CHAPTER 41 Postoperative Infections of the Spine
Postoperative infections in patients undergoing spine surgery are unfortunate complications that significantly contribute to patient morbidity. Although infection in the general spine surgery population is relatively infrequent, with rates between 1% and 5.4% usually being reported,1–7 specific subpopulations, such as trauma or cancer patients, may have much higher infection rates.4,8–10 The cost of treating postoperative infections was estimated at $100,000 per patient in 1996 in the United States,11 but it is difficult to estimate the physical and social impact on the patient, who may be subjected to repeat washout and revision procedures and prolonged courses of intravenous antibiotic treatment. Modern surgical techniques, antisepsis, and antibiotic prophylaxis have made significant inroads into the problem of postoperative infection, but surgeons must be continually vigilant for this complication. Familiarity with current state-of-the art diagnostic tests, imaging evaluation, and treatment methods is essential.
Incidence
Noninstrumented Spinal Procedures
Lumbar diskectomy is one of the most common spinal procedures and is associated with highly successful clinical outcomes.12 Fortunately, these procedures have an extremely low rate of infection, with most large series reporting an incidence of 1% or less.13,14 Newer series of endoscopic minimally invasive diskectomy have achieved even lower rates of infection,15,16 with one study reporting no infections in the treatment of 262 patients.16 Infections after lumbar disk surgery can be manifested as superficial wound infections or as diskitis, with increasing back pain 2 weeks to several months postoperatively in conjunction with fever and laboratory and radiographic abnormalities.
Patients undergoing laminectomy without fusion may also enjoy a low incidence of infection, although slightly higher than that for patients undergoing diskectomy alone. Infection rates of approximately 2% are commonly reported in the literature for this procedure.17 Laminoplasty techniques have been associated with a higher rate of infection and are probably more appropriately considered instrumented procedures because most involve the placement of some type of implant.18
Noninstrumented posterior spinal fusion is associated with a higher rate of infection than is simple laminectomy or lumbar diskectomy,4,19 a factor attributable to longer operating times, more blood loss, greater soft tissue destruction, and placement of devascularized allograft.
Although most noninstrumented spinal surgeries involve a posterior approach, anterior cervical diskectomy and fusion procedures can be and often are performed without instrumentation, especially when only a single level is treated. Infection rates for the anterior cervical approach, however, are extremely low with and without the use of instrumention,20 thus making it difficult to discern any real difference between these two groups.
Finally, relatively limited interventional procedures such as chemonucleolysis and diskography are associated with an infection rate of up to 4% in the absence of preoperative antibiotics. Fortunately, this incidence can be dramatically decreased with the use of prophylactic antibiotics.21–24
Instrumented Spinal Procedures
The use of instrumentation in posterior spinal procedures increases the incidence of postoperative infection to approximately 3% to 7% in most series.2,25–28 Spinal instrumentation increases the risk for infection by acting as a locus minoris resistentiae for organisms rather than as a source of inoculation.29 In fact, one study demonstrated that 11 of 21 patients undergoing hardware removal for noninfectious reasons had positive bacterial growth on cultures.30 Although most infections occur in the immediate postoperative period, there are multiple reports of delayed infections occurring years after surgery.31–34 It is thus likely that colonization of implants is commonplace and that clinical infection occurs either when bacteria are sufficiently pathogenic or when host factors predispose to infection.
The type of instrumentation may affect the probability of clinical infection. Older steel implants tend to be uniquely implicated in the development of late spinal infections.34 Corrosion and fretting at cross-connector sites have been associated with foreign body reactions and the development of a local environment favorable for the growth of endogenous or low-virulence bacteria.32,34–36 This has not been reported with newer titanium implants, which are resistant to corrosion and thought to be relatively bacteria resistant.
Anterior instrumented spine surgeries are associated with extremely low rates of infection; when infections do occur, they tend to be superficial.20,37–39 The low incidence of infections with the anterior approach is probably attributable to the use of avascular planes in dissections and minimization of soft tissue trauma and necrosis. Although the anterior approach itself is associated with a low risk for infection, the highest rates of infection are encountered with combined anterior and posterior approaches to the spine,40 a finding probably attributable to the greater length and complexity of these cases.
An emerging category of spine surgery is minimally invasive surgery. The goal of minimally invasive spine surgery is to minimize soft tissue trauma and blood loss and thereby hasten patient recovery and decrease the risk for infection. Although several authors have realized good results with minimally invasive techniques,41,42 most series are small and no reduction in wound infection rates has been conclusively demonstrated.43 Further experience with these techniques will clarify the exact extent of the reduced infection risk with these methods.
Finally, the implantation of intrathecal drug delivery systems and spinal cord stimulators is associated with an approximately 5% risk for infection.44,45 Infection with these devices occurs in the pump or stimulator pocket in most cases, although infection of the intraspinal component can lead to meningitis or epidural abscess.44–46 These infections tend to occur early, usually within the first 2 postoperative months.
Infection Risk Factors
Although the type of surgery plays a large role in determining a patient’s risk for infection, numerous patient-, surgery-, and disease-specific factors have been elucidated (Table 41-1).
TABLE 41-1 Risk Factors for Infection
| TYPE OF FACTOR | CONDITION | INCREASED RISK |
|---|---|---|
| Patient specific | Age | >20 years |
| Diabetes mellitus | Glucose intolerance | |
| Malnutrition | Albumin <3.5 mg/dL Total lymphocyte count <1500/mL | |
| Obesity | ||
| Alcoholism | ||
| Tobacco use | ||
| Urinary/fecal incontinence | ||
| Disease specific | Immunocompromised state | Steroid use Rheumatoid disease |
| Malignancy | ||
| Trauma | Spinal cord injury | |
| Surgery specific | Posterior approaches | Staged anterior-posterior procedures |
| Length of surgery | >5 hr | |
| Number of levels | ||
| Estimated blood loss | >1 L Blood transfusion | |
| Postoperative stay in an intensive care unit | ||
| Preoperative hospital stay |
Patient Factors
Important among patient factors are medical comorbid conditions, including increasing age, obesity, diabetes, poor nutritional status, and alcohol and tobacco use.6,40,47–50 Other factors associated with an increased risk for postoperative infection include steroid use, rheumatoid disease, and an immunocompromised state.40,51,52
Obesity is a frequent comorbidity in the spine surgery population. Several studies have demonstrated an increased risk for infections in obese patients undergoing spine surgery.40,49,51,53,54 Obese patients are subject to longer operative times; greater amounts of retraction, which, in turn, causes increased soft tissue necrosis; greater amounts of poorly vascularized fatty tissue with decreased oxygen tension; decreased immune defense in adipose tissue; and poor tissue concentrations of prophylactic antibiotics.29,55–57 Finally, obesity predisposes the patient to diabetes.
Malnutrition is a well-known factor that predisposes patients to infection. It has been demonstrated to impair immune response and wound healing. Klein and coauthors reported that 25% of patients undergoing elective lumbar surgery had positive indices of malnutrition and that 11 of 13 infections occurred in these patients.47 Other authors have also reported a high rate of infection in malnourished patients undergoing spine surgery,58 as well as the development of malnutrition in some spine surgery patients during their hospital stay, a particular concern for those undergoing staged procedures.59 Commonly used indices of malnutrition are serum albumin level and the total lymphocyte count, with values of less than 3.5 mg/dL and 1500/mL, respectively, being considered abnormal.60 Other indices, including skinfold thickness, transferrin levels, arm muscle circumference, and weight-height ratio, can also be used to assess nutritional status.61 Malnutrition may be associated with malignancy and trauma, two conditions known to be related to high rates of infection.
Diabetes impairs wound healing and predisposes to wound infection in spine and other surgeries.6,40,62–64 Postoperative wound infections have been reported to occur in up to 24% of diabetic patients undergoing spine surgery.40,63 Proposed mechanisms by which diabetes contributes to infection risk include increased glucose concentrations in wound fluids, the presence of dysfunctional polymorphonuclear neutrophils and macrophages, impaired lymphocyte chemotaxis, and delayed wound re-epithelialization.65–68 Impaired glucose tolerance without overt diabetes has additionally been correlated with this complication in the spine.6,51 Although studies of deep sternal surgical site infection in cardiothoracic procedures have demonstrated an ability to reduce this risk with strict perioperative glucose control, such a study in the spine is lacking.69,70
Tobacco use has been demonstrated to be a risk factor for wound infection in several studies.71–73 Hypothesized mechanisms include deprivation of oxygen to tissues and impaired wound healing and neutrophil defense.74–76
Surgical Factors
Several surgical variables other than those discussed earlier have been identified that may predispose patients to infection. Many of these variables appear to correlate with the magnitude of the surgery itself. It is therefore not surprising that the number of levels treated, length of the surgery, procedural complexity, and amount of blood loss have all been associated with an elevated risk for infection.2,25,49,62,77,78 Operative times longer than 5 hours have been associated with an increased rate of infection, as has blood loss of 1000 mL.62,77
The use of a cell saver system has been inconsistently correlated with infection risk. Although blood that has been processed by the cell saver system has been shown to be contaminated in 37% of various surgical procedures, no contamination was found in neurosurgical procedures.79 Additionally, even though use of the cell saver system was correlated with infection in series of spinal patients,31 no increased risk has been noted in other specialties.80 The use of blood transfusion, however, has been correlated with infection in numerous studies, and this risk may be independent of the amount of blood loss.31,80,81
Other surgical risk factors include revision surgery, the use of allograft material, and surgery extending to the sacral region, the latter of which may be attributable to urine and fecal contamination.25,82,83 Finally, the presence of two or more resident surgeons being involved in the procedure has been correlated with increased infectious risk in one study.51 Although not completely explored, this variable may be a reflection of the length and complexity of the procedure rather than a truly independent risk factor.
Disease-Specific Factors
Infection risk has repeatedly been demonstrated as significantly altered by the disease state of the patient. The presence of malignancy appears to be associated with the highest incidence of infection, reported to be higher than 20% in some series.4,8 This rate has been reported to be even higher in patients undergoing radiation therapy in conjunction with open surgery.84–87 The high rate of postoperative infection in this population is probably multifactorial, however, with poor nutritional status, the long and complex surgical procedures necessary for spine reconstruction, and use of adjunctive therapies such as corticosteroids all contributing to the dramatically elevated risk for infection.
Traumatic spinal injury is also associated with a significantly higher risk for infection, especially in the presence of a complete neurological injury.9,10 Again, the elevated risk in this group may be multifactorial, with prolonged stay in the intensive care unit, urinary or fecal incontinence, and large procedures all playing a role.6
Prolonged presurgical hospitalization and postoperative stay in the intensive care unit are also risk factors for wound infection. Blam and associates reported that patients staying in the intensive care unit for more than 1 day had a 6- to 13-fold greater risk for postoperative infection than did patients who did not stay in the intensive care unit.9 Wimmer and coworkers showed that extensive presurgical hospital stay was significantly associated with infection.62
Clinical Findings
The signs and symptoms of spinal infection depend on whether the infection is superficial or deep. Superficial infections occur above the lumbodorsal fascia in the dermis and subcutaneous tissue and are usually manifested in the immediate postoperative period as erythema, purulent drainage, and local tenderness. Patients may have low-grade fever, and laboratory evaluation may reveal elevated erythrocyte sedimentation rate (ESR), elevated C-reactive protein (CRP) level, and leukocytosis. The presence of these indices is variable, however. For example, Levi and coauthors reported an average temperature of 37.5° C and a white blood cell (WBC) count of 10.2 × 106 cells/mL in 17 patients with postoperative infections.2 If the wound is open or purulence is expressible, Gram stain and cultures are often useful in revealing the pathogen and targeting treatment (Fig. 41-1).
Deep infections have a much more variable manifestation. They may develop in the immediate postoperative period, with some authors reporting most occurring 2 to 3 weeks postoperatively, or in a significantly delayed fashion several months to several years after surgery.32,34 Patients with an acute manifestation are often symptomatic with significant pain, fever, anorexia, and night sweats. The wound overlying a deep infection can appear completely normal or, if the infection tracks superficially, can be purulent. Patients with a delayed manifestation often have increasing back pain, wound drainage, and erythema but may lack fever altogether.34,88
Spinal epidural abscess is a rare complication of spine surgery that may occur in an acute or delayed fashion and cause increased back pain, fever, and neurological deficit.89,90 Patients with spinal epidural abscess may have a rapid neurological decline, and the presence of any neurological deficit should raise concern for this process.91
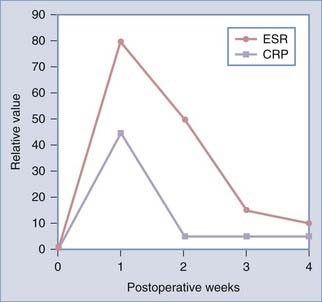
Evaluation
Both laboratory evaluation and imaging are important in the assessment of postoperative spine infections. Laboratory evaluation should include a WBC count, ESR, CRP levels, and cultures and Gram staining if there is purulent drainage or an open wound. The WBC evaluation may be and often is normal, especially in patients with a delayed manifestation, but it can useful if elevated.88,92 The ESR is reliably elevated in the setting of infection, but a high ESR can be difficult to interpret in the immediate postoperative period. ESR values normally rise to a maximal value of 102 mm/hr after spine fusion surgery and 75 mm/hr after disk surgery on postoperative day 4 before declining to normal levels 2 to 4 weeks postoperatively.92 Patients with infection have persistently elevated ESRs, usually more than 2 SD greater than the mean.92 Infections with low-grade pathogens such as Propionibacter may, however, be associated with low or normal ESR values.93 Obtaining serial ESRs can additionally be useful in tracking the response to treatment of infection. CRP values may be of added benefit in the diagnosis of infection, as well as in monitoring treatment response. A normal elevation of CRP is also seen in the immediate postoperative period; however, this elevation is more rapid and returns to baseline more quickly than does the rise in ESR, although complete normalization may take up to 2 weeks (Fig. 41-2).94,95 Additionally, CRP values are elevated more frequently than ESRs in the setting of infection with low-grade pathogens.93
Accurate diagnosis of bacterial pathogens is critical in the treatment of postoperative infections. Antibiotic therapy should be withheld until after specimens are taken for Gram staining and culture. These specimens are easily obtained from draining or open wounds, but care should be taken to prepare the skin carefully before specimen collection to prevent being misled by normal skin flora. If débridement is planned, specimens should be taken from both superficial and deep parts of the wound. Blood cultures can aid in the diagnosis of a pathogen when obtaining a direct specimen is difficult. Alternatively, computed tomography (CT)-guided or open biopsy of infected tissue may be helpful, with a diagnosis being obtained more than 50% of the time.96–98
Imaging Diagnosis
Plain Radiographs and Computed Tomography
Plain radiographs are useful in the assessment of spine alignment, local soft tissue reaction to infection, and bony response to infection but have limited utility in the immediate postoperative period. Early bony changes in response to infection are manifested approximately 2 to 3 weeks postoperatively by evidence of disk space narrowing, bony destruction, and blurring of end plates. These findings may be followed by vertebral body collapse or sclerosis of end plates and bony ankylosis in the more chronic setting (Fig. 41-3).99 Increased swelling noted in soft tissues, especially in the retropharyngeal space after anterior spine surgery, may indicate the presence of an abscess. Finally, plain radiographs are useful for evaluation of the integrity of spine hardware, with lucency around screws being associated with loosening and failure.
CT imaging reveals a sequence of bony changes similar to that seen in radiographs but provides improved anatomic detail and can better detect paraspinal masses and epidural collections.99 When performed with contrast enhancement, CT can accurately delineate the presence of an abscess and provide a useful aid in surgical planning or can be used to guide percutaneous biopsy of infected bone or soft tissues.100 CT myelography may be useful in aiding the diagnosis of epidural or subdural empyema when magnetic resonance imaging (MRI) is unavailable or contraindicated.101
Nuclear Imaging
Technetium 99m–labeled methylene diphosphonate bone scans can be used to help diagnose and localize an infection, but this technique suffers from limited sensitivity and specificity given that other conditions, such as trauma, tumor, or vascular insult, may have increased uptake and that uptake may be negative in photopenic areas where there is decreased blood flow or bone tissue.99,102 A three-phase bone scan may increase the sensitivity and specificity of this test.103 An indium 111– or technetium 99m–labeled leukocyte scan may help in diagnosing infection in settings where other factors, such as fracture, may cause false-positive results on bone scanning.103,104
Recent experience with 18F-fluorodeoxyglucose positron emission tomography (PET) shows some promise, with the major caveat being the inability to differentiate tumor from infection.105,106 PET may be particularly useful in the postoperative setting, however, where a negative PET scan can rule out infection.107
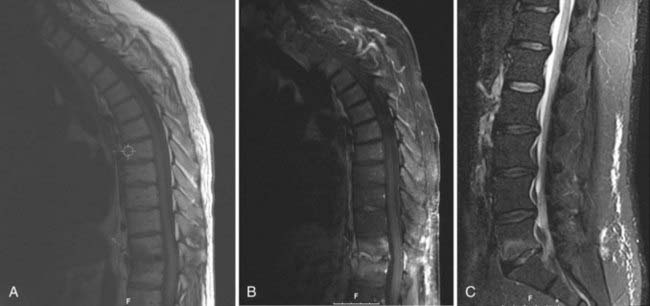
Magnetic Resonance Imaging
MRI is the imaging modality of choice when evaluating spine infections and enjoys a sensitivity and specificity of approximately 95% in the diagnosis of various spine infections, including osteomyelitis.108–110 Early MRI findings in the setting of infection include bone marrow edema signal manifested as hypointensity on T1-weighted sequences and hyperintensity on T2/STIR (short tau inversion recovery) signals.110,111 Although these findings are somewhat nonspecific, the observation of end-plate erosion with loss of the low signal intensity line, disk space narrowing, and disk space hyperintensity on T2-weighted sequences dramatically increases the sensitivity for infections.112 Loss of the normal low-intensity disk space cleft on T2-weighted sequences is another clue to the presence of infection.99 The addition of contrast enhancement is useful in confirming the presence of infection, delineating the extent of infection, and differentiating infection from solid granulation tissue, with the latter most often having a homogeneous pattern of enhancement (Fig. 41-4).111–114 Finally, MRI is also useful in detecting the presence of soft tissue masses associated with infection, such as paraspinal or epidural abscesses. Identification of such an associated mass increases the likelihood of infection being present to 98%.112
Some of these MRI findings, including vertebral body edema signal and contrast enhancement, may be present in the postoperative setting in the absence of infection.115,116 The presence of an adjacent soft tissue mass in this setting, however, strongly supports the diagnosis of infection. Moreover, absence of the MRI findings just listed strongly correlates with the absence of infection.116
Bacteriology
Skin flora are the most common causative organisms in postoperative spine infection, with staphylococcal species, particularly Staphylococcus aureus, being the most frequently detected.2,27,52,117 Methicillin-resistant S. aureus (MRSA), gram-negative organisms, and mixed flora are detected in sufficient frequency, however, to recommend withholding antibiotics until adequate culture specimens have been obtained and then providing treatment with broad-spectrum antibiotics until the culture results are available. Delayed infections are most frequently caused by bacteria of low virulence, with Propionibacterium and Staphylococcus epidermidis being common offenders.34,93,118 Isolation of Propionibacterium in culture specimens can take up to a week, and recent reports indicate that this bacterium might play a role in acute infections as well.93
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree