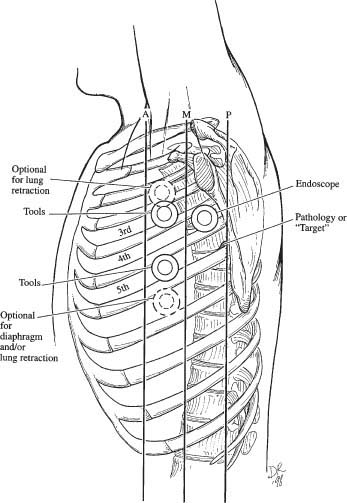
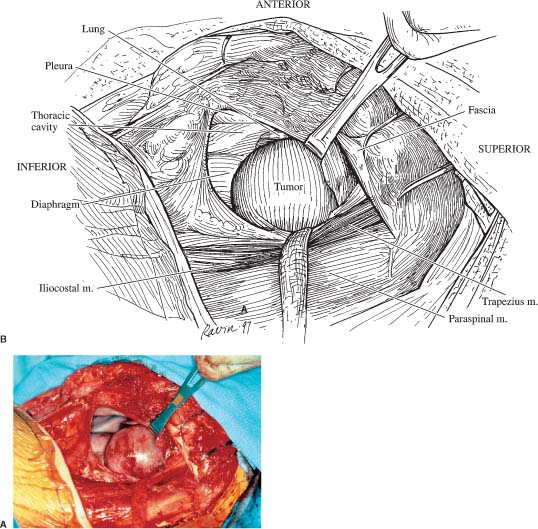
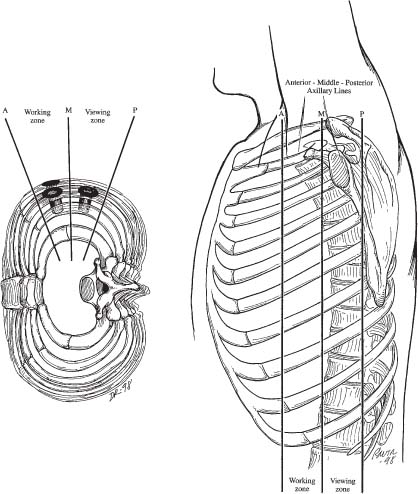
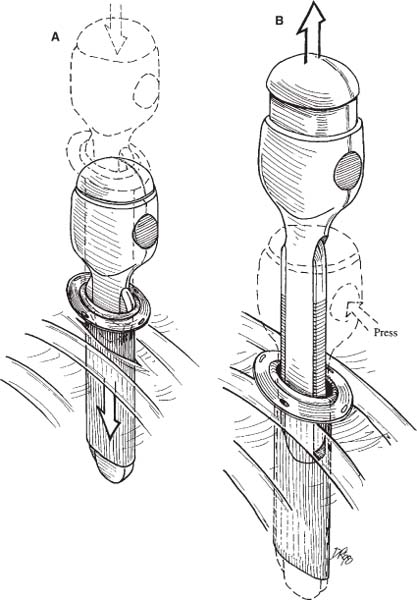
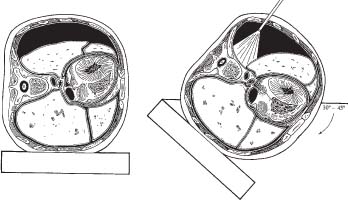
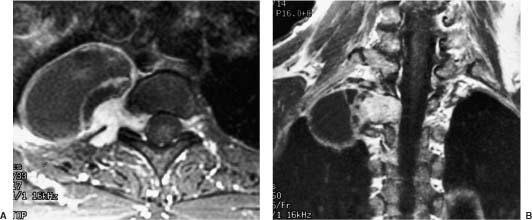
32 Transthoracic endoscopic surgery provides an excellent alternative for the resection of thoracic schwannomas, neurofibromas, or other benign neurogenic tumors with major components that extend into the thoracic cavity. The relatively simple surgical strategies and indications are reviewed in this chapter. The most ideal tumors for transthoracic endoscopic resection are benign paraspinal neurogenic tumors located peripherally within the intercostal nerves or those that extend from the neural foramina into the chest cavity. Before the advent of thoracoscopy, these tumors required a thoracotomy for removal (Fig. 32-1).1–3 Resection of paraspinal nerve sheath tumors may be indicated to prevent spinal cord compression from the tumors growing into the spinal canal, to relieve mass effect within the chest when a large tumor has impaired pulmonary function, to prevent malignant transformation of a tumor, or to provide a tissue diagnosis.1–9 In the thoracic spine, nerve sheath tumors with a significant component of their mass within the spinal canal compressing the spinal cord (i.e., classic dumbbell tumors) should not be approached endoscopically.3 These intradural tumors are approached posteriorly or posterolaterally using a laminectomy, transpedicular approach, or costotransversectomy. The dura is opened to allow resection of the intracanalicular tumor and decompression of the spinal cord, and the dura is closed in a watertight fashion. If the tumor also extends into the chest, a costotransversectomy approach can be used to resect small to moderate-sized extensions of the tumor (i.e., up to 4 cm); however, if a large component of a dumbbell tumor extends into the chest cavity, a thoracotomy or a thoracoscopic approach may be needed to allow adequate visualization and access so that the intrathoracic component of the tumor can be resected safely. The risk of a cerebrospinal fluid (CSF) leak can be minimized by resecting the foraminal and intradural tumor first and then by obtaining a watertight dural closure. Subsequently, thoracoscopy is performed to resect the residual tumor within the thorax. Initially, the patient is placed supine on the operating table while the anesthesiologist inserts a double-lumen endotracheal tube, an arterial line, and a central venous catheter. Proper positioning of the endotracheal tube is verified using a flexible fiberoptic bronchoscope. The patient is turned and placed in a lateral decubitus position on the operating table with the operative side up. A foam axillary roll is used to pad the dependent axillae. The dependent leg is flexed and the patient’s knees and bony prominences are padded with pillows and foam padding. The hips are securely taped to the operating table so that the table can be safely tilted anteriorly during surgery. Tilting is used intraoperatively to allow the atelectatic lung to fall away from the surface of the spine. FIGURE 32-1 Before the advent of thoracoscopy, a thoracotomy was required to resect a large intrathoracic schwannoma. Intraoperative photograph (A) and corresponding illustration (B) showing an 8-cm, solid tumor arising from the left T10 neural foramen and extending widely into the chest. A 12-inch thoracotomy incision was required for its exposure and resection. The incision extended posteriorly to expose the laminae and spinous processes so that the intradural component of this dumbbell tumor could be resected. The size of this incision contrasts strikingly to the small incisions used for thoracoscopy. The patient’s dependent arm is usually placed on a padded arm board; the upper arm is abducted and supported in an airplane splint. A C-arm is positioned to provide a clear anteroposterior view of the patient’s thoracic spine and thorax. Fluoroscopy is used to count the ribs to identify the levels of the patient’s pathology. When the level of pathology has been identified radiographically, the overlying skin is marked with indelible ink. The positions of the portals, scapula, and potential incisions are marked on the patient’s chest wall. The patient’s entire chest, axillae, proximal arm, back, and abdomen are sterilely scrubbed with a standard cleansing solution. Sterile towels and drapes are applied to maintain wide access to the chest. The surgeon and surgical assistant stand anterior to the patient, facing the patient’s anterior thorax. The anesthesiologist blocks the airflow to the side of access. The nonventilated lung becomes atelectatic, permitting access to the spine. FIGURE 32-2 Three portals are usually used for thoracoscopic paraspinal tumor removal. The portals are triangulated above and below the spinal target level. An additional portal may be needed in the working zone, rostral or caudal to the working portals, to insert a retractor for the lung or diaphragm. Thoracoscopic resection of paraspinal tumors usually requires three portals: one for the endoscope and two working portals for tools. Occasionally, a fourth portal may be required to insert a fan retractor if the lung or diaphragm needs to be retracted (Fig. 32-2). The portals should be spread far enough apart over the surface of the chest to allow the surgeon’s hands to have unrestricted movement. The portal for the endoscope is positioned between the middle and posterior axillary lines (viewing zone); the working portals for tools are inserted between the middle and anterior axillary lines (Fig. 32-3). A 10-mm diameter, 0-degree angle, rigid, high-resolution endoscope is used. Flexible portals (10 or 15 mm) are used to minimize postoperative intracostal neuralgia. Before a portal is inserted, the skin, muscle, and intercostal nerve at the sites are blocked with 1% marcaine with epinephrine. The anesthetic reduces the incidence of intercostal neuralgia at the portal sites. The epinephrine helps maintain hemostasis and prolongs the action of the marcaine. The portals are inserted using a technique that resembles chest tube insertion. The skin and subcutaneous tissues are incised (10- to 15-mm-long incision) parallel to the superior surface of the rib. A hemostat is passed through the intercostal muscles directly adjacent to the superior surface of the rib, thereby avoiding the neurovascular bundle on the caudal surface of the rib. The blunt tips of the hemostat penetrate through the parietal pleura into the thoracic cavity. The hemostat tips are opened and widely spread apart to dissect the intercostal muscles from the ribs to create a space for the trocar and portal. After the surgeon excludes the presence of focal pleural adhesions, the portals are inserted into the chest. The portals are secured to the chest wall with sutures or stables (Fig. 32-4). A wide variety of endoscopic tools are is for removing paraspinal tumors. The soft tissue dissection tools are used routinely for laparoscopic and thoracoscopic procedures. Special thoracoscopic spine tools (Kerrison’s, Cobb’s, etc.) and drills are also important for performing this surgery. Before performing any surgical procedures, the surgeon should become adept at using all thoracoscopic tools precisely. The nonventilated lung becomes densely atelectatic within a few minutes after its airflow is blocked. Pleural adhesions, if present, need to be detached to permit exposure of the tumor. After the lung is mobilized, it is retracted manually or with gravity by rotating the patient anteriorly (Fig. 32-5). Mechanical retraction of the lung should be performed cautiously using a fan retractor to avoid injury to the lung parenchyma. Mobilizing the lung permits direct visualization of the mediastinal structures, the surface of the spine, and the paraspinal tumor. Complete visualization and access to the tumor and adjacent vascular and visceral structures are provided. After the margins of the tumor have been exposed, the tumor is resected using the following steps. The pleura are incised over the tumor. The segmental vessels adjacent to the tumor and supplying the tumor are cauterized, ligated, and sectioned. The tumor is internally debulked using an ultrasonic aspirator, cautery loop, or sharp dissection. The margins of the tumor are mobilized, avoiding traction on the nerves of origin, protecting adjacent vascular and visceral structures. The remaining portions of the tumor are dissected sharply. FIGURE 32-3 The posterior axillary line is superficial to the thoracic vertebrae in a coronal plane over the spinal cord. The space between the middle and posterior axillary lines, the viewing zone, provides the best region to insert the endoscope for spinal thoracoscopy. The space between the anterior and middle axillary lines, the working zone, provides the best region to insert portals for tools to perform dissections of the spine. This configuration brings the surgeon’s hands anteriorly away from the endoscope, allowing more space to maneuver. After the tumor is removed, the surgical site is irrigated and hemostasis is completed. Chest tubes are inserted through two of the portal incisions. The lung is reinflated. The portal incisions are closed with deep and subcuticular resorbable sutures. The chest tubes are kept in place until their output diminishes to less than 100 cc per day. Thoracoscopic resection of intrathoracic schwannomas or neurofibromas begins by identifying and protecting the vascular and visceral structures adjacent to the tumor (Figs. 32-6 and 32-7). If the tumor has a cystic component, a long needle can be inserted into the tumor to decompress the lesion internally (Fig. 32-8). The pleura is incised, opened widely, and mobilized from the margins of the tumor (Figs. 32-9 and 32-10). The vascular supply to the tumor is coagulated with bipolar cauterization. If the tumor is located peripherally on the intercostal nerve and does not enter the neural foramen, the normal segments of the intercostal nerve are identified proximally and distally to the tumor using subperiosteal dissection to mobilize the neurovascular bundle from the rib. The tumor capsule is separated from the surrounding normal tissues using sharp and blunt dissection. The intercostal nerve is sectioned proximally and distally, leaving stumps of normal nerve tissue attached to the tumor that can be used as handles to grasp and manipulate the tumor as it is mobilized circumferentially. The tumor may be resected en bloc as a single specimen; however, to remove a large tumor from the thorax through an endoscopic portal, the tumor may need to be sectioned into pieces or placed within an endoscopic specimen bag (Fig. 32-11). FIGURE 32-4 (A) The flexible portal and trocar are inserted into the incision in the intercostal space. (B) The trocar is removed, leaving the portal in place. The portals are sutured or stapled to the skin to anchor them into position. FIGURE 32-5 Rotating the patient anteriorly 30 to 45 degrees allows gravity to retract the atelectatic lung. This technique reduces or eliminates the need for mechanical lung retraction. The patient’s body should be taped securely to the operating table with wide cloth tape to permit the table to be rotated this extensively. Nerve sheath tumors that extend into the neural foramen are approached using a strategy that avoids extensive manipulation of the tumor, traction on the foraminal component of the tumor, and avulsion of the proximal thoracic nerve root that could cause leakage of cerebrospinal fluid (CSF) or spinal cord injury. The intrathoracic tumor is first detached from the distal segment of the intercostal nerve (Fig. 32-12). The distal tumor is mobilized from normal tissues with sharp and blunt dissection, avoiding traction on the proximal tumor mass within the neural foramen. Once sufficiently mobilized and detached from normal tissues, the tumor is sectioned to detach its main portion from the portion entering the neural foramen (Fig. 32-12). The bulk of the tumor mass can then be removed piecemeal.
Thoracoscopic Resection of Intrathoracic Paraspinal Neurogenic Tumors
 Operative Indications
Operative Indications
 Operative Techniques
Operative Techniques
Patient Positioning
Portal Placement
Thoracoscopic Tools
Exposure of the Tumor and Spine
 Specific Strategies for Thoracoscopic Removal of Paraspinal Tumors
Specific Strategies for Thoracoscopic Removal of Paraspinal Tumors
Extradural Tumors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree