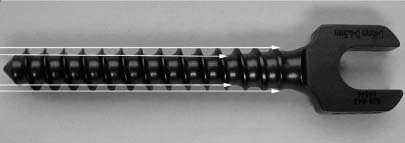
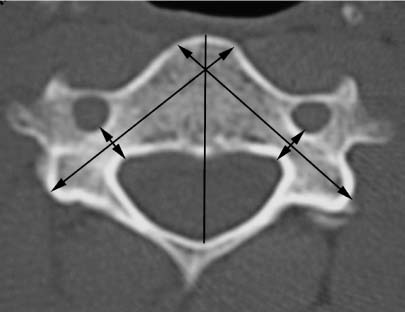
40 The goals of spinal fixation are to preserve existing neurologic function; to facilitate recovery of lost neurologic function; to correct deformity; to facilitate bone fusion; to preserve as many normal motion segments as possible; and to facilitate early mobilization, physiotherapy, or rehabilitation. Instability is usually associated with pain, deformity, and neurologic deficit. Segmental transpedicular fixation of the spine is a tremendously popular and relatively safe technique of ensuring rigid fixation of single or multiple motion segments. We believe that pedicle screw fixation is the “gold standard” of posterior instrumentation techniques. We feel that there are very few areas in spinal surgery where pedicle screw fixation does not out-perform other conventional means of posterior fixation, particularly in cases involving neoplasia. Pedicle screws can be placed in the spine from the cervical region caudally, all the way to the sacrum. However, because the relative anatomic relationships between the pedicles and the rest of the vertebrae change throughout the spine, working knowledge of this anatomy is essential for the safe and accurate placement of these screws. Even armed with this knowledge, current techniques remain poorly defined in certain areas of the spine, such as from C3 to C6. Other areas remain relatively safe, where the primary difficulty lies with soft tissue exposure, such as at the lumbosacral junction. Nonetheless, with a comprehensive understanding of pedicular anatomy, even the most difficult pedicles can be used to obtain a rigid fixation, allowing for a solid bone fusion. Pedicle screw fixation offers significant advantages for the treatment of spinal neoplastic disease. After posterior resection, this type of reconstruction reconstitutes a very effective tension band, preventing uncontrolled flexion and extension movements in the affected segments. Following anterior resection and reconstruction, posterior short segment fixation offers and ensures rigid stabilization, controlling motion in not only the sagittal, frontal, and axial planes but also with vertically oriented forces acting in compression and distraction. Fixation through both the posterior and middle columns makes this possible. Thus a well-planned pedicle screw construct can provide extremely rigid fixation to an unrestricted number of motion segments. In neoplastic conditions especially, pedicle screw fixation results in a race between eventual hardware failure versus bone fusion in some cases, or in others, patient death. The environment to achieve solid bony fusion is severely affected by several factors including radiation treatment, chemotherapy, and the use of steroids. But if fusion is successful, many patients with incurable disease can still go on to a reasonably long, high-quality life following radical surgical resection with good control of the neoplastic disease. Understanding of the biomechanical forces at work for a specific spinal disorder allows the surgeon to predict if the planned fixation construct will provide adequate stability over the short or long term. The specifics of the pathologic neoplastic process further determine the survival of the construct or the patient. Several biomechanical terms are important in gaining insight into the biomechanics of this type of fixation. Force is the product of acceleration and mass, measured in newtons (N). This concept is particularly important in testing the biomechanical properties of a spinal construct in the laboratory. Stiffness measures the ability of an implant to resist deformational change if a force is applied to it. Stiffness is the force per unit of deformity and can be linear (newton per millimeter) or angular (newton per degree). Flexibility and elasticity are the inverse of stiffness (1 ÷ stiffness) and represent a measurement of the tendency of a construct to deform. The ideal implant should have enough stiffness to maintain stability and to prevent progressive deformity and yet should be flexible enough to allow for bone fusion through load transfer across the fusion site (load sharing). This prevents bone resorption and enhances bone density. Constructs with too much elasticity allow excessive load transfer and motion, discouraging fusion and defeating the purpose of instrumentation. Constructs with too much stiffness may cause excessive stress shielding across the fusion site, leading to the bone resorption (according to the principles of Wolff’s law), stress fatigue, and eventual failure. The primary goal of spinal instrumentation is to provide sufficient temporary stabilization so that a bony fusion occurs. Without fusion all spinal constructs eventually fail. The pathologic process, bone quality, implant design, and technical aspects related to the stabilization construct interact to produce the outcome. In patients with neoplastic involvement, the race between bone fusion and instrumentation failure tends to be in favor of instrumentation failure. Load sharing and thus bony fusion is less of an issue in patients with neoplastic disease. The rigidity of the stabilization seems to be most important, considering in general a reduced life expectancy. The interface between the screw and the rod affects the rigidity of the construct. Pedicle screw fixation is considered rigid fixation compared with other designs. But pedicle screw constructs can also be grouped into rigid and less rigid constructs or constrained and unconstrained constructs. A constrained or rigid system does not allow for motion between the rod and the screw. A constrained system allows for less load sharing than an unconstrained system. The unconstrained or less rigid system allows for a small amount of motion between the screw and the rod as seen in the polyaxial screw head design. It favors load sharing and therefore, at least theoretically, bony fusion. Crosslinking of a pedicle screw construct has a significant effect on the stiffness of the construct in axial rotation but does not affect sagittal or frontal plane stiffness or stiffness under compression or distraction significantly.1,2 The magnitude of the increase in torsional stiffness correlates with the cross-sectional area of the crosslink. Two crosslinks are more effective in limiting rotation than a single crosslink.3,4 It is pertinent to review briefly some of the biomechanical considerations in screw design, as the pedicle screw is the fundamental component of any pedicle screw construct. The diameter, length, orientation, position, and linkages of the screws all contribute to the success of the construct. The major diameter of the screw is related to the pullout strength, and the minor diameter is important in determining bending strength and the ability to resist deformation or fracture. Bending strength varies as the third power of the minor diameter. Liu et al5 reported a 104% increase in static and fatigue strength as a result of a 27% increase in minor diameter. A small change in the depth of the screw thread can significantly affect the minor diameter and thus the bending strength (Fig 40-1). There are two basic screw designs: cylindrical and conical. The cylindrical design consists of an outer diameter (major diameter) that is constant along the length of the screw. The inner diameter (minor diameter) usually decreases toward the tip of the screw. Tapering the inner diameter in a cylindrical screw leads to a more aggressive thread at the tip while preserving the maximum diameter close to the screw head where shear forces across the screw are maximal (Fig 40-1). A conical screw design has tapered major and minor diameters. The conical design in theory should generate greater insertional torque (force needed to advance the screw) while maintaining purchase characteristics of the screw as it compacts cancellous bone within the pedicle. Kwok and colleagues6 compared insertional torque and pullout strengths of conical and cylindrical pedicle screws in human cadaveric vertebral bodies. They found that conical screw profile increased insertional torque but had little effect on straight axial pullout strength in cadaveric bone when compared with the cylindrical screw design. The pull-out strength of conical screws backed out 180 degrees is significantly less than a cylindrical screw backed out the same amount. FIGURE 40-1 A cylindrical-type screw. Various methods have been proposed for screw hole preparation, including drilling or curetting of the pedicle (funnel method), and probing with a curved flat probe or a conical straight probe. Moran et al7 found that drilled holes provided weaker fixation than probed holes. George et al8 found no statistical difference between drilled and probed holes. We feel that in theory it is counterproductive to remove cancellous bone from within the pedicle by drilling or curetting. We prefer to mark the entry hole with a small highspeed bur by just penetrating the proximal cortex, and we then use a smooth conical-tipped probe to probe the pedicle. This method, although not scientifically proven, compacts cancellous bone within the pedicle and should lead to an increased screw pullout strength. Screw pullout strength correlates with insertional torque. Zdeblick et al9 found that a linear relationship exists between the insertional torque and the number of cycles to ultimate pedicle screw pullout. Bone mineral density was a less effective predictor of failure. A smaller pedicle width correlated with increased insertional torque probably due to a better fit. Screw diameter significantly affects pullout strength. Willett et al10 have shown that increasing the major diameter of a screw by 20% from 5 to 6 mm increases the pullout strength by 47%. Orientation of the pedicle screw can significantly affect the pullout strength as well. Three different approaches have been described. In the “straight-ahead” method described by Roy-Camille et al,11,12 the screws are placed parallel with the superior end plate in the parasagittal plane. Magerl13 described the “inward” or anteromedial screw orientation where the screws are directed in line with the axis of the pedicle but parallel to the superior end plate. This results in the triangulation of the pedicle screws.13,14 Krag et al15,16 described a modification of the anteromedial technique and called it the “up and in” technique. The entry site is lateral as in the Magerl method but slightly lower in the pedicle, almost in the inferolateral quadrant. The screws are inclined medially in line with the axis of the pedicle but the screw is angled toward the anterior edge of the superior end plate. This technique improves screw pullout theoretically by increasing screw length and thus increasing screw-bone contact. The “toe-nailing” effect of nonparallel screws resists lateral shifting in the upper vertebra. In addition, placement of the screw head in an inferolateral position moves it away from the adjacent superior facet joint. Not surprisingly, bone mineral density is the single most important patient factor affecting pullout strength.17–19 The use of pedicle screws should be viewed with caution in severely osteoporotic patients. It is important to realize that the stability of fixation depends more on the strength of bone than on the qualities of the implant. Hadjipavlou and colleagues20 found a positive correlation between bone mineral density and pullout strength. They also found that triangulation is more important in osteoporotic vertebrae. In comparing axial pullout force in normal and osteoporotic human lumbar spines, Halvorson found that the method of hole preparation did not significantly affect the pullout strength in normal bone but that hole preparation had an effect on the screw pullout in osteoporotic bone; tapping with a small tap or placing a screw without tapping significantly improved screw pullout strength. Proximal cortex quality and integrity were also found to be important.21 In addition, augmenting the pedicle screw with two offset hooks at adjacent levels doubled the pullout strength in osteoporotic patients. Fusion rates, screw loosening, and screw breakage were found to be no different between two groups of patients with mean bone mineral densities of 72 mg/mL (osteoporotic) and 140 mg/mL (normal). Bone mineral density is more reliable than subjective radiographic grading of osteoporosis and for this reason might be included in preoperative evaluation of osteoporotic patients.18 Lu et al19 compared bone mineral density at different levels in the lumbosacral spine and in different areas of the vertebrae. Bone mineral density increased gradually from lumbar to the sacral vertebrae, possibly as a result of increased loading at the different levels. The highest bone mineral density was found at regions close to the pedicles and at the bases of the pedicles. McAfee et al22 found a linear correlation between decreasing volumetric density of bone and increasing rigidity of the spinal construct in an animal model. The screw-bone interface is critical in the use of spinal instrumentation. The insertion depth of the screw directly influences the screw-bone interface and therefore fixation. Screws placed at 50% depth of the vertebrae have 75% the strength of those screws placed at 80% depth.16 Screws placed at 100% vertebral body depth have 124 to 154% the strength of those placed at 80% vertebral body depth. An increase of 5 mm in screw length results in a 26% increase in fixation strength. The ideal screw, therefore, should be able to make the most of the available screw-bone interface. It should have the largest possible diameter and be long enough to reach the anterior cortex without perforation. However, in practice this is usually not possible. Although increasing the area of the screw-bone interface improves the strength of fixation, the risk of increasing the depth of screw placement must be balanced against the risk of damage to the anterior soft tissue structures.13,15 Repairing a stripped screw can be readily performed. However, it should be kept in mind that if polymethylmethacrylate (PMMA) is used, the risk of cement leakage from the pedicle or vertebral body must be acknowledged and minimized to prevent neurologic damage. Zindrick et al23 found that PMMA was able to restore secure screw fixation and that pressurized injection doubled the pullout force. Wittenberg et al24 studied the effect of bone cement augmentation on axial pullout strength and transverse bending stiffness of pedicle screws inserted into lumbar vertebrae. Their group found that both PMMA and a biodegradable composite (polypropylene glycol-fumarate) increased axial pullout force, whereas the PMMA also increased transverse bending stiffness. Moore’s group25 compared augmentation of pedicle screw fixation strength with PMMA to that of calcium phosphate cement. Calcium phosphate cement can be injected into a prepared screw hole but has the added advantage that it is reabsorbed and replaced during healing and normal bone remodeling. These investigators found that PMMA improved pullout strength by 147% and that calcium phosphate cement improved pullout strength by 102%. Vertebral bodies have two basic functional components: the anterior elements (vertebral body) and the posterior elements (laminae, facet joints, and the processes for attachment of muscles and ligaments—spinous processes and transverse processes). These two functional components are connected by the pedicles. The posterior elements provide areas for muscle attachments and the pars interarticularis lies at the junction of the horizontally located pedicle and vertically oriented laminae. Pedicles are engineering masterpieces. They are the only connection between the anterior weight-bearing elements and the posterior elements. All forces acting on the posterior elements are ultimately channeled to the anterior elements by the pedicles. The pedicles transmit both tension and bending forces. They are cylindrical in shape with thick cortical bone walls, enabling them to resist bending in any direction. The combination of tension and compression on opposite walls of a hollow cylindrical structure leads to almost no force in the center of the structure. Vertical and horizontal trabeculae pass through the pedicles into the different areas of the posterior elements. It is necessary to have a thorough knowledge of the position and specific anatomy of the pedicles in every area of the spine to perform a procedure involving spinal structures. Pedicles are considered to be the most important of anatomic spine landmarks. The medial pedicle wall forms the lateral extent of the canal and thus the lateral margin of the thecal sac. Pedicles also form the inferior and superior borders of the foraminal zone and hence directly indicate the location of nerve roots. Pedicle screw fixation in the cervical spine is a technically difficult procedure, due to important surrounding structures such as the vertebral arteries, spinal cord, and the exiting nerve roots. In addition, there is a significant variation in pedicle morphometry and orientation at a given level. This precludes the use of a standard entry point and directionally targeted techniques. In general, the height-to-width ratio of the pedicles decreases from C3 to C7. They are taller than they are wide at C3 and become more round toward C7. The mean height of the C3 pedicle is ~7.4 mm and the width is 4.8 mm, compared with a height of 7.1 mm and a width of 6.9 mm at C7.26 Medial angulations are highly variable, ranging from 27 to 59 degrees (mean 45 degrees). Panjabi et al27,28 found a gradual decrease in medial angulations of 40 degrees at C3 to 29 degrees at C7 (Fig 40-2). Jones et al26 found average medial angulations at C7 to be 45 degrees (Fig 40-3). An et al29 found average medical angulations of 37 degrees at C7, 32 degrees at T1, and 26.5 degrees at T2 (Fig 40-4).
Pedicle Screw Fixation of the Thoracic and Lumbar Spine
 Internal Fixation with Pedicle Screws
Internal Fixation with Pedicle Screws
 Pedicle Screw Biomechanics
Pedicle Screw Biomechanics
Screw Design
Screw Hole Preparation
Screw Pullout Strength
Bone Mineral Density
Screw Insertion Depth
The Stripped Screw
Pedicle Anatomy
Cervical Spine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




