7 Physical Examination I. Key Points – There are four main components to the spinal exam: motor, sensory, reflex, and mechanical. This is in addition to the general exam, which includes observation for cutaneous and nail changes, deformity, pain behaviors, and other signs. – Although components of a general survey nature should always be included, the physical exam is tailored to specific situations based on the history, the region of suspected involvement, and abnormal findings during the survey exam. – No protocol can cover every contingency, and the exam must be individualized based on patient-specific factors. The order of the exam procedures must also be tailored to the situation. II. Main Components of the Spinal-Related Exam – Motor (strength, coordination, spasticity, muscle bulk/tone including atrophy/fasciculations) • Strength evaluation is usually graded using the Royal Medical Research Council of Great Britain (MRC) scale, shown in Table 7.1. – Sensation (pinprick, light touch, proprioception, temperature) • Pinprick testing. Dermatomes and sensory distributions of peripheral nerves are shown in Fig. 7.1. • Proprioception (posterior column function) is assessed by testing joint position sense in the second toe on each foot, and/or vibratory sense with a low-frequency (128 Hz) tuning fork applied to bony prominences in the ankles. • Temperature sense may be crudely assessed by pressing the cool metal of a reflex hammer handle to the skin. Table 7.1 Muscle Grading (Modified Medical Research Council System)
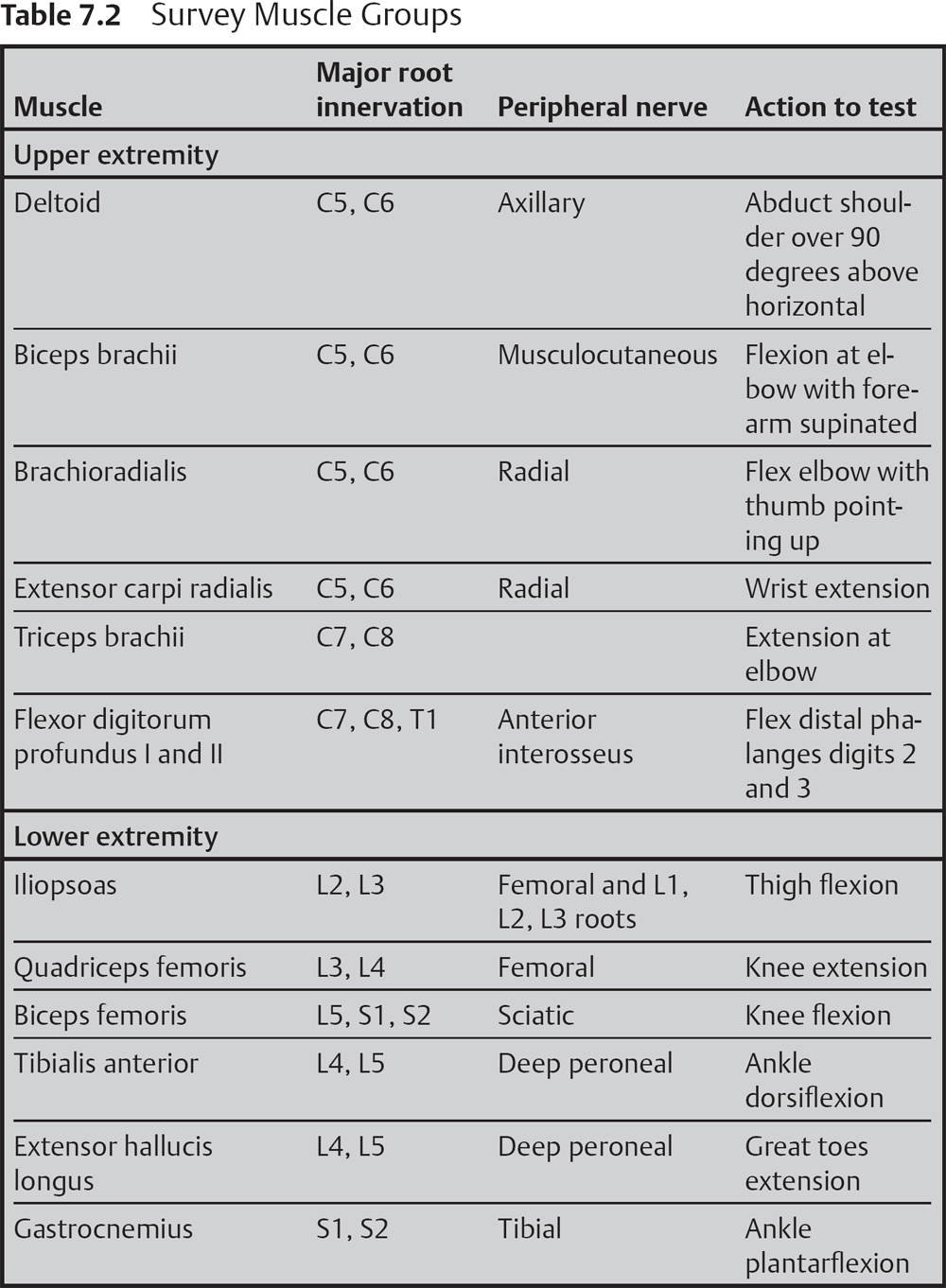
 An overview of survey muscle groups to examine is shown in Table 7.2.
An overview of survey muscle groups to examine is shown in Table 7.2.
 Further motor testing, as indicated, may include the tibialis posterior and gluteus medius (in cases of foot drop to distinguish radiculopathy from peripheral neuropathy), first lumbrical (median nerve), and abductor digiti minimi (ulnar nerve).
Further motor testing, as indicated, may include the tibialis posterior and gluteus medius (in cases of foot drop to distinguish radiculopathy from peripheral neuropathy), first lumbrical (median nerve), and abductor digiti minimi (ulnar nerve).
| Grade | Strength |
| 0 | No contraction (total paralysis) |
| 1 | Flicker or trace contraction (palpable or visible) |
| 2 | Active movement through full ROM against gravity |
| 3 | Active movement against resistance |
| 4 | Active movement against resistance (subdivisions: 4–, slight resistance; 4, moderate resistance; 4+, strong resistance) |
| 5 | Normal strength (against full resistance) |
| NT | Not testable |
Abbreviation: ROM, range of motion.
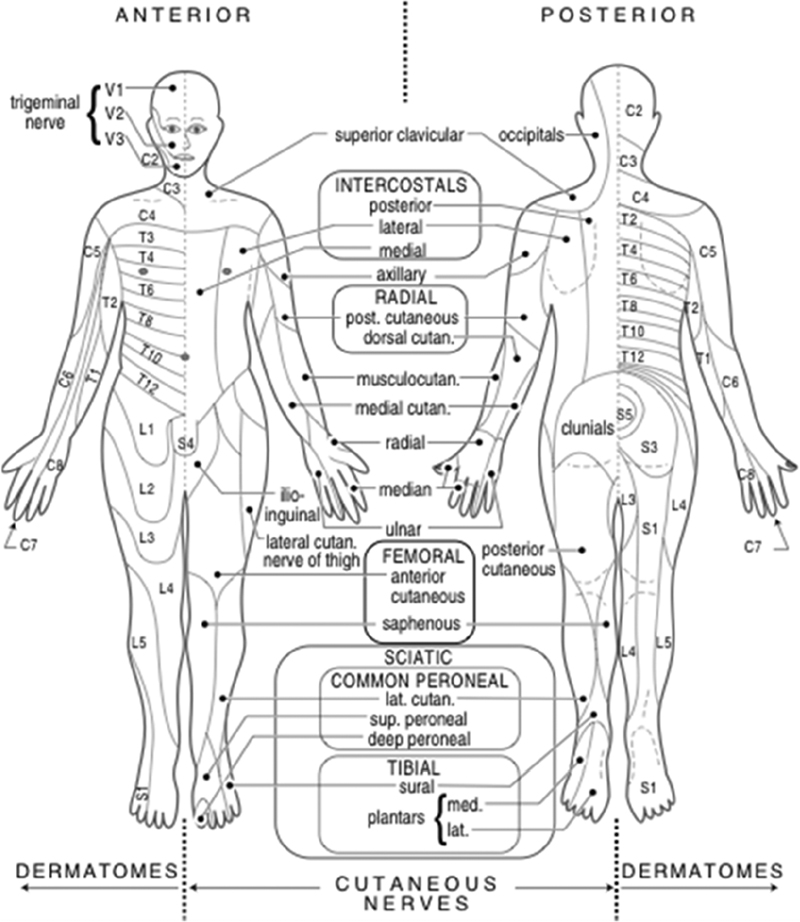
Fig. 7.1 Dermatomes and sensory distributions of peripheral nerves.
– Reflexes (muscle stretch reflexes, pathologic reflexes, cutaneous reflexes, sacral reflexes, and priapism)
• Muscle stretch reflexes are usually graded as shown in Table 7.3. The muscle stretch reflex involved is shown in Table 7.4.
• Babinski sign, Hoffmann sign, and testing for ankle clonus. Assessment for long tract signs should be made in all patients to disclose unsuspected cervical or thoracic myelopathy or other causes of upper motor neuron deficit.
Table 7.3 Muscle Stretch Reflex (Deep Tendon Reflex) Grading Scale
| Grade | Definition |
| 0 | No contraction (total paralysis) |
| 0.5 | Elicitable only with reinforcement* |
| 1+ | Low normal |
| 2+ | Normal |
| 3+ | More brisk than normal (hyperreflexic) |
| 4+ | Hyperreflexic with clonus |
| 5+ | Sustained clonus |
*In the lower extremities, reinforcement consists of having the patient hook the tips of the fingers of the left hand into the tips of the hooked fingers of the right hand and pulling (Jendrassik maneuver). Reinforcement in the upper extremities consists of having the patient clench the teeth.
• Further reflex testing, as indicated, includes abdominal cutaneous reflexes, anal wink, and bulbocavernosus.
• Priapism may indicate spinal cord injury.
– Mechanical factors (including observation for cutaneous changes, pain behaviors, muscle bulk/tone, and provocative maneuvers)
• Gait and station. Casual gait is assessed in all patients to check balance, weakness that compromises gait, and pain manifestations. Tandem gait and/or the Romberg test can further assess balance and posterior-column (proprioceptive) function.
• Cervical spine
 Cervical range of motion and specific levels of tenderness should be documented to distinguish myofascial from bone-related factors. Specific facet pain diagram patterns can be reviewed with the patient to identify problem levels.
Cervical range of motion and specific levels of tenderness should be documented to distinguish myofascial from bone-related factors. Specific facet pain diagram patterns can be reviewed with the patient to identify problem levels.
 The Spurling maneuver (axial loading on the vertex of the head with rotation to one side, repeated with rotation to the other side) may reproduce cervical nerve root symptoms in a patient with herniated cervical disc or foraminal stenosis.
The Spurling maneuver (axial loading on the vertex of the head with rotation to one side, repeated with rotation to the other side) may reproduce cervical nerve root symptoms in a patient with herniated cervical disc or foraminal stenosis.
 Shoulder pathology can often mimic cervical spine pathology. Tenderness of the acromioclavicular joint to palpation or a positive empty-can test suggests primary shoulder pathology as a cause of shoulder pain.
Shoulder pathology can often mimic cervical spine pathology. Tenderness of the acromioclavicular joint to palpation or a positive empty-can test suggests primary shoulder pathology as a cause of shoulder pain.
• Lumbar spine
 Lumbar range of motion and specific levels of tenderness should be documented to distinguish myofascial from bone problems.
Lumbar range of motion and specific levels of tenderness should be documented to distinguish myofascial from bone problems.
 Nerve root tension signs. “Pull” on the nerve root, which can reproduce pain in situations where the nerve root is compressed.
Nerve root tension signs. “Pull” on the nerve root, which can reproduce pain in situations where the nerve root is compressed.
Table 7.4 Muscle Stretch Reflexes
| Nerve root involved | Corresponding muscle stretch reflex |
| C5 | Deltoid and pectoralis* |
| C6 | Biceps and brachioradialis |
| C7 | Triceps |
| C8 | Finger flexor* |
| L4 | Patellar (knee jerk) |
| L5 | Medial hamstrings* |
| S1 | Achilles (ankle jerk) |
*A reflex that is not widely used and may be difficult to elicit.
 Laségue sign or straight-leg raising (SLR). Supine patient raises one lower extremity (LE) at a time. Classically positive findings include pain or paresthesias in the distribution of the involved nerve root (not just back pain) at less than 60 degrees elevation. In response the patient may lift the hip on the involved side off the exam table. This procedure helps to differentiate radiculopathy from hip pathology (e.g., trochanteric bursitis). Positive in 83% of cases with nerve root compression, it is more sensitive for compression in L5 or S1 than in upper lumbar roots.
Laségue sign or straight-leg raising (SLR). Supine patient raises one lower extremity (LE) at a time. Classically positive findings include pain or paresthesias in the distribution of the involved nerve root (not just back pain) at less than 60 degrees elevation. In response the patient may lift the hip on the involved side off the exam table. This procedure helps to differentiate radiculopathy from hip pathology (e.g., trochanteric bursitis). Positive in 83% of cases with nerve root compression, it is more sensitive for compression in L5 or S1 than in upper lumbar roots.
 Femoral stretch test or reverse straight-leg raising. With patient prone, the knee is flexed on one side at a time. This test is more likely to be positive than SLR with upper lumbar nerve root compression (L2, L3, or L4).
Femoral stretch test or reverse straight-leg raising. With patient prone, the knee is flexed on one side at a time. This test is more likely to be positive than SLR with upper lumbar nerve root compression (L2, L3, or L4).
• Hip and sacral pain. It is important to distinguish hip-mediated pathology and low back pathology.
 Palpation over spinous processes, paraspinal muscles, greater trochanters (to assess for greater trochanteric bursitis), and SI joints (Fortin finger test) may suggest sacroiliitis.
Palpation over spinous processes, paraspinal muscles, greater trochanters (to assess for greater trochanteric bursitis), and SI joints (Fortin finger test) may suggest sacroiliitis.
 FABER (acronym for flexion, abduction, external rotation, also called the Patrick test) test of the hip with the patient supine: back pain suggests musculoskeletal lower back or sacroiliac pain; groin or hip pain suggests hip pathology.
FABER (acronym for flexion, abduction, external rotation, also called the Patrick test) test of the hip with the patient supine: back pain suggests musculoskeletal lower back or sacroiliac pain; groin or hip pain suggests hip pathology.
 Shear test can help distinguish sacral pain. Patient prone, the examiner applies pressure to the sacrum while applying a traction force caudad with the corresponding limb. A test is positive if it reproduces the patient’s typical pain.
Shear test can help distinguish sacral pain. Patient prone, the examiner applies pressure to the sacrum while applying a traction force caudad with the corresponding limb. A test is positive if it reproduces the patient’s typical pain.
 FADIR (acronym for flexion, adduction, internal rotation) test of the hip with the patient supine can help to distinguish piriformis syndrome. Positive reponse: pain reproduction centered at half the distance between the S3 foramen and the ipsilateral greater trochanter.
FADIR (acronym for flexion, adduction, internal rotation) test of the hip with the patient supine can help to distinguish piriformis syndrome. Positive reponse: pain reproduction centered at half the distance between the S3 foramen and the ipsilateral greater trochanter.
• Vascular considerations: Palpation for pedal pulses to rule out vascular insufficiency.
III. Clinical Pearls
– Babinski sign or a positive Hoffmann sign: if there is no known etiology in a given patient, further investigation is required (to rule out cord compression or brain involvement).
– Cervical radiculopathy does not cause pain with shoulder abduction.
– Painless weakness in the LE is almost never due to lumbar nerve root compression. Consider diabetic neuropathy, cervical spondylotic myelopathy, or motor neuron disease, for example.
Common Clinical Questions
1. A 55-year-old male presents to your clinic with progressive lower extremity weakness and difficulty ambulating. He brings with him an MRI that shows grade 1 spondylolisthesis L5-S1 with severe central canal stenosis. Flexion/extension lumbar spine x-rays show no instability. His exam shows diffuse weakness of the LEs, diffuse reduction of pinprick sensation in the LEs, reduced Achilles reflexes, and bilateral upgoing toes. Actions that could be taken include:
1. Decompressive laminectomy L5-S1 with attempt at reduction with bilateral pedicle screw/rod instrumentation.
2. Lateral interbody fusion L5-S1 with lateral vertebral body plating.
3. Anterior lumbar interbody fusion with percutaneous L5-S1 pedicle screw/rod instrumentation.
4. MRI of the thoracic and cervical spine.
The appropriate options to take at this time are:
A. 1 and 3
B. 2 and 3
C. 1, 2, and 3
2. A patient presents with a 2-month history of left UE pain radiating to the thumb and index finger that has not responded to conservative therapy. He has a positive Spurling sign with the head turned to the left. Strength is normal. Reflexes are normal except for a reduction in the left biceps. An MRI of the cervical spine shows disc degeneration with protrusion into the left neural foramen at both C5-6 and C6-7. Flexion/extension cervical spine x-rays are without instability. After providing informed consent, he indicates he wishes to proceed with surgical treatment. Appropriate surgical options include the following except:
A. ACDF C5-6
B. ACDF C5-6 and C6-7
C. ACDF C6-7
D. Cervical disc arthroplasty C5-6
3. A 60-year-old male has diffuse weakness of the UEs with reduced reflexes, and hyperreflexia in the LEs with bilateral upgoing toes. Etiologies that could be considered include:
1. Cervical spine stenosis.
2. Left C5-6 foraminal herniated cervical disc.
3. Motor neuron disease (amyotrophic lateral sclerosis).
4. Coincident severe lumbar and cervical spinal stenosis.
From the above list, appropriate diagnoses for this patient are:
A. 1 and 3
B. 2 and 4
C. 1, 2, and 3
D. 4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







