a temporary postoperative normalization SDB can reoccur, soft palate surgery must always be performed in such a way that CPAP therapy remains an option at all times. But if the palate musculature is partially resected during UPPP, then a nasal over pressure respiratory therapy with the help of nasal CPAP can become very difficult, because the air escapes through the mouth. Mortimore et al. [485] discovered that after a UPPP with partial resection of the velum musculature no mask pressure higher than 13 cm water column can be nasally applied through the CPAP mask without creating an air leakage through the mouth. In the case of patients with an intact velum, and also after application of the UPPP technique described here, no air escapes through the mouth, not even in the case of nasal CPAP pressures of 20 cm water column. Han et al. [262] corrobated this observation in a prospective control trial where they found a higher CPAP failure rate because of mouth air leak in the group who underwent a more radical UPPP with removal of all of uvula and part of the soft palate than in the group with a less radical UPPP and the uvula partly preserved.
Equally dreaded is nasopharyngeal stenosis (Fig. 6.2.9). The following are considered as risk factors for the development of a nasopharyngeal stenosis: aggressive surgical technique, extension of surgery to the lateral pharyngeal walls, and postoperative wound infection.
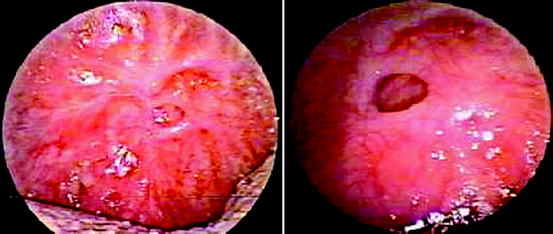
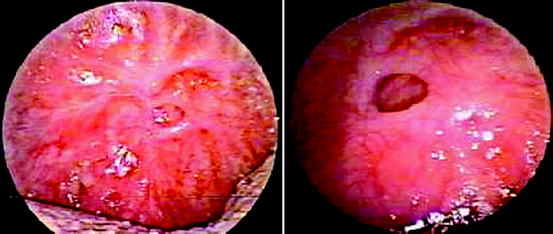
Fig. 6.2.9
Nasopharyngeal stenosis after aggressive UPPP
The surgical treatment of nasopharyngeal stenosis after UPPP is difficult, and unfortunately does not yield positive results in all cases. Often several surgical procedures and intermittent insertion of nasopharyngeal obturators are necessary [231, 369, 370]. We prefer to open the stenosis with scissors as laser surgery may lead to deep thermic lesions and uncontrolled scarring. It is of importance to insert a placeholder in the wound to avoid recurrence of the stenosis. We create such a placeholder out of 1 mm thick silicon foil as shown in Fig. 6.2.10. This has proven to be effective, easy to handle, and cost-effective.
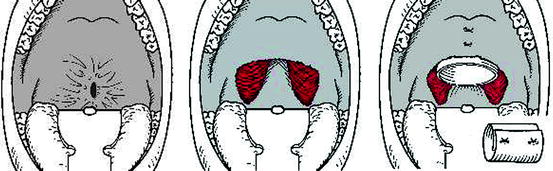
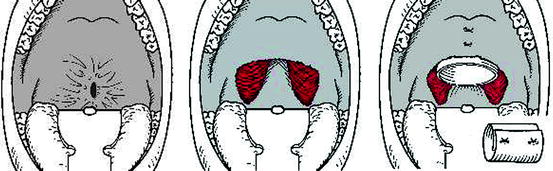
Fig. 6.2.10
Treatment of nasopharyngeal stenosis after UPPP. Stenosis (left). Situation after opening (center). Situation after insertion of placeholder made of silicon foil (right) (see small picture in the right lower corner)
Other authors use other kinds of custom-made nasal obturators (Fig. 6.2.11) [231]. Nowadays, we regard the appearance of a nasopharyngeal stenosis less as an inevitable complication, but as the result of an inadequate surgical technique.
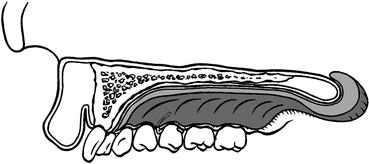
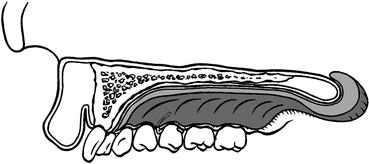
Fig. 6.2.11
Customized palate obturator with nasopharyngeal extension
Katsantonis [345] has classified the late-term complications after radical UPPP in descending frequency as follows:
Pharyngeal dryness and hardening
Postnasal secretion
Dysphagia
Incapability of initiating swallowing
Prolonged angina
Taste disorders
Speech disorders
Numbness of tongue
Permanent velopharyngeal incompetence (VPI)
Nasopharyngeal stenosis
A permanent rhinolalia aperta has not been observed in connection with the muscle-preserving technique described above. Though it must be said that we have observed this sign of a velar insufficiency in the case of patients, who alio loco received too radical surgery (resection of palate musculature and uvula). Several patients, who had received a tonsillectomy with UPPP, reported a positive change in timbre and resonance of their voice. Patients with speech professions (French teacher; radio announcer for Italian and French) and two professional musicians (wind instrument players) experienced no difficulties in resuming their jobs after a 3-4 week interval. Nevertheless, the indication should be made with special restraint for this patient group [75].
Goh et al. [235] published the study with the longest follow-up, namely 17-20 years after a radical UPPP according to the technique of Simmons et al. [676] on 49 unselected patients (now in a mean age of 67.1 ± 10.1 years) who had been operated between 1980 and 1983 for OSA at Stanford University. They investigated the quality-of-life outcomes of these patients by a retrospective chart review and telephone survey. On a visual analogue scale patients graded the clinical benefits and complications of UPPP with tonsillectomy. All patients had improvement of snoring, EDS, and nocturnal arousals after surgery. There was deterioration over time for all three benefits (67.3-40.8% for snoring; 49-34.7% for EDS; 22.4-14.2% for nocturnal arousals). Although the most common complication of UPPP was velopharyngeal insufficiency (28.5%), dry throat (22.4%) tended to cause more significant problems. Complaints of foreign body sensations were reported by 20.4%, swallowing problems by 24.4%, and speech alterations by 16.3% of the patients. Although 43 patients had preoperative sleep studies, only 22 returned for a postoperative sleep study. Of these 22 patients, only one (4.5%) was cured as defined by Riley (RDI < 20) [610]. Six (27.3%) patients had deterioration of sleep study results, whereas 15 (68.2%) were not changed significantly. Of the 21 patients with persistent OSA, 12 (57.1%) developed cardiovascular problems. In the group without postoperative sleep study, 16 of 27 (59.3%) developed cardiovascular consequences, three of them were deceased at the time of study. None of these patients sought or underwent any other medical therapy after UPPP. In this unselected group of OSA patients, 49 patients had a mean BMI of 31.1 ± 5.6 kg/m2 at time of operation, and 69.8% of 43 had severe sleep apnea according to the preoperative sleep study. We can learn a lot more from Goh’s et al. paper which reports on an unselected group of obese patients with mostly a severe OSA who were only treated with a radical UPPP and tonsillectomy.
6.2.5 Indications and Contraindications
Foremost, UPPP can eliminate the snoring sound of the so-called velum snorer. But it is not that easy to recognize with certainty the velum snorer. Clinically, the velum snorer displays characteristic anatomical traits of his or her soft palate, such as a long and/or wide uvula with lateral mucous membrane folds, a salient posterior palatine arch (webbing) (Fig. 6.2.12), a short distance between soft palate and pharyngeal posterior wall, and craniocaudal mucosal folds formation in the mesopharyngeal posterior wall. The velum snorer is especially distinguished by a snoring sound characterized by a base frequency of 25-50 Hz and a multitude of overtones, which results in a regular and harmonic sound pattern [644]. The UPPP has no effect in the case of a “tongue base snorer,” whose nighttime respiratory sounds are characterized by loud, hard, metallic, nonharmonic snoring with frequency amplitudes between 1,100 and 1,700 Hz.


Fig. 6.2.12
Soft palate. Yellow dots: caudal edge M palatoglossus. Green dots: caudal edge M. palatopharyngeus. White line: so-called webbing = distance of the free edge of the posterior palatine arch to the caudal edge of the M. palatopharyngeus
The literature provides only few prospective studies for OSA, which suggests the following selection or exclusion criteria for UPPP:
In general, obesity is a negative selection criterion. The limit for an isolated UPPP appears to lie at a BMI between 28 and 30 kg/m2.
A high AHI or ODI is a negative selection criterion for isolated UPPP. The absolute value is disputed; it seems to lie between 20 and 30 per hour. Above an AHI of 25, we pursue a multilevel surgery concept.
Large tonsils that are removed with UPPP are a positive selection criterion. If still existing, we always remove tonsils in the context of a UPPP for OSA.
Contradictory data are produced when radiocephalometric data are used for the selection of patients. A retrognathia or a micrognathia are negative selection criteria. In these cases the obstruction often lies behind the tongue.
A positive Müller maneuver (provoking of a collapse during inspiration against the artificially closed airway) in the context of the nasopharyngeal videoendoscopy has no predictive values; therefore, we do not employ it.
Even sleep endoscopy which is able to add to better patient selection in certain cases of SDB does not guarantee a positive outcome of UPPP although the finding of obstruction is found on palate-uvula level [279].
An analysis of the literature data yields the following exclusion criteria for an isolated UPPP, which in principle we already formulated in 1990 based on our own results [774]:
Chronic heart and/or lung diseases
Neurological/psychiatric illnesses in need of treatment
High anesthesia risk
Obesity; BMI > 30 kg/m2
Chronic alcoholism
Soporific drug abuse
Severity of OSA; AHI > 25
Severe bite misalignment
Narrow pharyngeal airway behind the tongue
Large distance between lower edge of mandibula to the hyoid
Certain craniofacial deformities
Too short soft palate
If indicated, we perform UPPP and T combined with rhinosurgery in the majority of patients. In these cases, the patient is forced to breathe through the mouth during the nasal packing (1-2 days). This leads to a heightened postoperative morbidity; but this is justifiable in the majority of cases. These patients need to be supervised, e.g., in the wake-up room immediately postoperatively (i.e., during the first 3-6 h after surgery). A supervision in an intensive care unit is usually not necessary [464]. Yet the issue of heightened postoperative morbidity should be discussed with the patient preoperatively, since in principle it is of course possible to perform nasal surgery and UPPP separately.
In the case of an AHI of above 25, we no longer perform isolated soft palate surgery. The experience of diminishing success rates with increased initial AHI has shown that in these cases the complete airway is affected by the disease. We therefore prefer a multilevel surgery concept for moderate and severe OSA, in which UPPP or its newer modifications with tonsillectomy play a central role (Chap. 10).
In children, UPPP is indicated only in exceptional cases as, for example, neurologically impaired children, craniofacial deformities, or Down’s syndrome [1, 310, 352, 365, 714]. We have only limited but positive experience in individual cases of M. Down and Pierre Robin Sequence.
As until today we have no safe tool to predict the outcome of UPPP in the individual patients they should be informed that UPPP alone can improve, not change or deteriorate their SDB. Therefore a postoperative sleep study is obligatory.
Take Home Pearls
UPPP is the surgical standard procedure for OSA if the site of obstruction is located at the level of the soft palate. If still present, tonsils need to be removed.
For primary snoring less invasive techniques provide comparable results and should therefore be favored.
There is no rationale for aggressive UPPP. Aggressive UPPP does not improve surgical success rates but definitely does increase complication rates.
Postoperative risk increases with severity of the OSA, BMI and accompanying other diseases. The surgeon must be aware of a possibly difficult intubation.
6.3 Recent Modifications of Uvulopalatopharyngoplasty
Wolfgang Pirsig and Thomas Verse
Core Features
Modifications of UPPP can be divided in two groups: the so-called uvulopalatal flaps and those techniques extending to lateral pharynx.
Uvulopalatal flaps are simple techniques that can be performed very quickly. These are used as alternatives to conventional UPPP. Short-term results are comparable to conventional UPPP. Long-term data do not exist so far.
Techniques addressing the lateral pharynx are recommended as second-line treatments after unsuccessful UPPP. First short-term data are promising.
In our millennium, several modifications of UPPP have been published, some of which have proven to be more effective in reducing pathological sleep parameters of patients with OSA on the short-term follow-up. There is the group performing uvulopalatal flaps [213, 293, 397, 502, 573] and the group including the lateral pharynx in their surgical concepts [87, 88, 540].
6.3.1 Surgical Technique
6.3.1.1 Uvuloplatal Flap
Uvulopalatopharyngoplasty (UPPP) is a relatively time-consuming surgical procedure, even in the case of sufficient surgical experience and practice. This fact has contributed to the interest generated by a modification, the uvulopalatal flap, developed at Stanford [573]. Today, we use a modification of the original technique with lateral extension to the tonsil bed, which impresses by its simple and fast mode of executing [293].
The preparations for surgery are identical to those described for UPPP. Surgery is performed under general anesthesia. The patient lies with reclined head, as in the case of tonsillectomy. In the case of OSA, the first step is always a gentle tonsillectomy (Fig. 6.3.1). In the case of patients who have already undergone tonsillectomy, there is no need for time-consuming opening of the scarring between the anterior and posterior palatine arch as with the UPPP technique. After this, incisions into the soft palate are made bilaterally on both sides of the uvula, as shown in Fig. 6.3.1.
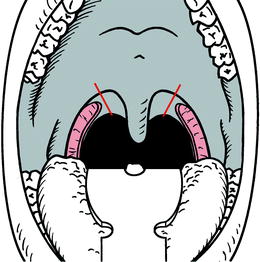
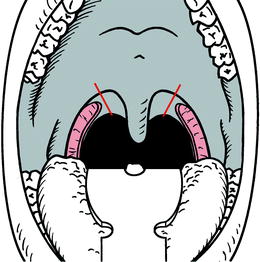
Fig. 6.3.1
Situation after tonsillectomy. Bilateral incisions into the soft palate on both sides of the uvula
At this point, the classic UPPP technique is left behind. The tip of the uvula is grasped with surgical tweezers, and excessive mucous membrane is resected (Fig. 6.3.2).
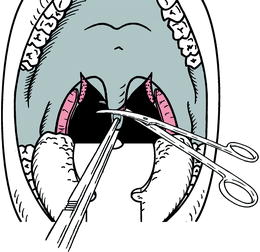
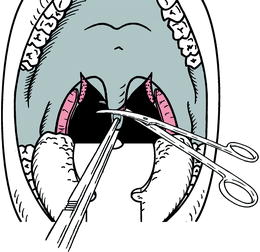
Fig. 6.3.2
Shortening of the uvula
The now exposed muscle tip of the uvula is also with the surgical tweezers folded toward cranial. The opening of the velopharyngeal flap is assessed, and the necessary extent of the uvulopalatal flap determined (Fig. 6.3.3). Powell et al. recommend marking the correct position of the uvulopalatal flap on the anterior side of the soft palate with tincture [573]. As a next step, in the marked area, the mucosa of the anterior palatine arch, the fat, and the underlying salivary glands are removed under careful preservation of the muscles (Fig. 6.3.3). The removal of the complete soft tissue above the musculature is crucial as only this can prevent the uvulopalatal flap from becoming too thick. A too thick uvulopalatal flap may lead to dysphagia, articulation impediments, and obstructed breathing.
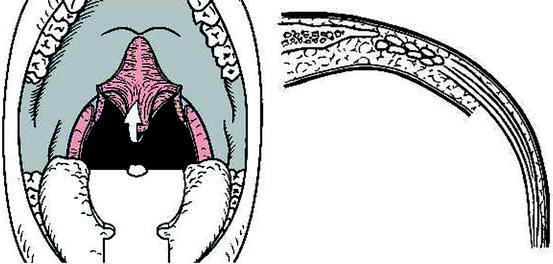
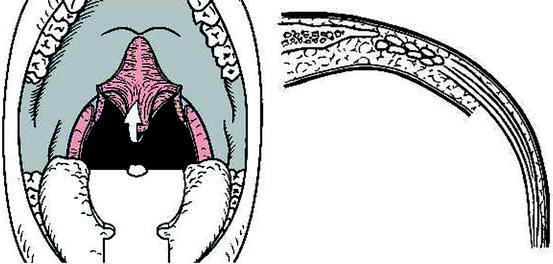
Fig. 6.3.3
Identifying the correct size of the flap by rotating the uvula upwards (left). Removal of mucosa, fat, and salivary glands in the estimated area. Lateral aspect of the soft palate (right)
Now, the uvula is loosely folded into the defect and worked in with atraumatic, resorbable suture material. We basically recommend a double suture with a thread thickness of 2.0 or 3.0, depending on the dimension of the soft palate. As a rule, 5 sutures are sufficient. This results in an uvulopalatal flap, which in its thickness is in accordance with the level of the surrounding soft palate (Fig. 6.3.4). Finally, lateralization of the posterior palatine arch is achieved by sewing together of the two palatine arches, comparable to the technique employed for UPPP (Fig. 6.3.4).
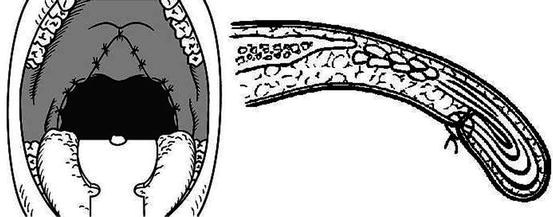
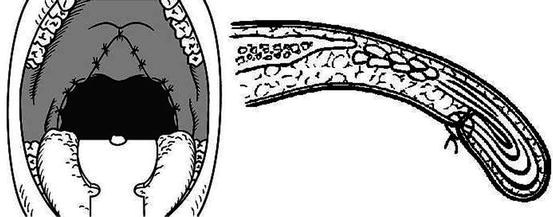
Fig. 6.3.4
Postoperative situation. Frontal aspect (left). Soft palate, lateral aspect (right)
The lateralization is achieved by deep intra-muscular sutures (2.0 resorbable thread, atraumatic needle), which are run through the posterior palatine arch (M. palatopharyngeus), through the base of the tonsil bed, and through the anterior palatine arch (M. palatoglossus). We always execute a double suture of the palatine arch; in our experience, a double suture significantly delays a tearing of these sutures. The aim of the lateralization is to prevent a potential traverse folding of the pharyngeal posterior wall. Figure 6.3.5 compares the pre- and postoperative situation.
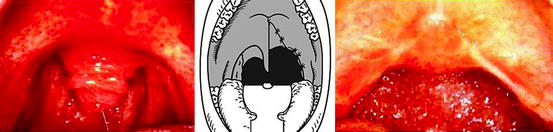
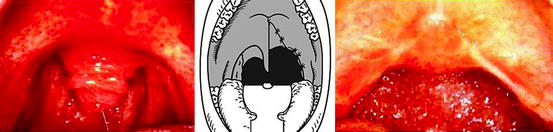
Fig. 6.3.5
Uvulopalatal flap (Mannheim technique). Preoperative finding (left). (Middle) Diagram comparing preoperative (left side) and postoperative (right side) situation. (Right) Situation 6 weeks postoperatively
In 2003, Li et al. [400] published their modification of an extended uvulopalatal flap (EUPF). Under general anesthesia and after bilateral tonsillectomy, the retropalatal space in both the anteroposterior and lateral dimensions is expanded by incisions of the supratonsillar fossae. Mucosa and submucosal fat are removed with preservation of the muscle, and the tip of the uvula is excised. From a point in the midline approximately 5-10 mm below the posterior end of the hard palate, a V-shaped incision is made to the upper poles of the bilateral tonsillar fossae. The denuded uvula and soft palate now comprise the EUPF, which is imbricated and sutured to the residual mucosa of the soft palate using 2-0 Vicryl. The new tonsillar fossa is closed to decrease the dead space. The anterior and posterior pillars are approximated using mattress sutures with maximal lateralization.
For treating patients with SDB and with those who had their tonsils already removed, Friedman et al. [213] presented the Z-palatoplasty (ZPP) in 2004. After outlining two adjacent flaps on the palate – together they look butterfly-shaped – only the mucosa of their anterior aspect is removed. Then, the two flaps are separated from each other by splitting the palatal segment down the midline. A two-layered closure brings the midline all the way to the anterolateral margin of the palate. The final result creates 3-4 cm of distance between the posterior pharynx and the palate. In addition, the lateral dimension of the palate is usually doubled to approximately 4 cm. A uvula-similar structure is not visible although both the uvula muscles are preserved within the new palate. In addition, all patients also underwent tongue base radiofrequency with the application of a total of 4,500 J in monthly intervals.
6.3.1.2 Lateral Pharyngoplasty
In 2003, Cahali [88] introduced the lateral pharyngoplasty (LP) procedure for treating OSA in adults with the intention to splint the lateral pharyngeal muscular walls. These regions, thickened and exceedingly collapsible during respiration in these patients, have a key role in the pathophysiology of OSA. After bilateral tonsillectomy the superior pharyngeal constrictor muscle within the tonsillar fossa (outer pharyngeal muscular layer) is sectioned and sutured to the anterior pillar to provide support to the lateral pharyngeal wall. Then, a Z-plasty between the lateral free margin of the soft palate and the palatopharyngeus muscle is performed, thus providing lateral support to the soft palate. In addition, a partial uvulectomy is done. Therefore, the LP supports the pharynx through postoperative retraction of the inner and outer pharyngeal muscular layers.
Pang and Woodson modified Cahali’s technique and developed the expansion sphincter pharyngoplasty (ESP) for a selected group of OSA patients with small tonsils, Friedman [220] stage II or III, and lateral pharyngeal wall collapse noted on endoscopic examination [540]. Their principle is to isolate the palatopharyngeus muscle as the main part of the lateral pharyngeal wall bulk and rotate this muscle superoanterolaterally, to create the lateral wall tension and remove the bulk of the lateral pharyngeal walls. After bilateral tonsillectomy, the inferior end of the palatopharyngeal muscle is transected horizontally and rotated superolaterally with a figure 8 suture, through the muscle bulk itself, with a 3-0 resorbable suture with round body needle. The muscle is sufficiently isolated and left with its posterior surface partially attached to the posterior horizontal superior pharyngeal constrictor muscles. A superolateral incision is made on the anterior pillar arch bilaterally, identifying the arching fibers of the palatoglossus muscle. The palatopharyngeus muscle is then attached to the arching fibers of the soft palate anteriorly with a figure 8 suture, through the muscle bulk itself, with 3-0 resorbable sutures. After a partial uvulectomy, the anterior and posterior tonsillar pillars are approximated with resorbable sutures.
6.3.2 Effectiveness for SDB
Concerning the effectiveness of the UPPP modifications for treatment of sleep-related breathing disorders only few data have been published. Only one publication addresses the therapy of primary snoring [502]. Sixty-five patients received as sole surgical procedure an uvulopalatal flap. At follow-up 14 months postoperatively, both a significant subjective and objective reduction of the snoring sounds could be demonstrated. The polysomnography showed an unchanged RDI (preoperatively 3.2 ± 1.2 vs. 3.0 ± 1.8 postoperatively).
More data exist concerning the efficacy of the recent UPPP modifications for the treatment of OSA (Table 6.3.1). In an initial publication, 80 patients were diagnosed prospectively (EBM 3b) [573]; 59 of them received an uvulopalatal flap; the remaining 21 underwent a conventional UPPP. The results in regard to the polysomnographic and subjective findings were comparable in both groups. But it must be said that in 84% of the cases additional surgery on the hypopharynx was performed in the same session. Therefore, this study does not allow for inferences regarding the isolated effect of the uvulopalatal flap.
Table 6.3.1
Effectiveness of uvulopalatal flap and other recent modifications of UPPP for OSA
Author | N | Technique | Add. proc. | Follow-up (months) | AHI pre | AHI post | Success (%) | ESS pre | ESS post | EBM |
|---|---|---|---|---|---|---|---|---|---|---|
Hörmann et al. [292] | 30 | Flap | None | 1.5 | 19.2 | 8.2 | 46.7 | 5.5 | 3.0 | 4 |
Neruntarat [497] | 31 | Flap | GA HS | 8.0 | 48.2 | 14.5 | 73.7 | 14.9 | 8.2 | 4 |
Neruntarat [499] | 32 | Flap | HS | 8.1 | 44.5 | 15.2 | 78.0 | 14.1 | 8.2 | 4 |
Neruntarat [498] | 49 | Flap | GA HS | 39.4 | 47.9 | 18.6 | 65.2 | 15.9 | 6.2 | 4 |
Li et al. [399] | 33 | EUPF | None | 6.0 | 41.6 | 12.5 | 81.8 | No data | No data | 4 |
Cahali [88] | 10 | LP | None | 6.0 | 41.6 | 15.5 | 53.3 | 14.0 | 4.0 | 4 |
Friedman et al. [212] | 25 | ZPP | RFT TB | 6.0 | 41.8 | 20.9 | 68.0 | 12.5 | 8.3 | 2b |
Cahali et al. [87] | 15 | LP | Nasal surgery | 7.9 | 41.6 | 15.5 | 53.3 | 14.0 | 4.0 | 2b |
Li et al. [395] | 105 | EUPF | None | 12.0 | 43.8 | 15.0 | 80.0 | No data | No data | 4 |
Li et al. [396] | 55 | EUPF | None | 6.0 | 43.6 | 21.1 | 82.0 | 11.8 | 7.5 | 4 |
Li et al. [397] | 84 | EUPF | None | 6.0 | 46.5 | 14.6 | No data | 11.0 | 7.2 | 4 |
Li et al. [400] | 12 | EUPF | LLT/MLG | 6.0 | 53.5 | 30.4 | 41.7 | No data | No data | 3b |
Li et al. [398] | 50 | EUPF | None | 6.0 | 44.5 | 13.4 | 84.0 | No data | No data | 4 |
Hsieh et al. [297] | 6 | EUPF | MLG | 6.0 | 50.7 | 11.6 | No data | No data | No data | 4 |
Lin et al. [417] | 55 | EUPF | None | 6.0 | 43.6 | 12.1 | No data | 11.8 | 7.2 | 3b |
Baisch et al. [35] | 83 | Flap | RFT TB, HS | 1.0 | 36.4 | 19.4 | 59.7 | 9.7 | 6.4 | 4 |
Verse et al. [762] | 45 | Flap | RFT TB, HS | 4.3 | 38.9 | 20.7 | 51.1 | 9.4 | 7.2 | 3b |
Verse et al. [762] | 15 | Flap | RFT TB | 5.9 | 27.8 | 22.9 | 40.0 | 9.1 | 4.1 | 3b |
Pang and Woodson [540] | 23 | ESP | None | 6.5 | 44.2 | 12.0 | 82.6 | No data | No data | 2b |
Huang and Cheng [301] | 50 | MEUP | None | 6.0 | 37.9 | 6.1 | 80.0 | 9.8 | 5.2 | 4 |
All | 839 | 8,24 | 41.92 | 15.61 | 70.10 | 11.55 | 6.68 | B |
Our initial evaluation of 30 patients [293] who received an isolated uvulopalatal flap according to the technique described above resulted in a statistically significant reduction of the AHI (Table 6.3.1). Further significant improvements were found in the objectively determined snoring index (45.3 vs. 21.0) and in the minimal oxygen saturation (79.2% vs. 87.5%).
Better results have been recently reported by Li et al. (Table 6.3.1), who use an extended technique not comparable to our own [400]. These authors also report a significant improvement of the snoring index and the minimal oxygen saturation. Furthermore, a signficant improvement of daytime sleepiness and of quality of life in 7 of 8 domains of the SF-36 was observed.
Friedman et al. [213] compared the outcomes of ZPP (N = 25, BMI 31.0 kg/m2) with UPPP (N = 25, BMI 29.6 kg/m2) in patients with OSA and with already absent tonsils after 6 months follow-up. All of them also received a radiofrequency treatment of the tongue base. Subjective improvement was good for both groups, but objective clinical improvement was significantly better for the ZPP group. The AHI in the ZPP group was reduced from 41.8 to 20.9 and respectively from 33.4 to 25.2 in the UPPP group (Table 6.3.1). The authors consider a very significant limitation of their procedure that there is no landmark to describe the size of the flaps, that the procedure is technically more difficult and takes longer time than the classic UPPP. Further, the ZPP results in the absence of a uvula and many patients complain of a “foreign-body” sensation in the throat. We consider an essential limitation of this study that the efficacy of ZPP or UPPP cannot really be estimated because of the concomitant treatments of the tongue base with radiofrequency. In a more recent paper, the authors recommended ZPP as an effective and safe second-line treatment after unsuccessful UPPP [211].
In a randomized controlled trial, Cahali et al. [87] compared the clinical and polysomnographic outcomes of the LP procedure (N = 15) with UPPP (N = 12) according to the technique of Fairbanks [184] in adults with OSA incompliant of nCPAP. Concomitant nasal surgery was performed in 5/15 LP patients and in 8/12 UPPP patients. Comparing the preoperative data with those after a mean follow-up of 8 months, in the LP group a statistically greater reduction of body weight (mean BMI: 29.3 vs. 27.7 kg/m2), excessive daytime sleepiness (ESS: 14 vs. 4), and AHI (mean AHI: 41.6 vs. 15.5) was found. There also was a statistical increase in the amount of deep sleep and a reduction of morning headache. In the UPPP group, there were no significant changes in the polysomnographic parameters (mean AHI: 34.6 vs. 30.0), while mean excessive daytime sleepiness also was significantly reduced (ESS: 14 vs. 5). Interestingly, there were similar cross-sectional measurements of computed tomography of the pharyngeal airways while awake in both groups preoperatively and at follow-up.
In a prospective, randomized controlled trial, Pang and Woodson [540] compared the outcomes of expansion sphincter palatoplasty (ESP) (N = 23) with UPPP (N = 22) in selected patients with OSA with a mean BMI of 28.7 kg/m2 after a mean follow-up of 6.5 months. The AHI decreased from 44.2 to 12 (p < 0.005) following EPS and from 38.1 to 19.6 (p < 0.005) in the UPPP group. Using Sher’s criteria, success was 82.6% in ESP compared with 68.1% in UPPP (p < 0.05). When selecting an arbitary threshold of a 50% reduction in AHI and AHI less than 15, the ESP success rate was 78.2%, compared with that of the UPPP group at only 45.5% (p < 0.005). Postoperative endoscopic findings also demonstrated significant reduction of lateral pharyngeal wall collapse in the EPS group. This was not the case in the UPPP group, with some patients still having significant lateral pharyngeal wall collapse noted on Müller’s maneuver, postoperatively.
6.3.3 Postoperative Care and Complications
The immediate healing phase after uvulopalatal flap proceeds as after conventional UPPP. This of course also especially holds of the healing phase after the additionally performed tonsillectomy. Therefore, we implement the same postoperative management as after UPPP, and refer the reader to our discussion in Chap. 6.2.
Several studies [87, 213, 293, 397, 498, 540, 573] also furnish information concerning the potential complications after uvulopalatal flap or LP.
6.3.3.1 Uvulopalatal Flap
Focusing on the uvulopalatal flap, it has to be said that orginally the uvulopalatal flap was regarded as a potentially reversible surgical technique. We want to challenge this evaluation; we do not consider the uvulopalatal flap as in principle reversible. Our experience has shown that the scarrings after completed healing of the wound cannot easily be opened up again.
The dreaded velopharyngeal incompetence has clinically neither been observed by the Stanford or our study group. Neruntarat described transient nasal regurgitation in two of his patients (4%). In the Finkelstein test [199], a flow of liquid into the nose was demonstrated endoscopically in 3 of our 30 patients, without it becoming clinically relevant. In the longer run, a nasopharyngeal reflux could no longer be demonstrated.
Although a few patients complained of the sensation of having a lump in the throat (7%; 4/55) and mild nasal regurgitation (6%, 3/55) after EUPF, none of them complained about any physical limitation in their daily activities [397].
A nasopharyneal stenosis, as it has been described after other, especially aggressive soft palate techniques, has not been observed either after uvulopalatal flap or after LP.
In the first weeks postoperatively, irritations and foreign-body sensations are to be expected. This is due to the principle of the surgery, which transports mucous membrane segments which originally have been in the posterior side of the velum to the anterior side. As a result, some patients initially experience an irritation in the nasopharynx when it comes to a contact with the flap. These sensations disappear after several weeks.
Permanent foreign-body sensations develop, especially in cases where not merely an incision of the posterior palatine arch is performed, but a cut is also performed in the anterior palatine arch. This is necessary in rare cases, in order to achieve a sufficient opening of the velopharyngeal segment; but this should always be performed as cautiously as possible, in order to not endanger the sensible innervation of the flap and the uvula, which pulls from laterocranial toward mediocaudal. If one abides by this principle, then such permanent foreign-body sensations, which severely burden the patient, can be avoided.
Our own investigations concerning language and articulation have not brought to light any disturbances in this respect.
As a further complication, a hematoma in the area of the uvula tip with secondary inflammation, which led to a revision of the flap, and a suture insufficiency with partial flap insufficiency, has been described [573]. We also have observed suture insufficiencies with partial or complete dislodgement of the flap from its bed. These suture insufficiencies can be reliably avoided with the help of an adequate suture technique with deep-reaching double sutures and atraumatic suture material. In order to prevent unnecessary postoperative wound pain, it must be ensured that the knots are tightly bound, but that the tissue is not squashed. A slack adaptation of the wound edges is aimed at. Some surgeons consider the use of knot slides as very helpful in this context.
These data are comparable with those of gentle UPPP, and they corroborate the assumption by Finkelstein, according to which the proof of a subclinical nasopharyngeal reflux in the first weeks after soft palate surgery depends on the intensity, with which the surgeon hunts it out.
6.3.3.2 Other Techniques
Pang and Woodson [540] reported of no significant complications in either group following ESP or UPPP. All patients started soft diet consumption on the first postoperative day. There was no significant difference in the use of narcotics or pain relief in the two groups, and there was no long-term dysphagia or voice change.
Friedman et al. [213] found that patients undergoing ZPP used narcotic pain medication for 6.4 days and required 6.4 days to return to a normal diet as compared with 9.4 days and 10.3 days, respectively in UPPP patients (p < 0.005 resp. p < 0.002). Tongue base infections, secondary to radiofrequency treatments, were found in 1 ZPP patient and 2 UPPP patients. Temporary velopharyngeal insufficiency (VPI) between 2 and 60 days was reported in 12/25 ZPP and 7/25 UPPP patients. The majority of postoperative complications were related to throat discomfort, including foreign-body sensation (11 of ZPP vs. 17 of UPPP), dysphagia (1 ZPP vs. 11 UPPP), postnasal drip (3 ZPP vs. 4 UPPP), and dry throat.
As to complications there was no bleeding, nasopharyngeal stenosis, or permanent palatal incompetence [87]. In the first 10 patients of the LP group, there were significant swallowing problems with dysphagia over a mean of 20.4 days (range 8-70 days). Four patients in each group reported mild episodes of oronasal reflux of liquids which disappeared within 2-6 months.
6.3.4 Indications and Contraindications
The uvulopalatal flap is a comparatively modern procedure. We see the indication for the most part in the area of OSA. For primary snoring, there exist techniques such as radiofrequency surgery, soft tissue implants, and other procedures, which can be used on an outpatient basis and under local anesthesia. Given the comparable efficacy, these procedures are to be preferred also in respect to the costs involved.
UPPP and uvulopalatal flap are similar in regards to their basic principle and their effects upon the upper airways; therefore, we assume the same indication areas for both surgical techniques, when they are employed in a muscle-preserving manner. For the isolated soft palate surgery (uvulopalatal flap with tonsillectomy) we perform either UPPP or the uvulopalatal flap as the first-line procedure in moderate to moderately severe OSA. In combination with surgery on the hypopharyngeal segment we also use the uvulopalatal flap for severe OSA.
On the whole, we see few advantages for the uvulopalatal flap, especially if a tonsillectomy had been performed prior to surgery; but in the end it appears that every surgeon will have to choose for themselves the technique with which they achieve better surgical results.
6.3.4.1 Extended Techniques
For treating OSA using EUPF, Li et al. [397] selected patients with a normal weight and a narrowed retropalatal space judged by nasofibroscopy with Müller maneuver and 3-dimensional computed tomography.
Friedman et al. [213] published a longer list of selection criteria, among them are the failure of CPAP or dental appliances, patients without tonsils or those who underwent prior tonsillectomy, Friedman OSA stages II or III, and the appearance of obstruction at the level of the soft palate (diagnosed by fiberoptic hypolaryngoscopy and Müller maneuver).
Velum surgery including the lateral pharynpgoplasty (LP and ESP) is indicated to splint the lateral pharyngeal muscular walls and to remove or reduce the bulk of the lateral pharyngeal walls. Therefore, Pang and Woodson [540] selected patients with small tonsils (tonsil size 1 and 2), BMI < 30 kg/m2, Friedman clinical stage II and III [220], and lateral pharyngeal wall collapse noted on endoscopic examination who cannot tolerate CPAP. They excluded patients with large tonsils for whom they recommended the traditional UPPP.
Cahali et al. [87, 88] selected as inclusing criteria the presence of a low-lying soft palate (most of the patients were Malampatti type 3 with few type 4) associated with a fiberoptic pharyngoscopy finding of narrowing or collapse in the retropalatal region without narrowing in the hypopharynx (Fujita type 1), both at rest and during the Muller maneuver. All their patients had bulky lateral oropharyngeal tissues (either the tonsil or the posterior tonsillar pillar). They excluded patients with weight over 130 kg, morbid obesity, the presence of uncontrolled hypothyroidism, and gross maxillary or mandible deformities.
Summing up the results of the cited studies on uvulopalatal flaps and other recent modifications of UPPP we find some positive developments and also some limitations. All described modifications try to improve shortcomings of the conventional UPPP, and especially the LP attacks the problems of the lateral pharyngeal walls [87, 88, 540]. Most studies report on more reduction of sleep parameters than achieved with conventional UPPP. Clear criteria for patient selection are only given by some authors [87, 213, 540], especially for patients after prior tonsillectomy. Quality-of-life evaluation helps to improve the subjective outcomes of velum surgery [213, 397, 400].
Some surgical procedures are rather invasive and temporarily disturb the coordination of the velar muscles which results in postoperative problems with swallowing. Also the velar sensory innervation is disturbed by large incisions, thus enhancing the preexisting polyneuropathy of the patients with OSA. Another disadvantage is the uvulectomy performed by several working groups [88, 213, 397, 540, 573]. Most authors use nasopharyngeal endoscopy and Müller maneuver while awake to diagnose the level of pharyngeal obstruction, methods of questionable diagnostic value. No study described the use of sleep endoscopy. The numbers of operated patients are mostly small, especially when compared with conventional UPPP. The follow-up is very short, between 1.5 and 8 months. Most publications [87, 213, 397, 573] present outcomes of a two-level surgery instead of isolated velum surgery. Therefore, no long-term conclusions on the definite value of these new modifications are possible.
Take Home Pearls
The uvulopalatal flap is an alternative to conventional UPPP, especially in patients after prior tonsillectomy.
As in conventional UPPP complications frequently occur after aggressive surgery. The muscles of the soft palate should be handled with care. There is no need for broad resections.
Techniques addressing the lateral pharynx should be reserved to patients with still narrow velopharyngeal segments after unsuccessful UPPP.
6.4 Laser-Assisted Uvulopalatoplasty (LAUP)
Thomas Verse and Wolfgang Pirsig
Core Features
There are two kinds of laser-assisted soft palate surgeries. The so-called laser uvulopalatoplasty (LUPP) is similar to conventional UPPP, requires general anesthesia, and should be regarded as a modification of UPPP.
The so-called laser-assisted uvulopalatoplasty (LAUP) comprises a resection of redundant mucosa of the posterior tonsillar pillar and the uvula. Some authors perform a parauvular incision into the muscles of the soft palate in order to achieve additional stiffening. Instead of lasers, various other technical aids can be used as well (LAUP related procedures).
LAUP and related procedures are easy and quick to perform. They only require local anesthesia without sedation in an outpatient setting.
LAUP and related procedures can be combined with other surgeries for SDB.
Because of substantial postoperative pain, LAUP induces significant postoperative morbidity.
Potential complications are numerous. Most of them can be avoided, be a gentle resection of only mucosa.
LAUP and related procedures are only indicated to treat simple snoring. They are not sufficiently effective in treating OSA.
Since 1981, uvulopalatopharyngoplasty (UPPP) has gained acceptance as routine therapy in the surgical treatment of sleep-disordered breathing [224]. As an essential modification of the conventional UPPP technique, a laser-assisted velum surgery was developed, which was introduced by Carenfelt [91] in 1986, and which he called “laser uvulopalatoplasty” (LUPP). While Carenfelt performed the LUPP under general anesthesia and with sutures similar to those used with the UPPP, at the end of the 1980s, Kamami [339] introduced a further modification, which was carried out under local anesthesia in several sessions on an outpatient basis. This modification was called “laser-assisted uvulopalatoplasty” (LAUP); it has spread rapidly in Europe and since 1992 has also become increasingly popular in the United States [118].
Up to March 2008, more than 120 articles on LAUP have been published worldwide; however, only some of these articles are clinically relevant. Therefore, the present outline intends to structure the literature on the basis of clinical criteria in order to highlight the significance of LAUP/LUPP for the everyday routine work. In particular, the indication for LAUP/LUPP, their surgical prospects of success, and the complications associated with the procedure will be illuminated.
6.4.1 Surgical Techniques
We found 24 different descriptions of laser surgical techniques of the soft palate, explaining in detail which anatomical structures of the soft palate are involved in the surgery. Most of these publications are illustrated with explanatory drawings or photographs. Although the variability of the techniques described is very high, three basic techniques can be identified.
The oldest technique, applied by Carenfelt already in 1986 [91], is the LUPP, which some working groups [91, 809] reported to be more gentle to muscles, while others regarded it as being substantially more radical [197, 371]. The procedure performed with the LUPP is similar to that carried out with the UPPP, which means the preparation also extends to the pharyngeal walls and partly to the tonsils (Fig. 6.4.1). The Carenfelt and Haraldsson working group uses suture techniques for the adaptation of the posterior tonsillar pillar to the anterior tonsillar pillar in order to prevent uncontrolled scarring.
Most authors apply the LAUP technique introduced by Kamami [339]. The uvula is partly or totally removed. Then, two paramedian full-thickness, through-and-through trenches are made over the soft palate, on either side of the uvula, to a height of 1-2 cm. With few exceptions, the LAUP is performed under local anesthesia in an outpatient setting. There exists a more gentle procedure performed in several (up to five) sessions (Fig. 6.4.2) and a radical “one-stage-technique” (Fig. 6.4.3).
In most cases, the CO2-laser is used, sometimes the Nd:YAG [798] or the KTP laser [338]. No comparative information pointing to differences between various laser types has been found in the literature yet. However, Ducic et al. [164] were able to show in an animal test performed on six dogs that the CO2-laser caused deeper thermal tissue damage and more intensive scarring than the conventional UPPP technique using bipolar coagulation.
According to our experience, we see the most advantages in a cautiously performed modified Kamami technique [775]. We strongly advise against radical incisions into the palatopharyngeal and the palatoglossal muscles. As we know from our extensive experience from the UPPP surgery, there is no rationale for an aggressive surgical technique. The surgical outcome will not improve after a more radical procedure, but the incidence of severe complications will increase. We do not believe that there are no or only little complications after procedures like the one-stage LAUP (Fig. 6.4.3) as reported by Kamami [340].
Based on our experiences we developed a modification of the multiple-stage Kamami technique. We operate on the sitting awake patient. In general, there is no need for sedation. We perform a local anesthesia using 5-6 mL prilocaine (2%) with adrenaline (0.01%). Topical anesthesia is not advantageous because it often causes hypersalivation forcing the patient to swallow frequently. When we started to do LAUP surgery we used the CO2 laser (8 W, continuous wave, superpulsed mode) in the majority of the cases. Important is the use of a backstop protecting the posterior pharyngeal wall from the laser beam. Comfortable to use in contact mode is the KTP laser. Today, we predominately use mono- or bipolar high-frequency cutting instruments mostly in argon atmosphere, the latter being used to reduce thermal penetration into the tissue. As no lasers are used, all these technique are subsumed using the term RAUP (radiofrequency-assisted uvulopalatoplasty). Depending on the devices used, there is little smoke formation. The staff does not need to use glasses to protect his or her eyes from the laser beam. To sum it up, we do not see any need for lasers for this kind of surgery. In our experience, it is much less important which surgical tool is used than to use an appropriate surgical technique.
While the tongue is held down with a blade, an inverse V-shaped incision is made bilaterally to the uvula, only cutting about 5 mm into the anterior pillar of the soft palate (Fig. 6.4.4).
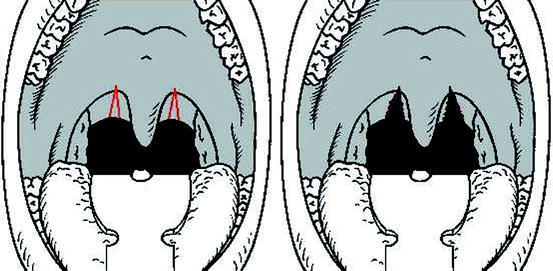
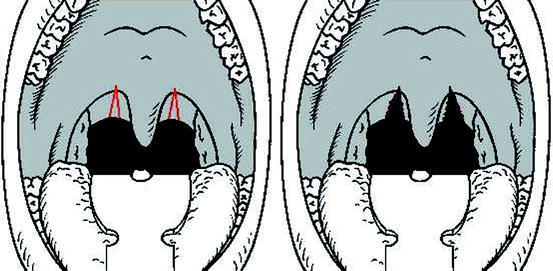
Fig. 6.4.4
(Left) palatal incision lines. (Right) incisions done
If bleeding occurs it has to be coagulated carefully. To complete the procedure the tip of the uvula is pulled downwards with a forceps. Thereby the uvula muscle becomes apparent. Preserving muscular tissue the redundant mucosa is taken away (Fig. 6.4.5).
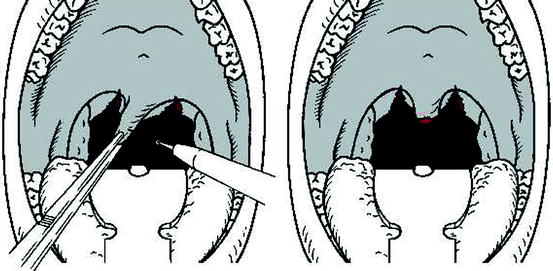
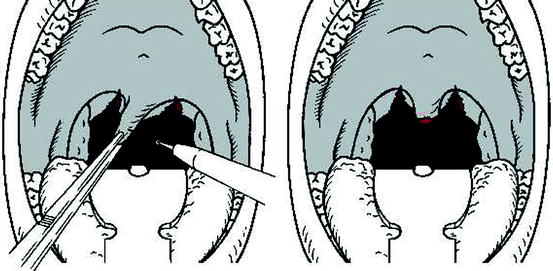
Fig. 6.4.5
(Left) uvula pulled downwards with forceps. (Right) uvula shortened
Figure 6.4.6 shows peri- and postoperative photographs of our technique taken in general anesthesia during one of our surgical courses.
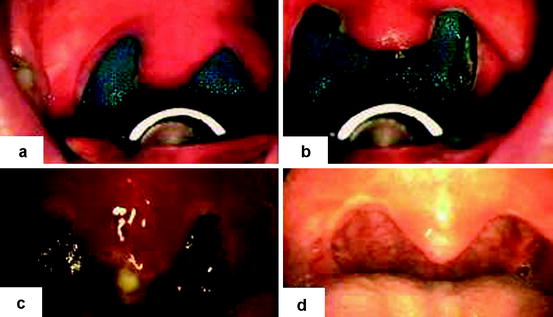

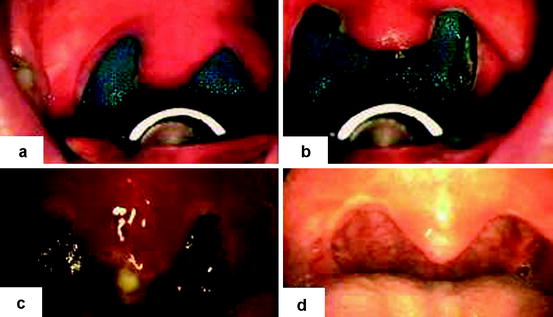

Fig. 6.4.6
Two cases of the Mannheim/Ulm/Hamburg Technique of LAUP. First case (a-d): (a) Preop. (b) immediately after surgery. (c) Six days postop. (d) 2 months postop. Second case (bottom). (Left) 2 weeks after surgery. (Right) three months after surgery.
6.4.2 Effectiveness for Simple Snoring
Up to now, there are no generally accepted techniques to quantify snoring. In the literature, either visual analogue scales (VAS) usually filled out by the patient’s bed partner or the so-called snoring indices (SI) based on different algorithms analyzing the recorded snoring sounds during sleep studies are used to describe the effectiveness of LAUP for simple snoring. Others use simple questionnaires with items such as “Do you still snore?” to verify treatment success.
Relevant data from prospective studies using VAS to evaluate the subjective improvements of either LUPP or LAUP for simple snoring are given in Tables 6.4.1 and 6.4.2. Extremely varying definitions of success complicate the interpretation of the results.
Table 6.4.1
Effectiveness of LUPP for simple snoring
Author | N | Follow-up (months) | VAS | VAS pre | VAS post | Success rate (%) | Def. of success | Laser | EBM |
|---|---|---|---|---|---|---|---|---|---|
Carenfelt [91] | 60 | 3-4 | 1-4 | No data | No data | 85 | Red >1 | CO2 | 3b |
Wennmo et al. [809] | 10 | 2-36 | 0-3 | 3 | 0.15 | 80 | VAS ≤1 | CO2 | 4 |
Albu et al. [7] | 90
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|