Chapter 32 Percutaneous Lumbar Restabilization via a Posterolateral Approach
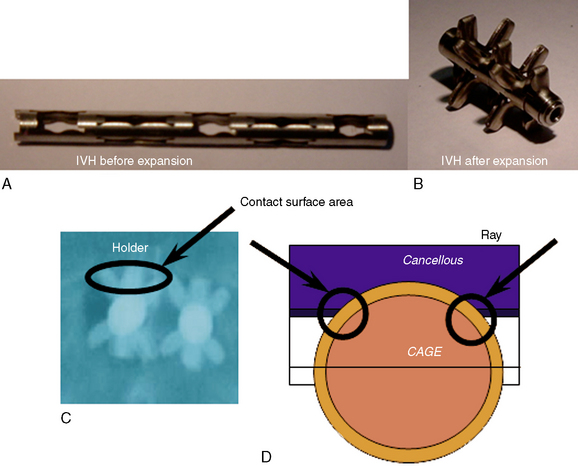
Minimally invasive percutaneous lumbar restabilization via a posterolateral approach is a valid and less aggressive procedure than conventional open surgery for the treatment of lumbar segmental insufficiency (LSI) or micro-instability. The potential for performing a percutaneous lumbar restabilization has been made possible by the development of a new expandable titanium device available in several sizes (B-Twin System [Disc-O-Tech Medical Technologies Ltd., Herzliya, Israel] or intervertebral holder [IVH]), which should serve as the first device of its nature in a series of new-generation implants conceived for the less invasive treatment of a number of spine conditions [1–5].
The advantages of this surgical option include the following:
 The procedure is performed with use of local anesthesia and minimal sedation if necessary (with an anesthesiologist standing by).
The procedure is performed with use of local anesthesia and minimal sedation if necessary (with an anesthesiologist standing by). It does not exclude the use of other percutaneous restabilization techniques, and if necessary, more standard procedures can be carried out in a second step or stage.
It does not exclude the use of other percutaneous restabilization techniques, and if necessary, more standard procedures can be carried out in a second step or stage. It allows for quick mobilization and recovery and, therefore, prompt physiotherapeutic adjuvant treatment and a faster return to normal daily life.
It allows for quick mobilization and recovery and, therefore, prompt physiotherapeutic adjuvant treatment and a faster return to normal daily life.The primary indication for percutaneous lumbar restabilization with the expandable interbody device is the treatment of lumbar segmental instability at the lower lumbar level (Fig. 32-1). This clinical feature is characterized by typical signs and symptoms associated with clear radiologic criteria (Table 32.1).
Table 32.1 Clinical and Radiologic Features of Lumbar Segmental Insufficiency (LSI)
| Clinical Features | |
|---|---|
| Clinical anamnesis | |
| Clinical characteristics | Single- or multiple-segment pain at the level of the interspinous ligaments and/or facet joints produced in hyperextension and/or rotation |
| Pathognomonic Radiologic Signs’ | |
|---|---|
| Conventional radiography | |
| Functional x-ray study | Dynamic sagittal instability (flexion-extension > 6 mm) |
| Magnetic resonance imaging: the stage or degree of LSI and with regard to the Modic changes described below | Local kyphosis and/or posterior articular subluxation on both T1-weighted and T2-weighted sequences |
| Modic changes | Type I: Disruption and fissuring at the level of the end plates with low signal on T1-weighted images and increased signal on T2-weighted images |
| Type II: Fatty conversion with increased signal on T1-weighted images and isointense or increased signal on T2-weighted images | |
| Type III: Marked sclerosis (osteochondrosis) with low or no signal on both T1- and T2-weighted images | |
’ To confirm the diagnosis of LSI, the patient must exhibit at least three of the radiologic signs or criteria listed in this table in addition to the standard clinical signs and corresponding anamnesis.
Indications and Contraindications
See Table 32.1 for the indications for percutaneous lumbar restabilization via a posterolateral approach. Box 32.1 lists the contraindications. Degree of disc removal remains a matter of debate because the surgeon is limited as to the degree of motion (in-and-out movements and technical limitation to go laterally in the working channel). Eroders cannot be used for the percutaneous application of the device. They are used strictly in the microsurgical reduced open application. The curette and possibly a shaver must be used in the percutaneous technique.
Patient Selection
For a proper patient selection, the clinical criteria for low back pain and hyperalgic blocks should prevail over the presence of associated leg pain, and the suspected diagnosis must be confirmed by the imaging data (Box 32.2).
BOX 32.2 Required Diagnostic Screening for Suspected Diagnosis of Lumbar Segmental Insufficiency
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree