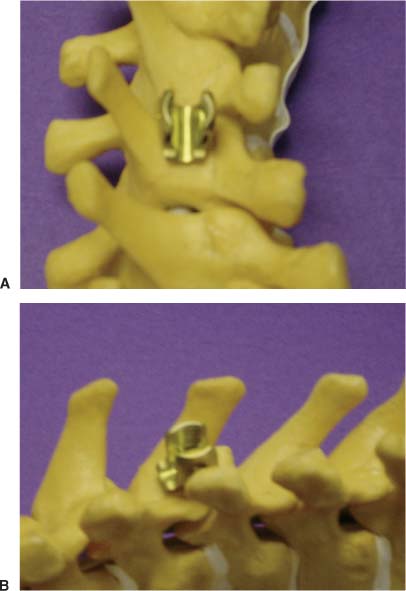
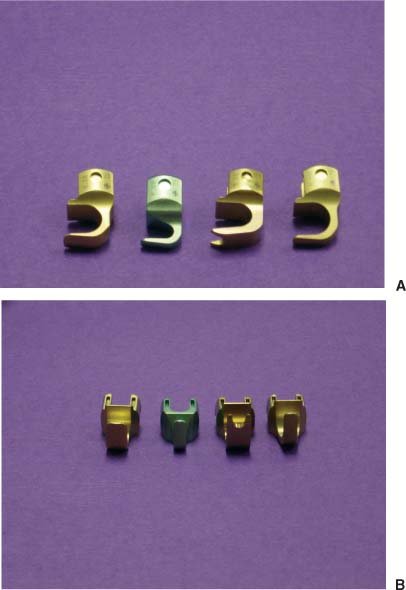
39 Hook-and-rod constructs for the treatment of instability of the thoracic and lumbar spine date back to the 1960s with the advent of the Harrington rod systems. These basic systems underwent a series of advances and modifications. The concept of segmental control with hooks and rods by Cotrel and Dubousset was the next great leap in reconstruction of the spine.1 This development paved the way for modern hook-and-rod reconstruction systems and the latest concepts for thoracolumbar spine instrumentation. Hook-and-rod constructs remain a primary means of reconstruction for patients with primary or metastatic tumors of the spine. These systems can also be blended with pedicle screws for hybrid constructs.2 Primary spinal cord and spinal canal tumors typically undergo extensive posterior element bony exposure. This can lead to a significant enough loss of the posterior tension band that kyphosis or instability results.3 Restoration of the tension band and stability are ideally achieved by a posterior construct. Metastatic disease can involve both the anterior and posterior columns. Anterior disease is more common, and reconstruction typically involves work to reestablish support in the anterior column. Posterior tension band reconstruction is also commonly needed to decrease stress on the anterior construct that can result in graft subsidence and pain. The need for anterior and posterior resection and reconstruction in patients with malignancy is becoming better recognized and in some series approaches 60% of patients with metastatic spine disease.4–6 Although pedicle screws are increasingly utilized alone or blended with hooks in hybrid constructs, hooks have some distinct advantages. Pedicle screws are stronger than hooks in most circumstances, but the reverse may be true in osteoporotic bone.7,8 Screw purchase may also be inferior to that of hooks in regions where disease has partially eroded a vertebral body but where fixation is desirable. Hooks also have the advantage of surgeon familiarity and ease of placement. Furthermore, hooks come in a variety of shapes, forms, and insertion sites that make them extremely versatile. This chapter discusses the technical details and options available for hook-and-rod reconstruction of the thoracic and lumbar spine for both primary and metastatic disease. All hooks have common components, including the blade, throat, shank, and connector (Fig 39-1). The blade and the throat are the parts of the hook that capture and purchase the spine. The blade comes in a variety of shapes to engage different components of the posterior elements of the spine. The throat can have different opening sizes to accommodate different spans of bone while allowing a snug fit. This is important to prevent migration of the hook into the spinal canal. The shank and connector can be of different sizes and heights to allow flexibility when making the connection to the rod. Offsets can also be built into the hook shank to provide even more flexibility for connection. The connector provides the region for rod capture. This is the most variable aspect of the hook. Virtually all systems have a unique connector. Despite the uniqueness of design between available hook-rod connectors, they all have one of three patterns. The rod can connect to the hook by loading from the top, side, or via a goalpost like a three-point shear clamp. FIGURE 39-1 Offset hook demonstrating the basic components of the blade, throat, shank, and connector. (A) Lateral view. (B) Front view. There are four basic hook choices (Fig 39-2): infralaminar, supralamina, pedicle, and transverse process. We discuss each of these hooks, focusing on their specific advantages, disadvantages, regions of use, indications, and contraindications. The infralaminar hook is placed beneath the lamina with the blade running from caudal to cephalad. It is inserted by dissecting the ligamentum flavum from the lamina surface. The ligamentum can be left in place or removed. Partial or complete removal is recommended to decrease mass in the spinal canal. The lamina is often squared off with a bur. The hook blade is then seated beneath the lamina with the throat size chosen to fit snugly around the lamina (Fig 39-3). This snug fit is important to minimize hook migration into the spinal canal as well as to optimally apply mechanical forces to the spine.9,10 Infralaminar hooks have the advantage of ease of insertion and strength. Ease of insertion is due to the shingled contour of the caudal aspect of the lamina. The blade follows this contour naturally into position. This is the strongest hook from a mechanical perspective due to the dense cortical bone of the lamina and the surface area of contact between the blade and the lamina.11 Infralaminar hooks typically have a neutral contour between the blade, throat, and shank. The blade is typically flat and broad, although narrow profiles are available. These hooks can be utilized at virtually any level of the spine where segmental fixation is required. FIGURE 39-2 Four basic hook choices. From left to right: infralaminar hook, supralamina hook, pedicle hook, and transverse process hook. (A) Lateral view. (B) Front view. FIGURE 39-3 Infralaminar hook inserted. (A) Top view. (B) Side view. The disadvantages of infralaminar hooks result primarily from their physical mass in the canal. This can result in focal stenosis, especially if bilateral hooks are used. Although this is rarely a problem in non-stenotic lumbar spines, it is a potential issue in the thoracic spine. These hooks are contraindicated in congenitally narrow canals such as those seen in achondroplasia, or those with acquired narrowing. Another disadvantage of a hook blade inside the canal is the possibility of hook migration. This is particularly true if there is not a tight fit of the throat to the lamina. This can lead to spinal cord compression and damage. Care must be taken in any manipulation of the hook to avoid migration. We typically keep a hook holder on the hook to maintain control during manipulation such as rod insertion to the hook. The loss of integrity of the posterior ligament structures, in particular the ligamentum flavum, is also a disadvantage of this type of hook. This loss of ligament support can lead to junctional kyphosis.10,12 The supralamina hook is placed from the superior edge of the lamina with the blade pointing caudally. It is inserted by drilling a level insertion site along the superior edge of the lamina. A small amount of bone is removed from the lamina cephalad of the intended hook site to minimize canal compromise during insertion. The ligamentum flavum is also removed to ease insertion. The hook blade typically has a ramped throat to match the angle of the lamina (Fig 39-4). In this way, the throat will fit more snugly to the lamina. An infralaminar hook in this position would be partially forced into the canal by the mismatch between the linear throat of the hook and the sloped contour of the lamina. A supralamina hook can be placed at virtually any level of the spine. This hook is typically used opposite an infralaminar hook placed at a more caudal level to allow compression of a spinal segment or graft. It can also be used as the cephalad component of a claw construct to reduce the risk of rod dislodgment. It has the advantage of strength similar to that of an infralaminar hook. The supralamina hook also matches the infralaminar hook well in the coronal plane, easing rod attachment. Supralamina hooks share the same disadvantages as infralaminar hooks. These include the risk of migration into the canal, spinal cord injury on insertion, and loss of the ligamentum flavum’s contribution to the posterior tension band. The pedicle hook is utilized to gain spinal purchase between the levels of T3 and T10. It is typically not possible to utilize this hook above or below these levels due to the anatomy of the pedicle, facets, and foramen. Therefore, the pedicle hook is widely used in the thoracic spine where both the canal and pedicles are narrow. It reduces or eliminates the hook in the canal relative to lamina hooks. The pedicle hook is structurally weaker than lamina hooks. It is the second strongest hook available.11
Posterior Thoracic and Lumbar Hook-Rod Instrumentation
 Hook Choices
Hook Choices

Infralaminar Hook
Supralamina Hook
Pedicle Hook

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree