Postlaminectomy Kyphosis
John M. Rhee
BIOMECHANICS AND ETIOLOGY OF POSTLAMINECTOMY KYPHOSIS
The normal cervical weight-bearing axis in the sagittal plane begins at the occipital condyles and should fall dorsal to the vertebrae of C2-C7 (1) (Fig. 87.1). A proper sagittal vertical axis helps maintain a lordotic alignment to the cervical spine, which averages 14 degrees, and places 36% of loads through the anterior column versus 64% through the posterior column (2). In this way, the biomechanical demands on the dorsal neck musculature are reduced and balanced by the favorable alignment.
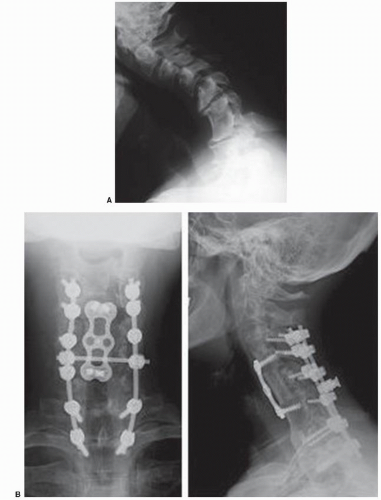
Cervical laminectomy can lead to kyphosis by altering this biomechanical balance in several ways. First, the approach involves a dissection of the cervical extensor musculature, which can lead to denervation, fibrosis, or atrophy, making the muscles less capable of performing their normal duties. The muscles can be placed at further disadvantage if the attachments of the semispinalis cervicis and capitis, the primary extensor muscles of the neck and head, have been removed from C2. Second, cervical laminectomy involves the removal of some of the dorsal soft tissue restraints that can act as a tension band, such as the supraspinous ligament, ligamentum flavum, facet capsules, and interspinalis muscles. Third, excessive facet resection can contribute to instability and kyphosis. Cadaveric sectioning studies have demonstrated that instability is prone to develop when more than 50% of a facet joint has been removed. The postlaminectomy kyphosis that occurs in the setting of aggressive facetectomy may be particularly severe due to the combination of kyphosis and spondylolisthesis that arises (Fig. 87.2).
These negative biomechanical factors then lead to a vicious cycle of kyphosis (Fig. 87.3). As the head translates ventrally, the sagittal vertical axis moves ventrally, causing additional compressive loads on the anterior column and tensile loads on the posterior column, further compromising the mechanical disadvantage introduced by laminectomy on the dorsal extensor muscles. The dorsal ligamentous restraints are then also put under further tension, additionally limiting their ability to act as tension bands. As a result of the kyphotic deformity, the spinal cord may be draped over the kyphos resulting in mechanical compression against the ventral vertebral bodies and contributing to impairment in spinal cord vascularity.
Dorsal compression of the spinal cord may also result from postlaminectomy kyphosis due to the formation of postlaminectomy membranes that can compress the dura in extension (3). Because of this biomechanical cycle, it is imperative to avoid performing laminectomy without fusion if the cervical spine already demonstrates loss of lordosis preoperatively, as the dorsal structures in this scenario begin at a disadvantage and are likely to be at further disadvantage after laminectomy.
CLINICAL PRESENTATION
Many patients who develop postlaminectomy kyphosis have initial improvement in their presenting neurologic symptoms after surgery. However, as the deforming forces progress and kyphosis develops, they may complain of axial neck pain due to muscle fatigue. Typically, these symptoms are mechanical and demonstrate a reasonable degree of relief at rest. As the deformity progresses, myelopathy and/or radiculopathy can recur. In the most severe situations, kyphosis can lead to loss of forward gaze, difficulty swallowing and eating, poor ventral skin hygiene, and the need to prop up the neck with the hands (Fig. 87.4).
INCIDENCE AND EPIDEMIOLOGY
The reported incidence of postlaminectomy kyphosis varies widely. Mikawa et al. (4) reported that 52% of patients demonstrated change in cervical alignment after multilevel laminectomy, with 14% developing kyphosis. Guigui et al. (5) noted that 31% had a change in alignment versus preoperative, with 25% having increased kyphosis. While the true incidence of postlaminectomy kyphosis is unclear, it does appear to be more common in children than adults. Possible reasons for the difference include the effects of spinal growth in the setting of disrupted dorsal stabilizing structures (6), negative effects of radiation therapy given to children who undergo laminectomy for tumors, or the relative lack of spondylosis and stabilizing osteophytes in children compared with adults. Accordingly, Kato et al. (7) found that multilevel laminectomies for ossification of the posterior longitudinal ligament (OPLL) led to a change in alignment in 47% of patients, but no neurologic worsening,
potentially due in part to the self-stabilizing effect of OPLL, especially if it bridges across motion segments.
potentially due in part to the self-stabilizing effect of OPLL, especially if it bridges across motion segments.
 Figure 87.1. Sagittal vertical axis. A normal sagittal vertical axis describes a plumb line from the occipital condyles, which should fall dorsal to the C2-C7 vertebrae and typically through T1. |
Risk factors for the development of postlaminectomy kyphosis include preexisting lack of lordosis, younger age at time of surgery, laminectomy of four or more levels, surgery involving the C2 lamina, performance of facetectomies, and increased preoperative range of motion (5,8). Although laminoplasty was initially designed in order to prevent the development of postlaminectomy kyphosis, some loss of lordosis also occurs with laminoplasty (Fig. 87.5). In general, however, the loss of lordosis after laminoplasty tends to be less than that seen after laminectomy and much less commonly of clinical significance in the properly chosen patient. Suk et al. (9) reported on average 5 degrees loss of lordosis after laminoplasty, with 10.6% of patients developing an average of 12 degrees of kyphosis. As one would predict, those who began with less lordosis (<10 degrees preoperative) were more likely to develop kyphosis, as were those demonstrating more global flexion than extension on preoperative dynamic radiographs. Loss of lordosis with laminoplasty may be lessened by sparing C2. Takeshita et al. (10) found that the decrease in lordosis from C2-C7 was 8.3 degrees if C2 was split during laminoplasty, 5.2 degrees with a dome-like laminotomy of C2, but only 1.5 degrees if C2 was left completely intact.
SURGICAL STRATEGIES FOR CORRECTION
Patients with postlaminectomy kyphosis may have significant pain as well as functional and neurologic impairment. Nonoperative treatments such as physical therapy for extensor muscle strengthening may be sufficient in mild cases of kyphosis but is unlikely to be of major benefit in those with significant kyphosis. In symptomatic patients with significant kyphosis, a surgical approach is generally required, particularly if there is myelopathy. Goals of treatment include (a) correction and fusion of deformity, ideally with a normalized sagittal vertical axis; (b) neurologic decompression; and (c) pain relief. A generalized algorithm for surgical management is presented in Figure 87.6.
FLEXIBLE AND PASSIVELY CORRECTABLE KYPHOSIS
If the deformity is flexible and passively correctable, then it may be reduced into the desired alignment and fused either ventrally and dorsally. Ventral-only surgery has several advantages (Table 87.1). Ventral surgery can allow for the direct decompression of a spinal cord draped over a kyphos, avoids reoperation through a scarred approach dorsally, preserves the dorsal musculature, which has already been compromised, and provides height restoration to the anterior column through the use of structural interbody or corpectomy grafts. However, disadvantages of ventral-only surgery include relatively less secure fixation in the vertebral bodies versus the dorsal elements (especially in osteopenic patients), and the inability of ventral plates to restore the dorsal tension band. Although ventral plates may “hold” the correction achieved through the placement of interbody grafts, they are at a relative mechanical disadvantage secondary to their action being ventral to the axis of rotation of the kyphotic deformity.
Dorsal-only surgery can also be considered in this scenario of a flexible and passively correctable kyphosis. A prerequisite of dorsal-only surgery is that sufficient spinal cord decompression can be achieved through realignment and restoration of lordosis in those with neurologic compression. In such patients, as well as those with no neurologic compression, dorsal surgery has the advantage of generally superior fixation versus ventral plates, particularly at the ends of the construct, where pedicle screws can be routinely placed into C2, C7, and the upper thoracic spine. In addition, dorsal implants are at a mechanical advantage in correcting kyphosis in that they act dorsal to the axis of rotation of the kyphotic deformity. However, dorsal surgery also has disadvantages, including the need for a revision approach through scar with no dural protection due to previous laminectomy, further denervation and damage to the dorsal musculature, more perioperative pain than is typically encountered with a ventral approach, higher wound infection rates, and relatively poor, limited surface areas for bone grafting and fusion.
Although ventral- or dorsal-only surgery can generally be utilized in those with flexible deformities, other factors should be taken into consideration. In those with poor bone quality or who need a long segment fusion, a ventral approach alone may be insufficient as the screw fixation
achieved in the vertebral bodies via ventral cervical plates may not be enough to counteract the deforming forces. In such cases, significant subsidence of the interbody grafts into soft end plates may occur as the spine settles back into its original kyphotic alignment. Furthermore, if a multilevel corpectomy is needed for neurologic decompression in the setting of postlaminectomy kyphosis, high rates of failure can be anticipated with ventral-only surgery due to the severe instability that develops from disconnecting the two sides of the spine with the corpectomy ventrally and the laminectomy dorsally (11). If bone quality is adequate and the goals of surgery can be accomplished with discectomies or short segment combination corpectomydiscectomy rather than long corpectomies, ventral-only surgery may be adequate. Otherwise, a combined ventraldorsal approach is more likely to result in favorable outcomes. In addition, in cases in which the sagittal vertical axis cannot be restored, consideration should be given to maximal fixation, since major deforming forces will be still be present.
achieved in the vertebral bodies via ventral cervical plates may not be enough to counteract the deforming forces. In such cases, significant subsidence of the interbody grafts into soft end plates may occur as the spine settles back into its original kyphotic alignment. Furthermore, if a multilevel corpectomy is needed for neurologic decompression in the setting of postlaminectomy kyphosis, high rates of failure can be anticipated with ventral-only surgery due to the severe instability that develops from disconnecting the two sides of the spine with the corpectomy ventrally and the laminectomy dorsally (11). If bone quality is adequate and the goals of surgery can be accomplished with discectomies or short segment combination corpectomydiscectomy rather than long corpectomies, ventral-only surgery may be adequate. Otherwise, a combined ventraldorsal approach is more likely to result in favorable outcomes. In addition, in cases in which the sagittal vertical axis cannot be restored, consideration should be given to maximal fixation, since major deforming forces will be still be present.
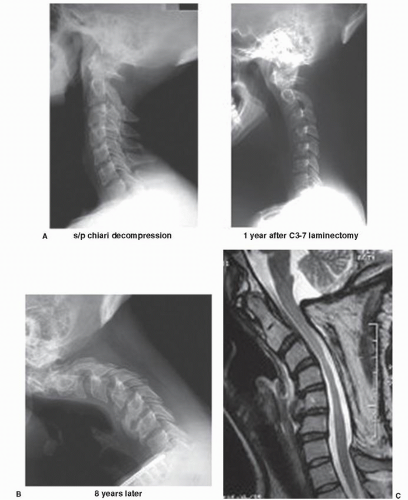 Figure 87.3. Progressive postlaminectomy kyphosis. A: A 38-year-old woman who initially underwent suboccipital craniectomy and C1-C2 laminectomy for Chiari malformation. B: One-year status post C3-C7 laminectomy for persistent headaches, demonstrating early kyphotic change. C: Eight years later, marked kyphosis has developed. Note the iatrogenic spondylolisthesis at C3-C4 and C4-C5. D: MRI demonstrates draping of the spinal cord primarily at C3-C4 with myelomalacia.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|