CHAPTER 27 Patient Positioning for Spinal Surgery
Equipment
Table
A basic electric operating table may be used for many spinal procedures (Fig. 27-1). Operations in the supine position, such as anterior cervical procedures and anterior lumbar fusions in the distal lumbar spine (L3-S1), are easily performed with such a table. Reversing the table may improve clearance under the table for the fluoroscopic unit. A lateral approach for thoracic, thoracolumbar, and lumbar procedures may also be performed on an electric table. For thoracoabdominal and retroperitoneal flank approaches, it is often helpful to place the level of pathology at the table break and flex the patient laterally.
There are many advantages to modular spine-specific operating tables such as the Jackson Spinal table (Mizuho OSI, Union City, CA) (Fig. 27-2). The carbon fiber frame is radiolucent and low profile to allow 360-degree fluoroscopy and the use of intraoperative CT scanners such as the O-arm (Medtronic Navigation, Louisville, CO). Modular components allow customization for each procedure and for a wide range of patient phenotypes. The head may be secured in a foam headrest, in a rigid fixator, or with traction. The legs may be supported in a sling to allow lumbar flexion or on a rigid tabletop to enhance lordosis (Fig. 27-3). Finally, intraoperative repositioning for anterior-posterior or posterior-anterior surgery is facilitated with a rotational capability that obviates the need for moving the patient from one table to another.
Principles of Positioning
Patient Safety and Protection
Neuropathies and Prevention
Ulnar neuropathy, one of the most common postoperative neuropathies, accounts for a third of all nerve injury claims in the American Society of Anesthesiologists Closed Claims Study database.1 Although the etiology of postoperative peripheral nerve injury is not entirely known, it is thought to be related to intraneural capillary ischemia resulting from nerve overstretch or compression, perhaps exacerbated by prolonged intraoperative hypotension. The ulnar nerve appears to be more vulnerable to ischemia than the median and radial nerves, with a reported incidence of 0.04% after noncardiac surgery to 37% in one series of cardiac patients who underwent detailed postoperative sensory testing. The time of onset of ulnar nerve symptoms varies from immediately after surgery to 3 days postoperatively. The duration of symptoms tends to vary across reports, with some completely resolving spontaneously in days and others persisting for years after the initial insult.2 Risk factors for postoperative ulnar neuropathy include diabetes, increased age, and male gender.3
Anatomically, the ulnar nerve appears to be particularly susceptible to direct compression as it courses through the superficial condylar groove at the elbow. Elbow flexion, especially to greater than 110 degrees, can tighten the cubital tunnel retinaculum and directly compress the nerve,4 and external compression in the absence of flexion may compromise the nerve. With the patient in the supine position, direct pressure on the ulnar nerve at the elbow is significantly higher if both forearms are pronated than if they are in a neutral and supinated position (Fig. 27-4).5
Brachial plexus neuropathy may have findings similar to ulnar neuropathy but may additionally be characterized by symptoms such as shoulder pain, scapular winging, and shoulder weakness. The incidence of brachial plexopathy during posterior spinal surgery has been estimated to be between 3.6% and 15%, as compared with 0.02% in a large study of 15,000 general surgical patients. Most patients achieve partial or full functional recovery, although some have persistent symptoms at late (1- to 3-year) follow-up.6,7
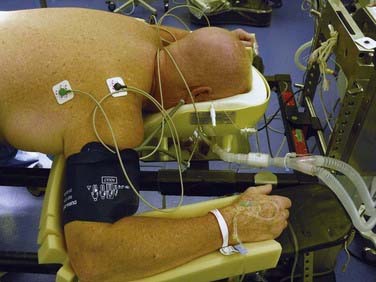
Some investigators have suggested intraoperative somatosensory evoked potential (SSEP) monitoring as a way to detect impending nerve injury. One retrospective study of 1000 spinal surgeries determined that the overall incidence of position-related upper extremity SSEP changes was 6.1%, with the lateral decubitus position (7.5%) and prone “superman” position (7.0%) having the highest incidence of position-related upper extremity SSEP changes. In this study, postoperative deficits did not develop in any patient who had positionally reversible SSEP changes.8
Lower extremity neuropathies have not been well studied in spinal surgery because they typically occur in patients undergoing surgery in the lithotomy position and after lower extremity orthopedic procedures. Injury to the common peroneal nerve has been reported more frequently than injury to any other lower extremity peripheral nerve, probably because of its vulnerable anatomic location. The common peroneal nerve is fixed in a superficial location as it traverses the head of the fibula, which leaves it susceptible to direct compression injury by devices that hold the legs in place. The legs should be padded and well protected at the level of the fibular head, particularly for procedures in the lateral decubitus position.9
In the event of a new postoperative neurological deficit, it is important to distinguish peroneal nerve injury from an acute L5 radiculopathy. A peroneal neuropathy is characterized by complete plegia of dorsiflexion and eversion without significant pain complaints, whereas an L5 radiculopathy usually results in dermatomal pain and sensory deficit accompanied by weakness of dorsiflexion, toe extension, and foot inversion.10
The lateral femoral cutaneous nerve (LFCN) originates from the L2-3 nerve roots and travels along the lateral border of the psoas major muscle and across the ilium toward the anterior superior iliac spine (ASIS). Because of its anatomic exit below the ASIS, compression neuropathy of the LFCN by posts or pads that support the pelvis may develop in patients who are placed in the prone position. In patients who sustain perioperative injury to the LFCN, hypoesthesia of the anterolateral aspect of the thigh usually develops, but some experience pain and dysesthesia as well. Few studies have been conducted to assess the incidence of positioning-related LFCN injury, although most estimates are around 20%. One study in particular estimated the incidence of LFCN injury to be 23.8% in patients who underwent prone spinal surgery with use of the Relton-Hall frame. All these patients experienced resolution of symptoms within 1 week to 2 months postoperatively.11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree