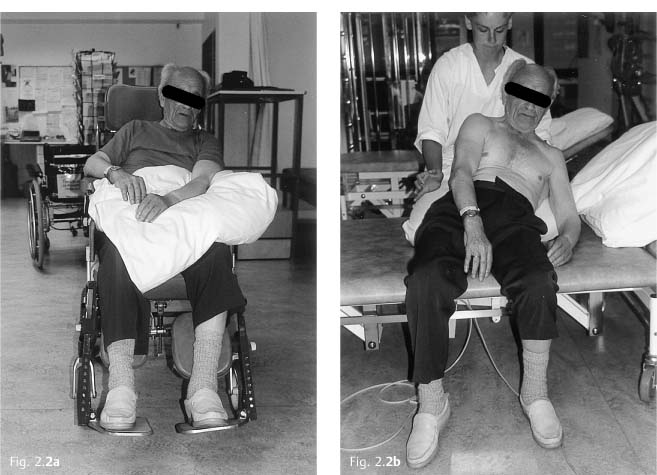
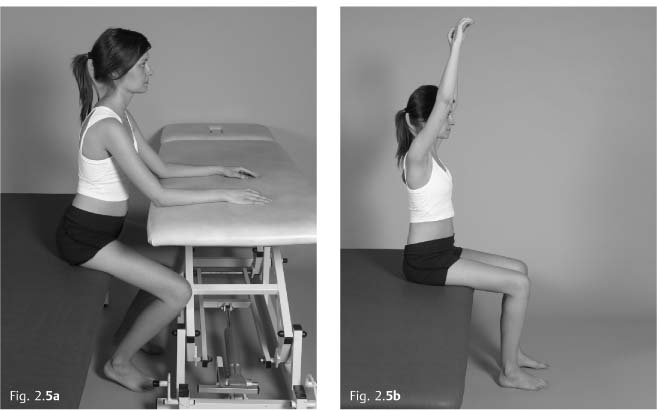
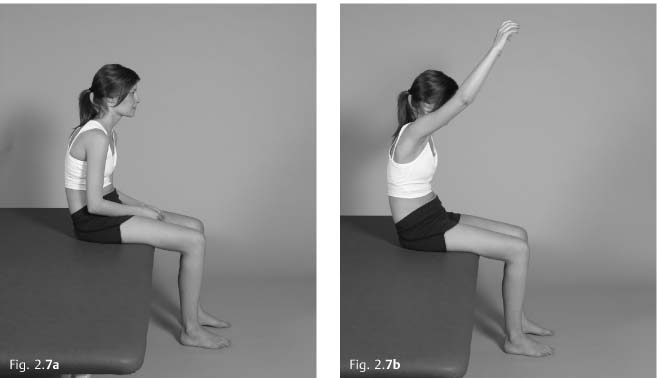
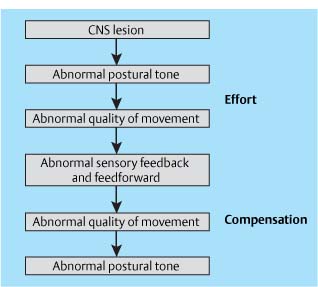
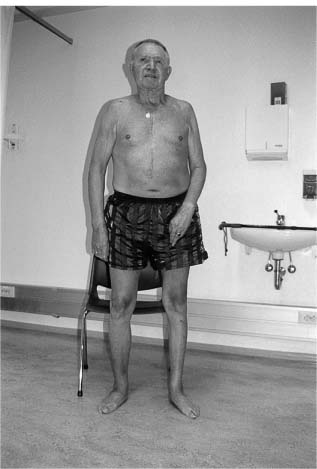
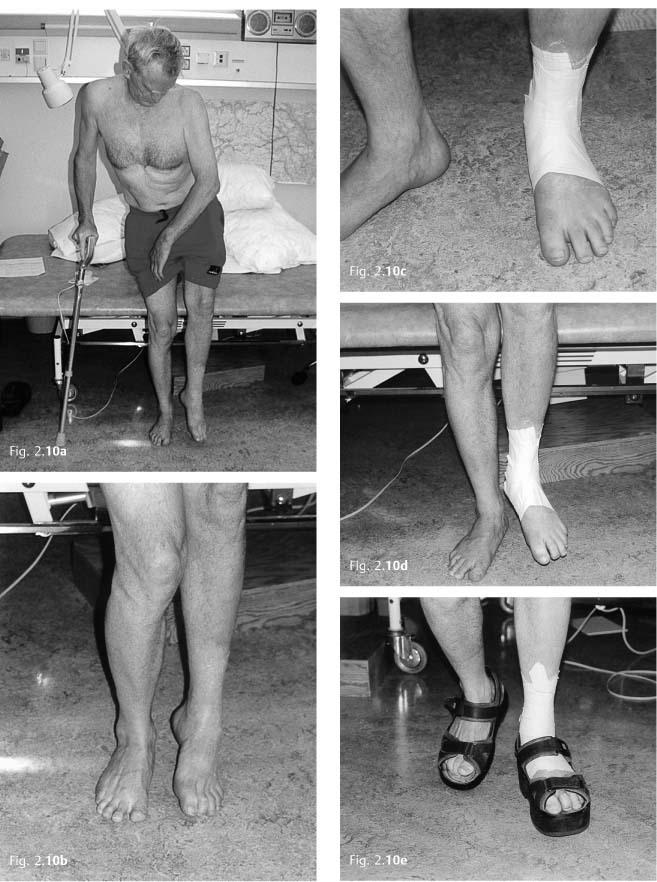
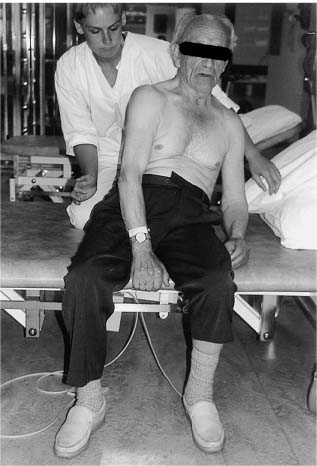
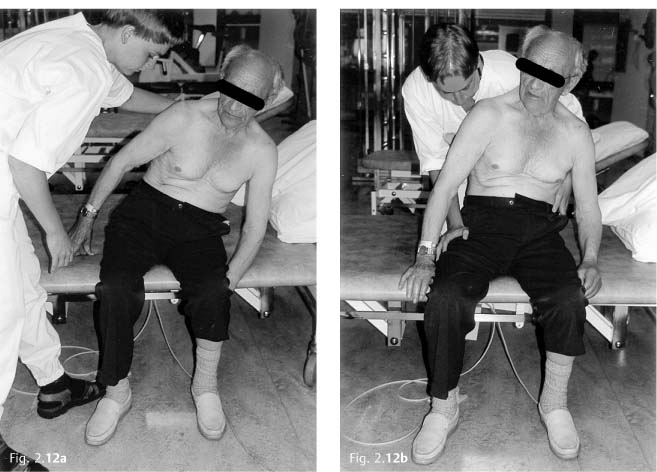
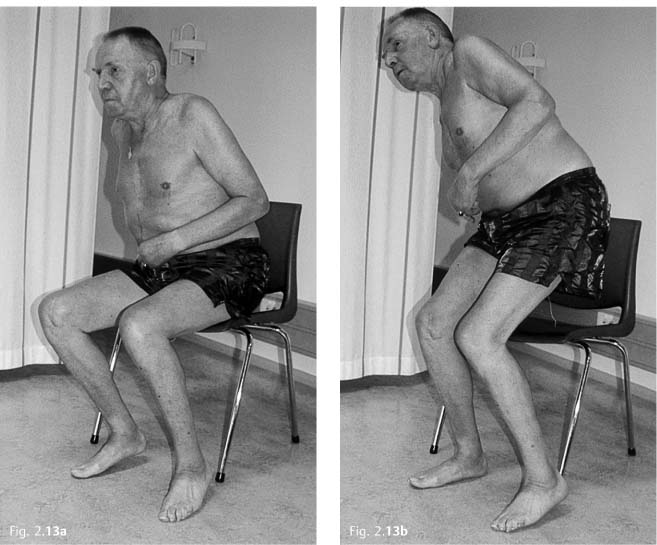
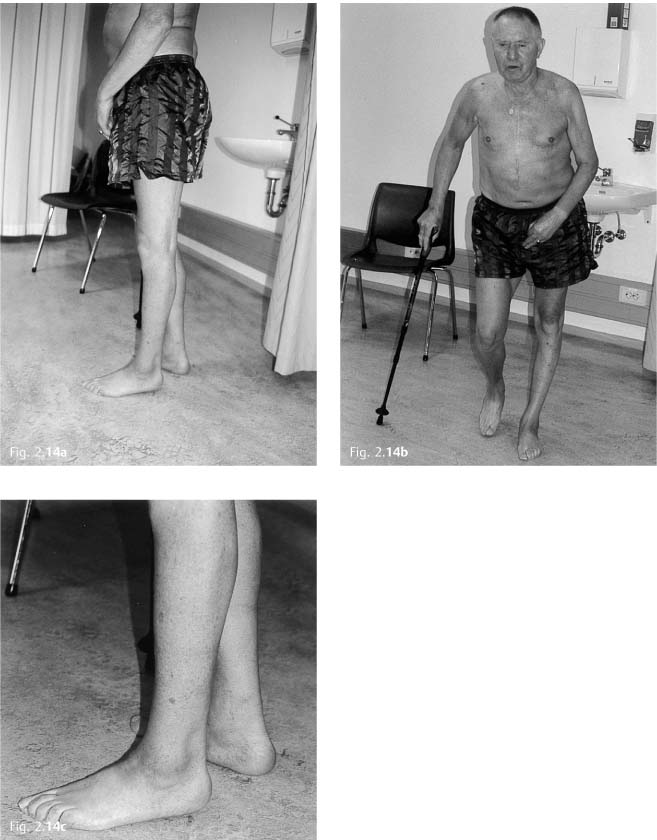
2 Physiotherapy 2.2 Intervention—Considerations and Choices 2.3 Other Interventions: Some Key Points Normal movement is complex. Many books have been written on the subject, and more recently there has been a lot of research in different branches of movement science. Movement science is the study of movement from different perspectives: for instance physiotherapy, psychology, pedagogy, physics, neurophysiology, biomechanics, and biologists studying human movement. It provides the basic knowledge of movement important for all therapists. Most research on movement, however, is still in its early days in that most of it is conducted in research laboratories with healthy, younger people, and therefore not always directly applicable to patients in a clinical setting. There is no international consensus on how this research could—or should—be applied clinically, and no consensus on intervention. In this book, I aim to present physiotherapy from my own experience, knowledge base, and point of view, and as an advanced course instructor of the International Bobath Instructors Training Associaiton (IBITA). The word concept means “something understood, an idea” (Taber’s Cyclopedic Medical Dictionary 1997) or it is “an element used in the development of a theory” (MillerKeane Encyclopedia and Dictionary of Medicine, Nursing and Allied Health 1992). Here, concept is applied to the knowledge base that clinical reasoning is based on. A conceptual understanding is therefore not learning a method, but learning to analyze and understand connections in an individual’s movement problems—Why do they move in this way? The aim of this chapter is to establish an understanding of balance and movement, and to highlight some of the reasoning and choices therapists make in the treatment of individuals with central nervous system (CNS) lesions. We now know that the CNS undergoes changes depending on what input it receives and the response to this input. There is a constant interaction between the individual and his environment that shapes the body and brain—plasticity is the bridge between brain and behavior. As a consequence, human movement is adaptable and humans have a capacity for learning, both with a healthy CNS and after CNS lesions. Therapists form an important part of the patient’s environment and training; treatment induces changes in cortical activation patterns over time (Nelles 2004). Therefore, theoretically, health professionals should be able to help the patient shape and adapt, to learn what seems appropriate and “unlearn” what seems inappropriate (associated reactions, inappropriate and inefficient motor strategies). Our aim should be to help the patient to develop and optimize their potential. But “We are currently being forced into interventions to ‘get the patient out’ that are supposedly cost effective. However, are we training compensatory strategies that will prevent true recovery, thus lengthening the time and increasing the level of care that the person will need in the long run?” (Held 1987, p. 174). This statement seems as true today as when it was written 20 years ago. Health professionals face this dilemma; often we know what is possible but rarely have the resources to see it through. We may limit the patient’s potential; perhaps we lack optimism and vision and do not believe that the patient can improve? The goals are set at a level we can reach based on our resources (time, economy, competence) and beliefs, not necessarily at the patient’s real potential for regaining function based on the localization and extent of the lesion, the patient’s premorbid status, his general condition, and his plastic ability—his capacity to learn. “First of all, we as therapists need to change our operating assumptions. We should expect recovery and work for that by preventing rather than encouraging compensation to occur. We should carefully analyse each person’s problems, and we must intervene early” (Held 1987, p.173). In rehabilitation, goals are often related to the following. The patient should, as much as possible be able to: • Participate in his life, fulfil his roles • Master activities – daily functions – function in his own environment • Control balance, movement, and function: – improve postural control and selective movement – regain the ability to interact with the environment – control the recruitment of tone. Learning through early and gradual interaction with gravity with good alignment to optimize muscle activation and with support or facilitation where and when it is needed – develop appropriate strategies and patterns of movement – develop appropriate strength to interact with gravity – maintain muscle length and range of movement Physiotherapy-related goals are set by the patient and therapist together. The patient’s needs and goals and therapy goals must be in harmony. The therapist’s challenge is to increase the patient’s competency, insight, and understanding for a process leading to greater participation and independence, and this takes time. Treatment for many patients will first and foremost be aimed at improving selective postural control and balance in functional situations to strengthen carry-over to daily activities in the patient’s own environment. If the patient’s postural control is regained to a level where he is able to take more part in his environment, be more oriented toward and integrated with the world around him, he will, in my understanding, have greater opportunities of participating in a variety of social settings. People are different: interests, wishes, goals, needs, previous experiences, what we like, who we like … To be able to create a constructive patient–therapist relationship, the therapist has to adapt to many different individuals and meet each one with a positive attitude, empathy, professionalism, and respect for the person’s integrity. It is important to create a good learning environment to motivate and inspire the patient, and at the same time give realistic information without taking hope away. Evidence supports the theory that the patient should be exposed to an enriched environment to develop his potential for learning (Virji-Babul 1991). Motivation and focused attention are important factors for learning (see Plasticity). Assessment and treatment build on: • Analysis of “normal” movement • Analysis of deviations from “normal” movement • Clinical reasoning • Appropriate treatment techniques to facilitate the patient’s regaining of motor control The following sections will focus on: • Balance and movement • Conceptual understanding for treatment rationale and choice of individually adapted treatment techniques • Other forms of treatment/interventions When we study humans in movement we are able to recognize whether they are sitting, standing or walking, standing up or sitting down, or turning around “normally,” because we all perform these activities in a basically similar way. We recognize when people have good balance, and observing their movement strategies enables us to recognize common features in the average population, which define our genotype. There are many common aspects to how individuals problem-solve a movement task: • Appropriate sequence of recruitment and tension development of muscles • Necessary range of movement in different single joints • Necessary ranges of movement between the extremities and the torso • Appropriate development of torque • Appropriate alignment, which is essential for the sequencing and selective activation of muscles • Appropriate effort—no more than needed for efficiency and successful goal achievement • Rhythm, tempo, variation Basic components of movement that are coordinated in time and space have to be activated for us to interact with gravity and use our arms functionally at the same time. Our daily activities demand both postural and movement control. Which components are most important depends on the person, the goal, the environment, and the actual situation. Each individual has his own, personal way of moving, the individual expression—the phenotype. We recognize a person by the way he moves. It may be enough to hear the steps in the hall: rhythm, step, tempo, firmness, light, hard or shuffling steps—all characteristics of the individual. The movement expressions may even reflect the person’s state of mind: the extended self-assured type or the flexed, modest insecure or anxious person are two extremes. Normal movement is varied, without inappropriate effort, efficient, effective, precise, and successful, developed through the interaction between the person, the task, and the environment. The expression normal movement reflects both the common features of humankind and the individual expression. A person’s build and posture inform the therapist of his movement experience and how he has used his body before. Through analysis of movement, the individual expression is evaluated, as well as how movement is performed in relation to the goal activity, the environment, and the ability to vary during different activities in different situations. Analysis of movement involves both observation and handling (hands-on) during activity, with special focus on: • Balance • Postural control – postural activity, build, and posture—postural tone – the relationship to gravity and to the environment, the base of support – coordination, reciprocal innervation – the relationship between body segments and their function (stability-movement) • Coordination of the individual components in sequence, time, and space, i. e., the recruitment of movement patterns • The selective movement of single components Balance is the result of the interaction between motor, sensory, and cognitive processes. Many routine activities, for instance balance, walking, reaching for something, or dressing demand none or very little effort or cognitive awareness. Balance is the foundation for our daily activities. It allows us to be stable and active in relation to gravity and the base of support whilst at the same time using our arms—which are free—for functional activities. Balance is movement as well as a prerequisite for movement. Through movement we interact with the environment and learn to perceive ourselves in relation to the world around us. Balance is a holistic sensorimotor and perceptual interplay between our surroundings and us, and requires graded and coordinated neuromuscular activity of the whole body at the same time. Balance may be expressed as a reaction when displacement occurs suddenly and unexpectedly, or a strategy when we right ourselves, transfer weight, turn around, or step. Strategy refers to cognitive processing because it involves the organization and sequential planning of a goal-directed movement. Strategy should imply the existence of choice. That is, the goal should be attainable via different ways (Windhurst et al. cited in Massion 1992). • Strategy involves a level of processing, problem solving, and planning (feedforward). • Reaction defines the response of an organism, or part of it, to a stimulus (Taber’s Cyclopedic Medical Dictionary 1997). Reactions are the result of external influences (feedback). • Balance contains both these elements: It is a reaction to displacement at the same time that movement is planned in relation to the task and the environment. Examples Many studies have been carried out to explore where muscular activity is recruited first in standing and walking. Humans are normally able to use different strategies when displacement occurs. The strategies depend on the situation; the sequence of muscle activation varies in relation to needs and possibilities. The response varies depending on the feet; if they are free to move or kept stationary when displacement occurs, whether the base of support is smaller or larger than the feet, how displacement is given and if the study participants are instructed to stay still or are allowed to move. In a free-standing position on a stable base of support, research suggests that motor activity is first recruited in relation to the base of support, i. e., the foot and ankle, lower leg, then more proximally, the arms coming last (Nashner 1982). Several authors who call this the ankle strategy support this concept. The ankle strategy opposes body sway in standing, and is based on a distal-to-proximal activation (Horak and Nashner 1986, Rosenbaum 1991, Rothwell 1994, Shumway-Cook and Woollacott 2006). If the base of support is smaller than the feet, for instance in standing on a narrow ledge, the displacement is fast or large, or the base of support is pliable; the ankle strategy may not be sufficient to maintain balance, and the hip strategy is used. The hip strategy activates lower trunk-, pelvic-and hip-related musculature first, i. e., a more cranial–caudal (proximal–distal) sequence of recruitment. More recent research has found that in many conditions, stepping occurs even if the line of gravity is within the base of support, when balance is not threatened (Maki and McIlroy 1997, Shumway-Cook and Woollacott 2006). Prince et al. (1994) studied balance control in the upper body during locomotion. Their results indicate that hip extensors and the erector spinae muscles are activated immediately after heel-strike, which is the initiation of stance phase. Hip extension stabilizes the pelvis shortly after heel-contact, while the main role of the paraspinal muscles is to oppose trunk flexion (Fig. 2.1). The balance of the upper body in relation to the pelvis and hips shows a cranial–caudal activation to stabilize the head first, then segmentally to the pelvis. When the arms swing during normal walking, the musculature in the region of T2–T6 is especially active. The trapezius muscle assists in stabilizing the shoulder at the end of each arm swing forward. Fig. 2.1 Rotation between the body segments during walking. The rotation occurs throughout the spinal column, but mostly in the mid-thoracic region. The pelvis and shoulder girdles rotate, and the extremities rotate in relation to their proximal attachments and the base of support. The line of gravity seems to be falling between the model’s feet. Normally, most people can adapt to the actual situation. Balance provides the body harmony and safety in relation to the environment, and is the foundation of our motor system. With reduced or no balance we have to use other strategies to prevent falls. Patients with neurologic conditions have lost some of their movement repertoire and are unable to adapt to the same degree as before. Therefore they have fewer choices open to them if balance is threatened. In my understanding, balance is a holistic term encompassing: • Postural control • Righting • Protective reactions The consequence of this specific behavior (humans’ ability to stand and walk) is that the nervous system automatically has to balance the body’s center of mass over the feet during all motor activities performed in a bipedal posture: every movement necessarily begins and ends with a postural adjustment (Dietz 1992). Postural control develops through the interaction of sensory, perceptual, cognitive, and motor systems as well as the musculoskeletal apparatus of the body. The desire to move combined with information received and modulated from all receptor organs and senses of the body forms the basis for execution of movement. Movement is constantly adapting to variations in the environment, goals, and situations. Postural control is recognized as a key component in the acquisition of independence in activities of daily living (ADLs) and IADLs (instrumental ADLs, for instance the ability to go shopping) (Hsieh 2002). Postural control depends on a complex interaction of afferent information and motor activity. Humans use multiple sensory references, gravity (the vestibular system), contact with the environment (somatosensory systems), and the relationship between the body and objects in the environment (vision), to maintain an appropriate relationship between body segments for balance. It appears that under normal conditions, the nervous system may weight the importance of somatosensory information for postural control more heavily than vision and vestibular inputs (Shumway-Cook and Woollacott 2006). There is a continuous adjustment of postural tone before, during, and after every movement. Anticipatory postural control is the pre-tuning of sensory and motor systems in expectation of postural demands based on experience and learning (Shumway-Cook and Woollacott 2006). Anticipatory postural adjustments are active before movement starts. Postural control in sitting and standing allows us to maintain activity against gravity. This provides us with a vertical orientation, an antigravity activity with alignment of body parts as a reference frame for balance, movement, and orientation. Muscular activity on all sides of the trunk is balanced simultaneously to allow selective, segmental extension of the spinal column and to free the arms for functional use. Abdominal muscle activity is important as a stabilizing factor for the segmental extension. Postural control has individual expressions. The nervous system seems to weight the importance of somatosensory information for postural control more heavily than vision and vestibular inputs under normal conditions. Equilibrium reactions are defined as automatic reactions that serve to maintain and restore balance through all activities (Bobath 1990). Edwards (1996) states that equilibrium reactions are synonymous with postural adaptations present in all daily activity. She uses the term equilibrium control to describe the ongoing segmental movements that compensate for displacement of the center of gravity caused by the actual movement or activity (Edwards 1996, refers to Massion 1992). The author understands equilibrium reactions and equilibrium control together as synonymous with postural control. The postural activity seems to be a result of changes of tone—a functional adaptation, i. e., altered distribution of activity in different motor units for the maintenance of stability, like ripples in water. We see the movement, but we don’t see the postural control. We see the activity, but we don’t see the stability. Postural control is like the part of the iceberg under the water, movements are like the small part above the water. We can see postural responses only in the feet, especially when balancing on one leg. Skilled movement has both postural and voluntary components: the postural component establishes a stabilizing framework for the second component the primary movement. Postural control is central to all human activity and adjusts continuously during activity. The aim is to maintain equilibrium during functional activity. It gives us stability together with an orientation to the environment. Postural muscles of the trunk, pelvis, and shoulder girdles contract before the arm is lifted in sitting or standing in order to stabilize the body by minimizing displacement of the center of gravity (Morris et al. 1994). Trunk control is only a small part of postural control; when the hand is used the wrist and palm are positioned to stabilize for individual finger movements. Postural control allows us a dynamic adaptation of background activity and is a prerequisite for dynamic alteration of activity in the extremities and therefore for selective movement. Clinically, reduced postural control seems to be one of the main problems for many patients with CNS lesions. A loss of a stable reference frame as a basis for voluntary movement causes balance problems, reduced coordination and interaction between muscle groups, as well as a reduced tempo and ability to react. Postural control counter-stabilizes movements of the extremities; if the body is not kept stable as a person reaches out in space, his body moves with the arm and he is destabilized. As a consequence, the person’s choice of how to solve different motor tasks becomes limited, which again may reduce his ability to be independent and master daily activities. Postural control and precise, goal-oriented movement are not separate phenomena in the CNS; they are coordinated together to allow successful achievement of motor tasks in a context-based environment. • Maintain the alignment of posture—different alignments for postural variations in different situations • Adopt a vertical relationship between body segments to oppose gravity • Create the posture of being upright—where grading of postural (muscle) tone is fundamental to this function • Control the position of the body in space for orientation and stability • Create a stable reference frame for the extremities and the head Postural control represents the most automatic activity in human movement (Massion 1992 and 1994, Mulder 1991 and Mulder et al. 1996), although it is probably less automatic than previously thought. To be able to maintain postural stability demands a certain level of attention, and studies have demonstrated that attention demands increase with increasing balance demands (Hunter and Hoffman 2001). Simultaneous demands for cognition and balance increase the tendency to fall in elderly people (Brown et al. 1999); dual tasks demonstrate the same relationship (Mulder et al. 1995). The combination of a cognitive task and a balance task result in a poorer solution of the cognitive task if it contains spatial elements (Brodal 2004). In the following section the term “postural tone” or “tone” will be used instead of “muscle tone” to emphasize that the CNS activates many muscle groups for the maintenance of postural activity. Shumway-Cook and Woollacott (2007) describe postural tone as an increased level of activity in antigravity muscles. The most important factor in altering the level of tone is muscular contraction (Brodal 2001). Tone gives an automatic background for activity and may vary from moment to moment. It needs to be high enough to withstand the effect of gravity and at the same time low enough to allow dynamic adaptation through small movements. Tone changes and adapts in relation to movements and the activities we perform. Postural tone has a wide spectrum in normal movement: it is normally at its lowest in relaxed supine, when the base of support is large and the center of gravity low. It may change in a millisecond as when we jump out of bed to run to the bathroom. In normal daily activity postural tone is at its highest in toe-off in stance phase, just before weight transference to the opposite heel. Humans may grade activity in the postural system as needed and through experience and exercise. The ballet dancer who dances on tiptoes or the tight-rope walker are examples of postural activity on a much higher level than needed for ADLs. Tone is highest in those areas of the body where the need for maintaining and sustaining activity against gravity is highest, and varies in relation to the base of support and the effect of gravity. There are individual differences in postural tone, some people have a naturally higher level of tone, and others are have lower tone. Psychologic factors may play a role; people who are anxious often have a higher tone than those who are laid-back. Gravity acts on the body at all times, whether at rest or during activity. The level of activity in different muscles depends on the orientation of the body and the extremities to gravity and base of support, the relative relationship between body segments, the activity to be performed, and the environment and experience. All ADLs demand that we relate to and oppose gravity, from turning over in bed, shifting our position, turning over pages in a book, and reaching out to turn off the light in bed, to initiating head movement for sitting up, getting dressed, and managing the bathroom, lifting a fork to eat, writing a letter, running after the bus, or walking in the mountains. The musculoskeletal system is constantly adapting to modify activity during changing relationships. Outdoors, even the weather and wind act on our bodies and demand postural adjustments. Descriptions that may seem artificial in relation to movement science on healthy people may seem logical in clinical situations. Against gravity is a term used in the treatment of neurologically damaged persons. Acutely after stroke, a spinal cord injury, or relapse of multiple sclerosis (MS), many patients suffer from severely low postural tone (Fig. 2.2) and are unable to activate or sustain activity against gravity and therefore also have problems moving. The base of support is the contact area between the body and the environment: the feet in standing; the thighs, buttocks, or back (if there is a backrest on the chair) in sitting; and the contact area between the hand and an object. The quality of the base, its size, material, softness, temperature, and the distance between the base of support to the center of gravity, are all factors of importance in setting the level of postural tone and our motor response: we lie down to rest and sit, stand, or walk when we want to be active. Fig. 2.2a, b The patient has had an acute stroke. a It seems as if he is either falling or pushing himself up with his right arm. He has very low postural tone and balance. He is unable to stay upright and interact with gravity. b He compensates by increasing his flexor activity in the right side of head, neck, and trunk in an attempt to pull himself up. Notice his right foot in both a and b, which seems to push against the floor and footrest. There is very little activity in his left side. These factors are not all-important, however; postural tone is not always low in supine. Most people will recognize the situation in the dentist’s chair: if you are uneasy or nervous, your postural tone is higher. In this situation, adaptation to the contact area is not appropriate, and you may have a feeling of being suspended in the air above the chair through muscular tension instead of resting in the chair. If a person sits uncomfortably, too still, unable to adjust or change position, postural tone may increase. Because recovery depends, to a large extent, on the ability of the CNS to adapt to (peripheral) changes, the study of recovery is largely the study of adaptation (Mulder et al. 1996). Recovery largely depends on the ability of the CNS to adapt to (peripheral) changes. The interaction with the environment demands a constant adjustment of tone, alignment, balance, and movement. This interaction depends largely on the ability to receive and perceive information from peripheral receptors and to adapt and adjust in response to this information. Our initial evaluation of conditions of the base of support is based on tactile information from base of support (BOS): feet (soles), bottom, and hands. We evaluate the support conditions by tactile contact. Our next calculation is of inertia; a smaller support means that inertia is more easily overcome and more quickly evaluated and assessed. The larger the estimation of the tactile area, the more difficult it is to overcome inertia. The relationship between the body and the base of support is the foundation for adjustment of tone to varying environments and activities. Tone needs to be optimal for the actual activity, whether it is to relax, to initiate movement, balance, or perform functional activities. In a functional context, the sensorimotor and perceptual interaction between the body and the base of support is more important for the level of postural tone than the size of the base of support. In standing and walking the feet need to be mobile and continuously adaptable to the environment. The feet transmit information directly between the body and the environment and must adapt and respond to the base of support and not react to the base with inappropriate tension—pushing or clawing—for balance to be optimal. The feet are our base of support, our foundation, in standing. They are sense organs that communicate the information they pick up about the base of support—unevenness, texture, hardness, direction, incline, and the distribution of body weight—to the CNS. The structure of the foot determines which rotatory components are available in the foot and leg during walking and running (Nawoczenski et al. 1998), i. e., patterns of movement. Alignment and neuromuscular activity in the feet have a significant influence on the alignment and neuromuscular activity in the rest of the body (Ljunggren 1984, Thornquist 1984). Eline Thornquist (1984) states that the load and tension condition of the feet influence our way of moving and determine to a great extent the movements available to us. She uses the words interplay, balance, and interdependence to describe the relationship between our foundation, physical and psychologic factors, and the environment. Changes in alignment and neuromuscular activity proximally will influence the ability of the feet to function as balance organs. In the CNS there is widespread integration of somatosensory information and motor activity. Afferent input via both the somatosensory systems and vision informs us of where we are in relation to the environment and is therefore vital to our ability to adapt to the surroundings and to a variable base of support. When we move through the environment, vision is important in setting the level of neuromuscular activity through feedforward planning (Wade and Jones 1997). If we are able to see, we scan the environment to pick up information about our surroundings, and alter direction or speed if appropriate. Vision does not direct the placement of the foot in detail under normal circumstances. If the terrain is uneven or difficult, vision becomes more involved but has no role in the actual adaptation and adjustment of the foot to the base. The feet respond immediately to unevenness and changes. When standing on a mobile base—in a bus, on a train or boat, or on an unsteady rock—there is a flood of information from the feet to the CNS about the properties of the surface and the line of gravity in relation to the feet. Postural tone is automatically adjusted to the situation and the goal. This adaptation is in response to information received through the somatosensory systems, i. e., feedback. Activity—the interaction with gravity—demands continuous interplay between feedforward and feedback. When the hands are in contact with objects or directly with the environment (surfaces), either to handle and manipulate objects or to seek support or reference, they need to interact, adapt, reach, and let go, and vary their activity in relation to the task. Neuromuscular activity, sensory information and alignment distally (i. e., in hands and feet) influence the activity and alignment in more proximal areas and reversely. Reciprocal innervation is the coordination of muscle activity for efficient, harmonious, rhythmic, and smooth movement without involving more effort than is appropriate for the actual activity (Bobath 1990, Edwards 1996). All complex movements are a result of finely graded interaction between external forces (gravity, inertia, and passive, biomechanical characteristics in involved structures) and variations in the tension—length relationships in the different motor units in agonist, antagonist, and synergic muscle groups. Reciprocal innervation tunes and balances muscle action, and I understand this to be the same as that which Sahrmann (1992, 2002) calls muscle balance (see Chapter 1.1 The Neuro-muscular System). Reciprocal innervation is described as the harmonious interplay in and between muscles, i. e., coordination between eccentric and concentric muscle activity leading to selective control of movement. Reciprocal innervation involves: • Differential activation of motor units in a muscle • Coordination of different muscles surrounding a joint—agonists, antagonists, and synergists—i. e., eccentric and concentric interplay • Coordination of different body parts, right and left, proximal and distal, through neuromuscular activity Neurophysiologically, the recruitment principle is an important element of reciprocal innervation; the motor units involved in an activity are sequentially recruited and modified through pre-synaptic inhibition (see Chapter 1.1, The Neuro-muscular System and The Spinal Cord and Brain). Reciprocal innervation is the foundation for stability, selectivity, and coordination in normal movement. Postural stability is not related to the trunk alone, even if the trunk is essential for postural control. Postural control is a basis for all components of movement. For instance, when changing a light bulb above your head, the whole body needs to be stabilized and oriented toward the manipulation of the bulb into the socket while the hands, wrists, and forearms are the main components of the function of rotating the bulb into place. Inherent in the term postural control are its dynamic characteristics. The body is multi-segmental with lots of rotatory, translatory, and multidirectional joint movements and muscles that need to be controlled. Bernstein called this the degrees of freedom problem (Bernstein 1967 in Shumway-Cook and Woollacott 2007). Some activities may push stability to the limit and beyond, and necessitate a change of base of support, e. g., taking a step. Some tasks will focus on attaining the goal rather than maintaining stability limits, e. g. the keeper who throws himself to catch the ball, while the fall itself is as controlled as possible. Stability is a result of forces being balanced in relation to each other or equal to each other. In normal movement, stability is always dynamic, i. e., movement also occurs in stabilizing segments. Even as we stand still, there is a segmental adjustment through the body. The ability to hold a position demands continuous adjustment of neuromuscular activity. Stability allows movement between body parts. To reach out for an object, the body must stabilize and stay, then gradually move with the arm to reach further if necessary. As we reach, the hand initiates the actual movement of the arm while feedforward mechanisms (i. e., anticipatory postural adjustments) stabilize the body. During forward locomotion, the neuromuscular activation of the hip and pelvis has to maintain the stability of these segments at the same time as we are moving forward in space, and the hip joint rotates and changes from flexion to extension. As we reach swing phase, the activity changes; tone is reduced to allow a free swing. Stability areas vary, depending not only on the function, but also on all phase changes of movement, i. e., continuously. Therefore, mobility is essential for stability, as is stability for movement. The trunk may stabilize for movements of the extremities, the extremities may stabilize for trunk movement, the upper trunk may stabilize for pelvic mobility, pelvic area for trunk movements, the right side may stabilize for movements of the left half of the body, and so on. Even distally, the lower arm must be stabilized for movements of the hand and the wrist for the movements of the fingers. The same is true for the lower leg and foot. Stable areas of reference adapt and may change through the evolution of movement. Mobility is essential for stability, as is stability for movement. Selective movement is understood as the controlled, specific, and coordinated movement of one joint or body part in relation to other segments. Selective movement is the result of precisely graded neuromuscular activity based on reciprocal innervation. Stability and selectivity are both dependent on adequate ranges of motion, muscle length, alignment, and the coordination of agonists, antagonists, and synergists in concentric and eccentric work. Eccentric muscle activity is the result of active, neurophysiologic processes. Reciprocal innervation leads to the ability to: • Automatically adapt muscle activity for postural adjustments • Stabilize for selective movement • Grade the activation and interaction of agonists, synergists, and antagonists for precision in timing and direction Postural orientation involves: • The ability to maintain an appropriate alignment between body segments • The ability to maintain an appropriate relationship with the environment • The need to establish a vertical orientation to oppose gravity • Creating a reference frame for perception and action Dexterity, i. e., flexibility and skill in movement (not only distal, manipulatory skills; see Chapter 1.3, Upper Motor Neuron Lesion) enables adaptation to the here and now situation, and depends on postural control. Postural control is the basis for all voluntary motor skills (Massion and Wool-lacott 1996). Information that is needed to maintain postural control is crucial for conscious awareness of our own bodies, spatial orientation, and internal models (Brodal 2004). Internal models are the stored information needed for specific activities such as walking down stairs or reaching for something in space (see Chapter 1.1, Cerebellum, Clinical Hypotheses). Neural networks in the cortex coordinate the different sensory modalities and give them meaning. Postural control therefore creates a reference frame for perception and action in relation to the world around us (Brodal 2004). Body schema may be described as an internal postural image that informs us of the position of the body segments in relation to each other. It therefore provides a foundation for the exploration of space—the environment—for perceptual analysis and motor action. It is monitored by multiple sensory inputs. We need detailed information from all our sensory receptors to create and continuously update a body schema in order to balance and move: • Information from proprioceptors: – The muscle spindles—Ia afferent input is necessary for the anatomic relationships of the different body parts, i. e., activity. Studies imply that information from the hips and the trunk itself is important to trigger a person’s balance corrections. Proprioceptive information from the lower legs aids in the final adjustment and intramuscular coordination of postural programs and locomotion patterns (Allum and Honegger 1998). – The Golgi tendon organ measures the number of active motor units at a given time in each muscle used in postural control (Massion and Woollacott 1996). – Joint receptors – Skin receptors • The ability to evaluate the base of support: – Low threshold mechanoreceptors (pressure receptors) in the soles of the feet – Plantar cutaneous information (Kavounoudias et al. 1998) • The probable presence of graviceptors in internal organs: – Graviceptors are specialized sensory receptors detecting displacement of weight in relation to gravity, for instance the weight of shifting fluid in the intestines and kidneys. Recent research has argued for a separate pathway in humans for sensing body orientation in relation to gravity (Karnath et al. 2000a). – There is preliminary evidence to suggest that somatic gravity receptors, originating in the trunk, exist in monkeys and humans (Di Fabio et al. 1997). • Information from the vestibular apparatus in the inner ear that senses the orientation, movement, and acceleration of the head in space in relation to gravity • Vision detects movement and monitors the displacement of the head and body in relation to the environment Information reaching the central networks for postural control must be modulated, evaluated, and acted on. Postural control requires good alignment (biomechanics), appropriate muscle strength, and all the above-mentioned information to be appropriate to the activity of the moment. Fig. 2.3 and 2.4 Compare the patterns of movement in the two pictures. In Figure 2.3, the patient’s center of gravity is to the right of his right leg, and he presses actively (down on his walking stick). Therefore, the flexor activity in his right side is increased at the same time as he seems to lift his left side forward with his right. There is decreased mobility and interplay between body segments generally, but especially proximally. The patterns of movement in his arms and legs are stereotypical. Rotation in his left leg does not change to swing the leg forward. There is reduced dorsiflexion in the foot. This could be caused either by stiffness of his calf muscles or weak dorsiflexors, or malalignment of the whole leg negating the activation of dorsiflexion. Figure 2.4 shows a healthy young woman who is taking a step forward with her left leg. Notice the extension over the standing leg and the interplay between body segments. On the swinging side the pattern of movement changes from stance phase activity (more extensor/abductor/external rotation activity) to let go of the same activity through rotation to swing the leg forward. The left dorsiflexion ensures clearance of the floor. Patterns of movement are sequences of selective movements that vary from person to person, the task at hand, and the situation (Figs. 2.3 and 2.4). Movements are the output of a dynamic interaction between muscular forces and peripheral field effects (e. g., gravity, friction, joint reactive forces) and can be described in terms of their pattern, displacement, or topology (Mulder et al. in Harrison 1995). The motor system has to contract the agonist with the right force at the right time as well as time and organize the contraction patterns of the antagonists, synergists, and postural muscles necessary for the agonist in the actual function. The number of muscle fibers and motor units recruited in a muscle varies depending on the function and other muscles that are recruited in relation to the task. The anatomic construction of the skeleton enhances coordination and rotation between the different body parts. The muscles cause rotation to varying degrees depending on the anatomic form and arrangement of the muscle fibers, their function, and the organization of different parts of the muscle to each other (alignment) and their attachments. Examples are the tendo-Achilles that is rotated 90h before its attachment to the calcaneus, and the pectoralis major that is rotated 180h before its attachment to the humerus. Rotation is an essential component of normal movement, and it gives enhanced proprioceptive feedback to the CNS compared with, for instance muscle palpation or tendon tapping. Humans move along three planes: sagittal, frontal, and transverse (or horizontal), and this is combined through rotation. All weight transference and movement demand rotational components. We vary between symmetry and asymmetry caused by interplay between body segments through rotation. Rotation is based on the ability to grade and combine flexor and extensor components in infinite variations of movement patterns, and gives flexibility and resilience. Rotation, for instance between the upper and lower arm and between the thigh and lower leg, in relation to their proximal segments, and through trunk rotation cause a functional diversity that allows anything from fine motor activity and distal dexterity to coarse grasping and locomotion. Basic patterns of movement are reach and grasp and stance and swing. These patterns vary infinitely depending on the task and the environment. Reach and stance are both patterns that are mainly dominated by components of extension, outward rotation, and abduction. Grasp and swing have more flexor components to their patterns, often with components of outward rotation and adduction. When the arm is by the side, the hand is brought to the mouth through flexion/adduction/external rotation initially changing to graded internal rotation of the shoulder, flexion of the elbow, and supination of the forearm. The patterns interchange and vary in all our activities: we position ourselves in more extension if we need to reach out for something above shoulder height, when performing activities that demand fine eye–hand coordination we often chose to sit in a more flexed position—based on eccentric trunk extensor activity. Normal postural tone and normal reciprocal innervation allow individuals to choose their own background neuromuscular activity as is most appropriate for the situation. Normal postural control allows us to: • Oppose gravity • Move • Develop functional skills Righting refers to observable movement between body segments in relation to each other and to the environment, and happens when the line of gravity moves toward the limit of the support surface. The movements that represent the ability for righting are part of our most automatic balance control as well as being voluntary. Activities such as turning over in bed, changing direction in walking, sitting up, or standing from sitting are examples of righting. A person rights himself in relation to the task, environment, and the effect of gravity (Figs. 2.5–2.7). There is a continuous adjustment of muscular activity to maintain equilibrium at the same time as righting occurs. There are two main forms for righting: • Head righting—the head rights itself on the trunk as a response to displacement and aims to maintain the vertical position of the head. • Trunk righting: – When the trunk moves in relation to the base of support. All weight transference and positional transfers require changes and adjustments in activity between the shoulder girdles, the thorax, and the pelvis. – When we turn our head to look about or change direction, the body follows and rights itself in relation to the movement of the head. – When we sit up the head leads the sequence of movement. The abdominals stabilize the thorax and allow the neck flexors to take the weight of the head. The trunk moves and follows the head until the center of gravity is within the new base of support in sitting. The first part of this movement is trunk righting, as the new base has been acquired head righting follows. Fig. 2.5a, b The two figures show the interplay between righting and postural control as the arms reach up. Thoracic extension enhances the full range of movement at the shoulders and allows a further reach. Fig. 2.6 Postural control, righting, rotation, and weight transference interacting in the function of fetching a book. Thoracic extension, based on core stability allows postural control and rotation. Righting is an essential and basic component of the ability to move from one position to another: weight transference, transfers, changes in the direction of movement, and for the development of protective reactions and movement strategies. Righting is therefore essential to all our functional activities. If righting is inappropriate or inadequate to maintain balance, a person takes a step or uses his arms to protect himself from falling. When we step to avoid falling, and if the displacement is very sudden and the feet are free to move, anticipatory postural adjustments may not always be present (Maki and McIlroy 1997). Steps in this situation are more of a reaction, but elements of planning and strategy are present in the background at most times: we place the foot in the direction in which we are likely to regain balance. However, when we step to initiate locomotion, we plan ahead and initiate feedfor-ward strategies. Stronger cognitive elements are now present, and this is therefore not a protective reaction. Fig. 2.7a, b If the trunk is flexed, the center of gravity falls to the back of the base of support. As the arms reach above the head without the trunk righting itself, the reach is more limited. The arms are recruited in a protective reaction if stepping is not possible or inadequate. Often some elements of planning will be present: we place the arms where they may most appropriately save us or lessen or grade the fall. Balance is expressed in both reactions and strategies. Postural control, righting, and protective reactions are elements of balance. The midline is a term that is frequently used clinically. It is a broad term that is difficult to define precisely. Midline refers to the interplay of body segments and alignment, and involves both physical and perceptual factors, like body schema. We explore and adapt to our environment, and action requires perception, balance, and movement. We have to perceive our body in space to adapt to the environment. The term midline control refers to both an ability and an experience of being balanced. It seems appropriate to distinguish between postural control and righting because they seem to be functions of different systems, and may therefore guide particular therapeutic interventions. Postural control is not under direct cortical control. There are indirect connections through the reticular formation and the cerebellum. Postural control can therefore not be regained through verbal instruction. Postural control requires segmental displacement and interaction with gravity. Therefore, the therapist should ensure that the patient has segmental mobility, for instance of the spinal column. Righting seems to be a result of activity in many interacting systems: cortical, cerebellar, vestibular, reticular, and spinal. Therefore it can be influenced both through verbal instruction and handling (hands-on). Postural control and righting are the foundations for head control. Patients with CNS lesions are heterogeneic and show individual characteristics; lesions in a similar location and of a similar size in two patients will manifest differently. Patients have different personalities, talents, and experiences that have shaped their body and mind. Some patients may present with other medical diagnoses as well, such as diabetes and cardiac problems. Some patients may be in poor general condition for different reasons. The aim of treatment is to enhance the patient’s potential as much as possible, keeping this heterogeneity in mind. Many patients will not reach the same level of function as before the lesion and will have to compensate to be functional within their environment. Shumway-Cook and Woollacott (2006) define compensation as behavioral substitution, that is, alternative behavioral strategies that are adopted to complete a task. The two terms compensation and compensatory strategies are perceived to mean the same. In the acute phase there is often seemingly severe paresis or paralysis after an upper motor neuron lesion. The CNS is vulnerable in this phase (see Consequences and Reorganization after CNS Lesions); the concentration of neurotrophic substances increases and facilitates the formation of new connections. We learn by doing, and the patient’s CNS quickly learns new strategies that may seem appropriate for the moment. What the patient is stimulated to do, or required to manage do to by people, himself or the environment, drive the formation of new connections. Many patients are required to master independence in activities of daily living without having the postural or movement control needed to do so. When the patient sits alone on the side of the bed in the first few days, he is driven to compensate if he lacks the postural control to do so safely. If compensation leads to goal achievement, the drive toward improvement may stop. The brain is oriented toward immediate success and rewards, not to the process involved in reaching the goal. The compensatory strategies will be learned as relevant and appropriate for this stage. Held (1987) states that: “In other words, if compensation is allowed to occur, there is apparently no stimulus to the partially damaged system to recover and behavioral substitution will occur.” This may be explained by reactive synaptogenesis (the formation of new synapses and collateral sprouting) forming abnormal connections that compete with more appropriate connections. Compensation may therefore limit the neural functions that are spared after lesions. Clinical experience supports the theory that therapy may influence the restructuring processes in the lesioned CNS (see Chapter 1.2 Plasticity, Reorganization of Cortical Maps and Neurotrophic Factors). The CNS recovers very quickly after the initial shock, and some functions may be spared: as edema and the penumbral zone shrinks and circulation improves, neurons start working again and some functions return; this is called spontaneous recovery. If the patient learned to use compensatory strategies during the acute phase, these may not be necessary any longer. But if the CNS experiences these strategies as appropriate in the acute phase, they may be established and difficult to change. The strategies will often have developed based on the need to balance; as balance and movement control is reduced or absent to prevent falls or the feeling of insecurity, therefore they often involve fixing with the arms, grasping, and holding on, weight transference to the least affected side in stroke, fixing through flexion of trunk or flexion/adduction of hips, or pushing off the floor. This development may be illustrated as follows (Bryce 1989 in Edwards 1996, p.19; Fig. 2.8). Reduced postural tone and loss of reciprocal innervation as the basis for coordination as well as weakness influence the patient’s balance and quality of movement negatively; postural stability and orientation are reduced, and therefore also the control of movement. The main aim of the CNS is to ensure the person’s safety, and therefore available alternative strategies are recruited and enhanced. The sequence of recruitment (Henneman’s recruitment principle) and the sensorimotor organization of activity are altered as a response to balance impairment. The feedback to the CNS of the execution of movement through peripheral receptors will be different due to the movement being different and to the altered integration and modulation of sensorimotor activity: previous responses, feedback from a healthy system, and normal movement repertoire. The basis for the execution (i. e., anticipatory postural adjustments) of the next movement and movements in the future will therefore be altered. Fig. 2.8 Development of an abnormal postural tone. After a CNS lesion patients alter their strategies to compensate for loss of or reduced balance control. Many patients develop cognitive and visual strategies that seem to override the integration of information from somatosensory receptors—they do not listen to their bodies any more. Movement becomes slow and patients poke their head forward and look down to enhance visual information (this change in alignment of the head and neck will influence the vestibular system). With this increased dependence on cognitive strategies and vision, patients are increasingly prone to falls if they are distracted or people catch their attention. Mulder et al. (1996) propose three measures for the improvement of balance: reduced cognitive regulation, decreased dependency on vision, and increased sensorimotor adaptation. When we have the ability to balance, we rarely think of it; if we don’t have it, we think of it all the time. CNS lesions result in a move away from automatically regulated background control of balance and postural control to increased awareness and cognitive regulation of balance. Which balance strategy the patient adopts depend on his build, experience, personality, and the consequences of the lesion. Inappropriate compensatory strategies—alternative behavioral strategies—may delay or hinder the development of balance and selective motor control in patients with CNS lesions. Clinical examples Balance develops through interaction with gravity. We have to be exposed to gravity to develop postural control in standing, sitting, step standing, and walking. sberg (1989) found that stroke patients had improved orthostatic blood pressure, improved ADLs, and had fewer severe functional impairments and limitations after being placed in the standing position early and on a regular basis (every day for 12–days after admission) compared with patients in the control group. The differences between the groups were significant, and no other interventions could explain these differences. At the same time, it is not proved that early standing alone caused this, but sberg recommends early standing as a treatment intervention. Jacobs et al. (1985) found that a group of trial participants significantly improved their perception of trunk orientation (trunk positional sense) in relaxed standing compared to lying. These studies support the importance of early standing both for functional improvement and the patient’s perception of his body. Standing seems to improve both trunk positional sense and overall function. Normally the hip and pelvis are stabilized in stance phase for the swing of the opposite leg. This stability is dynamic, the pelvis and hip move in relation to each other, the trunk, and the base of support to allow the translation of the center of gravity in the direction of movement. Stability is maintained over the standing leg throughout this movement. Neuromuscular stability is a prerequisite for selective movement control. In clinical practice the therapist will meet patients who have reduced or altered recruitment of appropriate stability and movement. Many patients have instability both truncally (core stability) and over the pelvis and hips. Reduced stability or increased trunk flexion seem to prevent activation of hip extension, necessary for stability. At the same time, reduced stability over the pelvis and hip may influence trunk stability negatively. Weight transference in standing may increase compression of the ankle and thereby deform the foot. As a result, alignment is changed distally compromising the recruitment of neuro-muscular activity proximally. Patients compensate in different ways: shifting their weight onto the least affected side or body parts (Fig. 2.9), using the environment for support, enhancing the support and protective reaction of the arms, fixing within their own body, recruiting activity more proximally—a shift from ankle to hip strategy—there is an infinite variety of possibilities. Many patients are not able to step due to reduced stability of the standing leg. They move their strategies more proximally to their arms. Patients use arm support in different ways: fixing through adduction, inward rotation of the shoulder, and through increasing their flexion activity in the trunk, fixing through increasing flexion/adduction, compression of the hip, etc. The muscular interplay and muscle balance for selective stability necessary for maintaining a free standing position, weight transference, and walking are disturbed. Clinically, it may be necessary for two or three therapists to work together to facilitate trunk, pelvis, and hip activity for stance phase to allow for swing phase. If appropriate and available, a treadmill with body weight support may be of some help to ease the facilitation and rhythmic interplay between stance and swing as well as finding the right speed to facilitate central pattern generation in the individual (see Chapter 1.1, The Spinal Cord, Central Pattern Generators). Speed is very individual. Sometimes an orthosis or splint may be appropriate to stabilize the ankle. Heel-strike and heel-off seem to be important to signal phase changes to the patient’s CNS, therefore the heel should, if possible, be free to receive and transmit somato-sensory and weight information. Therefore, an orthosis that stabilizes the ankle medially and laterally or taping may be of use in a period of transition (Fig. 2.10). Fig. 2.9 The patient’s left shoulder girdle and pelvis is retracted, the left leg is pulled back with the pelvis and therefore seemingly outward rotated and adducted. The arm is pulled back with the shoulder girdle but is observably inwardly rotated and adducted with flexion/pronation of the elbow and lower arm. The stability and movement control is reduced on both sides (see also Fig. 2.3) but more on the left, most affected side. His body weight shifts toward the right in both standing and walking. In patients with Parkinson disease, one of the early symptoms is a flexed posture and lack of rotation. One of the early motor symptoms is reduced muscle function in the trunk (Bridgewater and Sharpe 1998), which causes reduced postural control. The patient’s reduced ability to right himself increases the flexor tendency and inhibits rotation. Flexion causes a forward lean of the trunk and displacement of the center of gravity, and the patient develops a tendency to fall forward. Patients have a shuffling and tripping gait with short steps and seem to be running after their own center of gravity. Some patients develop compensatory strategies in an attempt to bring the center of gravity back by pressing their feet into the floor through plantar flexion. Bridgewater and Sharpe (1998) refer to other studies in which dorsiflexion was found to be reduced. Trunk flexion and rigidity combined with pushing back from the feet cause the patients to lose mobility and to seem stiffened in their total expression of movement. Plantar flexion contractures may develop as a result. Figs. 2.10a–f This stroke patient has congenital hip dysplasia and 7 cm difference in leg length, the shorter leg being his left. He has always walked on his toes on his left side, and perceived no balance or movement problems and no restrictions in function or participation. Among other things, he and his wife used to dance a great deal. He then suffered a stroke, resulting in left side affection and motor apraxia. He had a lot of instability on his left side, no hip, knee, or ankle stability or voluntary movement. To help increase the stability of the ankle, the ankle was taped to recruit more proximal stability. Notice the difference in alignment and therefore the ability to recruit more appropriate neuromuscular stability in Figures 2.10a–f. Note: Taping is not a long-term solution; it may cause skin problems and is difficult for the patient and his carers to put on. After some time this patient received a sport bandage, which gave adequate stability distally. Fig. 2.11 The patient shows reduced balance as a result of an acute stroke. He has reduced tone on his left side and lacks the interplay of movement between body segments in all three planes. By improving mobility of the spinal column, shoulder girdles, and neck and facilitating selective extension, rotation is often spontaneously regained. The feet and muscles of the lower leg should be maintained at an appropriate length for mobility. Through improved distal mobility the patient will be able to receive and perceive somatosensory information and orientation of his body in relation to space and the support surface. These interventions may improve the patient’s ability to adjust his posture and thereby balance. Some stroke patients seem to develop a tendency to push away through their least affected extremities. This is a complex combination of symptoms, and mostly seen in patients with left side affliction (right hemispheric stroke). Clinically, the patients are often totally paralyzed on their affected side for a relatively short time initially (Fig. 2.11). Many names have been given to this syndrome; postural hemineglect (Sch ger and Kool 2001), the pusher syndrome (Davies 2001), contraversive pushing (Karnath et al. 2000a), etc. Vestibular information is probably integrated in a widely distributed cortical network (Brodal 2001). At least two centers in the brain seem to be involved in the regulation of vertical perception and summate to achieve postural orientation of the vertical axis: • Subjective postural vertical (SPV) is a sensitive direction-specific orientation for vestibular function which receives input from sense organs in the trunk—a truncal gravitation dependent system • Visual subjective vertical (VSV) is a visually perceived sense of being vertical that depends on visual, proprioceptive, and vestibular inputs Figs. 2.12a, b The patient pushes with his right arm and leg. a There is severe side flexion throughout the right side and the pelvis is elevated on the right side. His interaction with the base of support and between body segments is disturbed. He is malaligned and out of midline. b The therapist handles the patient to improve the alignment of his pelvis to the base of support. The patient pushes less, but there is still observable malalignment of his upper trunk and head. If perceptual systems are conflicting and mismatch, the patient may develop a “pusher syndrome” (Karnath et al. 2000a and b, 2001, Lösslein and Kolster 2001, Schäger and Kool 2001). They fall to the left side (usually) and their eyes perceive the world on a slant to the right. The cortex listens to the system it trusts most. In some patients, therefore, the input from the eyes will dominate and override positional information. The patient’s subjective vertical is 101–7h to the left, but they think that they are falling to the right (Fig. 2.12). There is increased flexor activity throughout the right side of the trunk and neck whilst pushing away from the right using the right arm and leg, and little or no activity throughout the left side. This is not a primary perceptual dysfunction, but as the patients receive conflicting information from the PSV and VSV of where they are in space, combined with flaccid paralysis and no information from the paralyzed side, they may develop perceptual problems. Perceptual problems that are often observed in patients with “pusher syndrome” are: • Visual neglect: Some patients do not seem to perceive visual information from the most affected side. • Neglect of the most affected side of the body: The patient has reduced perception of the most affected side and does not integrate information from this side. But, as previously stated, this syndrome often involves flaccid paralysis initially, therefore there is very little somatosensory information to receive or integrate. • Spatial problems, both in relation to one’s own body and to the relationship between the body and the environment • Reduced sensory perception, but the patient may have normal sensation if the two body halves are tested separately. Often the therapist finds that the patient has severely affected bilateral simultaneous perception of sensation. • Altered perception of the midline: The patient is afraid of falling to his least affected side. • Other perceptual and cognitive problems Physical problems that could occur are: • Hemianopia: The patient has reduced visual field to the paretic side. • Initial paralysis, which seems to recover quickly in many patients. They may have relatively good selective movement in the most affected side, but cannot use it because of severe midline disorientation. • Reduced postural control • Reduced weight transference, reduced interplay between left and right, reduced righting of head and trunk • Use of the least affected extremities to push with. If the patient has a right hemispheric stroke, his head, neck, and trunk are sideflexed to the right, and the head often rotated to the right. An increased use of protective reactions and strategies (the push from the right to avoid the perceived falling to the right) seem to inhibit the interaction of right and left in all three planes. If this syndrome is not treated successfully, patients develop severe flexor/retractor activity throughout their most affected side and are totally dependent on carers for all functions. They demonstrate inappropriate use of their least affected side, and their ability to vary patterns of movement is reduced. Often, carers and therapists experience lots of resistance when attempting to correct the patient’s alignment and relationship to the base of support. There may be bilateral problems, and problems arise in all practical situations that require balance and transfers as well as positioning in a chair and in bed. Treatment is goal-oriented toward regaining midline control. The following factors are important to evaluate: • The patient’s awareness of and activity in his paretic side • Regaining interaction of movement between body segments in all three planes, especially trunk, shoulder girdles, and pelvis • Improvement and facilitation of distal sensorimotor integration • Interaction between the right and left side to regain trunk and head righting and postural control In a treatment situation perceptions need to be matched. Vertical orientation requires alignment of the pelvis and intra-abdominal pressure. Therefore vision may be taken away (the patient blinded or vision blocked to the right) combined with using a broad bandage or belt to assemble the trunk and abdominal contents in the midline to increase abdominal pressure. Lying on the right side or with the right side supported in sitting and standing may make the left side more available for increasing the somatosensory information through the left side. Some patients develop a hypersensitive foot that pushes off the floor through plantarflexion and inversion (Figs. 2.13–2.14). They may experience a primary hypersensitivity toward stretch, touch, or weightbearing to the forefoot or this reaction may develop as a response to gravity in order to stiffen the leg to be able to stand on it to walk when the proximal areas are too weak or unstable to carry weight selectively. The severity of the reaction will vary in different patients and in different situations. Pressure, touch, or stretch to the foot in weightbearing cause plan-tarflexion with a backward translation of the tibia in relation to the foot. The pattern causes plantar flexion with varying degrees of inversion, a mechanical hyperextension of the knee as a result of the plantarflexion and is usually combined with flexor components at the hip, i. e., varying degrees of flexion/adduction/inward rotation. The mechanical hyperextension of the knee is a result of the knee being caught in the middle between a plantarflexed foot and a flexed hip during weightbearing. Quadriceps is rarely active in this reaction. The incoordination of foot, ankle, knee, and hip negatively affect balance and reduce interplay and variation of movement. Figs. 2.13a, b When this patient stands up from sitting he uses a lot of effort. Note the facial expression and the associated reactions in the arm. Compare with Figure 2.9, where the associated reactions are less when the patient has been standing for a short time. The transfer to standing demands interplay between body segments and the base of support. The patient has very little mobility generally, and his left foot is not adapting to the base of support, therefore weight transference to the left is not possible. He has to compensate by pushing up through his right side. This patient had two strokes approximately 30 years ago. He manages most activities and is active in participation. But it is costing him a lot of effort, and he becomes tired, more so as he is getting older. Flexor withdrawal may be caused either by a hypersensitive foot or sensitive (short) hip flexors (flexor reflex afferents), therefore either from a distal or a proximal initiation: • Weight transference through the foot causes stretch of the soft tissues within the foot. In some cases initial stretch in attempted weightbearing produces withdrawal of the foot from the floor. The pattern varies in severity and rotational components, but usually causes inversion of the foot and flexion of the hip and knee. • Withdrawal reaction may also be caused by stretch to the hip flexors, often initiated as a reaction when the patient starts to raise himself to standing from sitting. The stretch of the hip flexors causes hip and knee flexion combined with dorsiflexion of the foot with varying degrees of inversion or eversion depending on the neuromuscular rotational components of the hip. Figs. 2.14a–c Reduced adaptability of the foot in standing and walking. The left knee is hyperextended, the hip flexed. Stability is reduced over his left side and effort increases as balance requirements increase during gait judging by the level of associated reactions (compared with Fig. 2.9). All of the above-mentioned deviations prevent normal weight transference, balance, and transfers. Treatment is targeted toward the impairments: the hypersensitivity, the immobility of the foot, and improving muscle length and flexibility. Improving postural control, especially the stability component in different situations, involves bringing all the following into activity through graded weightbearing and varied active movement over the foot in different weightbearing activities: sitting to standing over one or two feet, controlled standing to sitting, standing and step standing, stepping in different directions, one-legged standing, stepping down from a height, sitting on one or two legs, stairs, etc. The restoration of dynamic interplay between the foot, knee, and hip is essential to the patient’s ability to balance and move. On the basis of continuous assessment and clinical reasoning the therapist chooses interventions that seem appropriate to the individual patient. The Bobath concept does not give a solution or method for treatment of patients. The current definition of the Bobath Concept is: It is a problem-solving approach to the assessment and treatment of individuals with disturbances of function, movement, and postural control due to a lesion of the central nervous system (IBITA, Theoretical Assumptions 2007; www.ibita.org). Treatment is tailored to the individual patient, and is response-based. Therefore interventions depend on the individual patient, his sensorimotor dysfunctions, his perceptual and cognitive resources and problems, the adaptive compensatory strategies developed, the environment, and the goal or task. All interventions, even if impairment-oriented, need to integrate activities to make treatment as functional as possible and the carry-over effect as strong as possible. Motivation is a crucial factor to learning. Treatment incorporates: • Regaining movement control • Motor learning • Interdisciplinary approach to enhance learning and carry over • The use of compensatory strategies when further motor learning does not seem possible (may incorporate the use of aids and orthoses) • Management strategies to prevent or minimize complications Berta Bobath described postural sets as “adaptations of posture” which “change with the intended movement—in fact, they may precede it” (Bobath 1990, p. 68). Body segments have a bio-mechanical and a neuromuscular relationship, both of which are the basis and consequence of the build of the individual, movement, and the actual relationship with the environment. This relationship continuously changes during activity. Neuromuscular activity and biomechanical factors influence and are affected by each other. Changes in the relationship with the environment and alterations in the biomechanical relationships through changes in rotational components or direction of joint movement require adaptation of the neuromuscular activity, even if the goal of movement or task stays the same. Neuromuscular activity depends on where the person started the movement from, i. e., standing up from sitting on a low, soft cushion or stepping down from a high seat. When a person flexes his elbow in sitting or standing, the biceps is the prime mover. The same movement performed in supine, with the arm stretched up in the air or the arm being held over shoulder level in sitting or standing, requires more eccentric control from the triceps as the prime mover and agonist. The neuromuscular activity required to perform pelvic tilt varies in different positions because the biomechanical relations alter with the changing relationship of gravity to the base of support. Therefore, the activity is different in sitting, in the transition from sitting to standing, in standing, through sitting to supine, and in supine. Analysis of movement is the detailed analysis of movement during every phase of an activity to form hypotheses for the patient’s recruitment of neuromuscular activity in function. This analysis is the foundation for clinical reasoning, together with an analysis of the patient’s performance that includes an assessment and evaluation of perceptual and cognitive function. Postural sets describe the interrelationship between body segments at a given moment. Movement may be described as a continuous change of postural sets. If serial photographs of a movement or activity are taken, each photograph represents a postural set. Analysis of postural sets gives information about: • The effect of gravity • The relationship to the base of support • Alignment • Ppatterns of movement • Neuromuscular activity There is an interrelationship between postural control and postural sets. The analysis of postural sets in a functional activity allows the clinician to observe actual and gradual changes in alignment and to form hypotheses regarding the neuromuscular activation creating the movement. The chosen interventions may or may not support the hypotheses. If the patient’s motor control is not improving, either the interventions or the hypotheses may be wrong and must be reconsidered. The clinician must continuously adapt the interventions to the patient’s response and required movement. Postural sets are also used in treatment to adapt and adjust requirements to suit the patient’s ability. The choice of postural sets depend on the patient’s balance control and relationship to the base of support, and therefore the choice of goal activity or task. If the patient has low postural control, or is flexed with asymmetry, malalignment, and deviant tone distribution, he will not be able to recruit a more appropriate activity to interact or respond to the environment. Shumway-Cook and Woollacott (2007) describe ideal alignment in relation to the standing position as follows: “muscles throughout the body, not just those of the trunk, are tonically active to maintain the body in a narrowly confined vertical position during quiet stance. Once the centre of gravity moves outside the narrow range defined by the ideal alignment, more muscular effort is required to recover a stable position.” Optimal or ideal alignments in any postural set allow us to use no more effort than necessary to maintain stability. Inappropriate alignment or malalignment may maintain an inappropriate neuromuscular recruitment pattern and thereby prevent the patient adapting his response to the environment. Sahrmann (1992) states that a normal neuromuscular interplay, muscle balance, or adaptive muscular activity facilitates good alignment, and that good alignment facilitates normal, adaptive neuromuscular activity. A selective movement in one postural set requires a different neuromuscular activity in a different postural set. As the biomechanical alignment changes, so does the neuromuscular activity.
Introduction
2.1 Balance and Movement
Human Movement Control
Balance
Postural Control
The Function of Postural Control
Postural Tone
Righting
Protective Reactions and Strategies
Clinical Relevance
Deviations from Normal Movement and Balance Control
2.2 Intervention—Considerations and Choices
Postural Sets
Physiotherapy
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree