Preventing Complications of Cervical Spine Surgery
Glenn R. Rechtine II
Christian P. DiPaola
PREVENTING COMPLICATIONS OF CERVICAL SPINE SURGERY
Prevention of surgical complications does not begin at the preoperative visit. Prevention should be an ongoing process with every patient encounter. Encouraging healthy lifestyle changes can make a huge difference in short- and long-term outcomes of surgery. Many of the diseases spine surgeons treat surgically are either caused or aggravated by lifestyle issues. Deconditioning, smoking, and malnutrition are contributory to spine symptoms and affect recovery from surgery. They also can and should be modified in order to optimize surgical results.
DIABETES
Diabetes is one of the most significant risk factors for surgical complications and poor outcomes (1,2). Delaying surgery to allow for better control can be of benefit in elective surgery. Analysis of the HgA1c can tell how well the patient has been under control (3,4). Tight control of perioperative glucose levels improves outcomes, shortens length of stay, and dramatically decreases wound infections (5,6). Therefore, aggressive management of blood sugars throughout the surgical experience is imperative for reducing the risks of infection and other complications.
SMOKING CESSATION
Smoking and nicotine abuse are major risk factors also. Smoking cessation is associated with improved outcomes and lower complication rates. A minimum of four nicotine-free weeks will reduce the risks of soft tissue healing complications (7,8), and 1 to 2 months of smoking cessation will reduce the risks of pulmonary complications and mortality in the perioperative period (9,10). In an experimental human model, smoking cessation for at least 4 weeks reduced the risk of surgical infections (11). Zdeblick showed decreased lumbar fusion rates in smokers that persisted even after smoking cessation (12). In a randomized trial, the overall complication rate in smokers was reduced from 52% to 18% by a preoperative smoking cessation intervention. Wound-related problems, cardiovascular complications, and secondary surgery were dramatically reduced (13,14).
Smoking cessation is most likely to occur within the first two office visits with a spine practitioner (15). The counseling and education should begin with the initial visit and continue with each subsequent visit. A consistent and nonconfrontational approach to educate the patients about the negative effect of tobacco on their spinal condition has a dramatic effect on cessation rates (16). As many as 40% of smokers will quit with appropriate help from the spine practitioner (15).
CALCIUM AND VITAMIN D
Optimizing bone health with calcium and vitamin D supplements is necessary to maximize bone healing. Currently, 40% of all Americans and a billion people worldwide are vitamin D deficient. The vitamin D deficiency is expressed as increased rates of heart disease, multiple sclerosis, prostate, breast, and colon cancer, as well as osteomalacia. The 400 IU contained in our multiple vitamins is the current recommended daily allowance (RDA). However, it is inadequate to maintain appropriate vitamin D levels. A study on young healthy subjects showed the minimum daily intake should be at least 1,200 to 1,500 IU in order to maintain minimum levels of vitamin D (17). In young healthy individuals given 1,000 units daily for 3 months, the serum level of 25-hydroxyvitamin D did not reach an average of 30. For preoperative patients, a prescription for 12 doses of 50,000 units of vitamin D2 over a 6-to-12-week perioperative time frame will help to ensure blood levels adequate for healing. At that point, it is recommended to have at least 1,000mg of calcium citrate with vitamin D, a multivitamin, and 1,000 units of vitamin D3 indefinitely. For older patients and those with osteoporosis, this becomes 1,500 mg of calcium citrate with vitamin D and 2,000 units of vitamin D3. The risk of toxicity is very low, the laboratory test for vitamin D has become much more cost-effective, and the supplements are inexpensive ($22.00 for the total of 12 doses of
50,000 units). The Centers for Medicare and Medicaid Services recognizes advising calcium and vitamin D intake as one of the 80 clinical practices that should be advocated for all patients. Counseling was included in the 2007 physician quality reporting initiative (18). This practice can result in higher Medicare reimbursements for physicians. This means it has been established as an expected practice protocol with evidence-based documentation. Only a minority of spine surgeons currently assess or address calcium and vitamin D levels, even in high-risk patients (19).
50,000 units). The Centers for Medicare and Medicaid Services recognizes advising calcium and vitamin D intake as one of the 80 clinical practices that should be advocated for all patients. Counseling was included in the 2007 physician quality reporting initiative (18). This practice can result in higher Medicare reimbursements for physicians. This means it has been established as an expected practice protocol with evidence-based documentation. Only a minority of spine surgeons currently assess or address calcium and vitamin D levels, even in high-risk patients (19).
Vitamin D deficiency impacts a large portion of the world’s population. In July 2007, an article by Holick (20) proclaimed that over a billion people worldwide were vitamin D deficient. Malnutrition exists even in our young medical professionals: Fifty-seven percent of resident physicians were noted to be vitamin D deficient, and 40% had laboratory confirmation of secondary hyperparathyroidism (21). The problem is getting worse with time. The levels of vitamin D in the American population decreased in surveys done in 2000 to 2004 compared to 1988 to 1994 (22). There are populations that are at higher risk. These include the elderly, diabetics, and dark-pigmented individuals (20). This racial difference may represent as much as a third of the excess risk of peripheral vascular disease among Black Americans (23). Vitamin D deficiency is associated with increased all-cause mortality (24). How does that impact the practice of spine surgery? The obvious answer is the effect on bone metabolism and lack of calcium absorption. In extreme forms, vitamin D deficiency will result in a reactive hyperparathyroidism and osteomalacia. Bone healing will be strongly impaired. This will be evidenced as slow or absent fracture and fusion healing.
In addition, vitamin D deficiency is associated with increased pain from multiple musculoskeletal sources including low back pain. Vitamin D also has a beneficial effect on the neuromuscular junction. Low levels of vitamin D are associated with increased risks of falls. In adolescents, muscle function as measured by jump velocity, jump height, power, and force were all improved by correcting vitamin D deficiency (25). Other nonspine effects of vitamin D deficiency are increased risks of breast, prostate, and colon cancer; heart disease; autoimmune disease; asthma; peripheral vascular disease; diabetes; obesity; and multiple sclerosis (20,26, 27, 28, 29, 30 and 31). Chronic widespread pain has psychological and emotional components. The association is higher in women with low vitamin D levels (26). Myalgias and nonspecific muscle pains can be improved in 90% of vitamin D-deficient patients by correcting the deficiency (27).
Even in adolescents, 15% are vitamin D deficient to a degree that puts them at risk for secondary hyperparathyroidism (28). Our usual diets are not sufficient. The only other sources for vitamin D are sunlight and supplements. Even in areas of the world with blazing sun exposures, vitamin D deficiencies exist. The prevalence of vitamin D deficiency in Qatari children, for example, was 68% (29).
CALCIUM SUPPLEMENTATION
Patients should be instructed to take calcium supplements unless there is a specific medical reason not to. The most common calcium preparation is calcium carbonate,
CaCO3. It is known as both oyster shell or coral calcium and found in over-the-counter preparations such as Tums, or Caltrate. Calcium carbonate requires a highly acidic environment for absorption. Any patient taking proton pump inhibitors or antacids for gastroesophageal reflux disease or ulcer symptoms will not absorb the calcium carbonate. As one ages, there is less stomach acid. Therefore, patients over 70 years of age will not benefit from calcium carbonate. As it requires acid, taking calcium carbonate with a meal, especially a high-fiber or fatty meal, diminishes the effectiveness of the supplement.
Calcium citrate is a much better preparation for many reasons: (a) It does not require acid for absorption; (b) it is less likely to cause constipation, gas, and abdominal discomfort; (c) it can be taken with food of any kind; and (c) kidney stones are less likely to occur. Dosing becomes a problem because the labels uniformly list the serving size as two tablets, which is missed by most consumers. As a result, they take half of the intended dose.
VITAMIN D SUPPLEMENTATION
Nutrition should be addressed at each visit. All patients should be encouraged to take calcium and vitamin D supplements. Some patients feel they do not need to take supplements because they drink milk. However, a study showed no significant difference in serum vitamin D levels in those who drank milk regularly and those who never drank milk (30).
Ninety-two percent of statin-treated patients with vitamin D deficiency had resolution of myalgias with vitamin D supplementation (31). Case reports and small case series have also described improvement in chronic back pain by correcting vitamin D deficiency (32). Correcting vitamin D deficiency also results in increased strength (33).
Something as simple as vitamin D supplementation can have a dramatic effect on costs. Overall health care costs were 39% higher in patients who were vitamin D deficient (34). Another study estimates the cost savings by optimizing vitamin D levels in Western Europe at greater than $200 billion per year if the mean 25-hydroxyvitamin D level is elevated to 40 ng/mL (35).
The 400 IU of vitamin D listed as the current RDA is inadequate. It takes a minimum of 1,500 IU per day to reliably obtain minimal blood levels (17). In the past, we have been reluctant to recommend higher amounts of vitamin D for fear of toxicity. These fears are not substantiated by the data. In order to reach toxic levels, it would require long-standing doses of at least 40,000 units per day. No reported cases of toxicity have involved less than 10,000 units a day for extended periods of time (36). One study looked at using a single dose of 300,000 units of vitamin D in elderly patients instead of 800 units per day. The vitamin D serum levels were higher in the first group even 3 months later (37). Obviously, this would require redosing at regular intervals.
PREHABILITATION
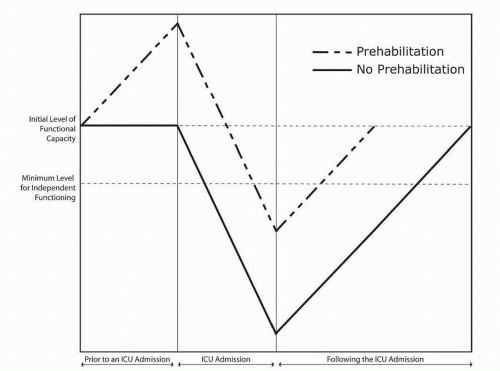
Active exercise and prehabilitation are very effective techniques for minimizing symptoms from the typical
degenerative spine conditions (see Fig. 153.1). The patient who is better conditioned also recovers from surgery faster with fewer medical complications. These benefits are demonstrated in all age groups, including elderly patients (38). Age is not a contraindication to prehabilitation (39). The program should involve a progressive aerobic training, strength training, and flexibility (40). This is another lifestyle issue that should be encouraged at each and every visit. Nielsen et al. (41) showed that lumbar fusion patients had shorter hospital stays, achieved their postoperative goals faster, and returned to work sooner using fewer resources if they had been involved in a prehabilitation program.
degenerative spine conditions (see Fig. 153.1). The patient who is better conditioned also recovers from surgery faster with fewer medical complications. These benefits are demonstrated in all age groups, including elderly patients (38). Age is not a contraindication to prehabilitation (39). The program should involve a progressive aerobic training, strength training, and flexibility (40). This is another lifestyle issue that should be encouraged at each and every visit. Nielsen et al. (41) showed that lumbar fusion patients had shorter hospital stays, achieved their postoperative goals faster, and returned to work sooner using fewer resources if they had been involved in a prehabilitation program.
CARDIAC EVALUATION
Preparation for surgery should be a team event involving the surgeon and the other practitioners involved in the patient’s care. The internist or primary care physician can help with risk stratification. Evaluation of cardiac, pulmonary, and renal issues should be done prior to the pre-op visit. Stress tests have poor predictive value as a preoperative assessment tool. There are no data to suggest benefit from percutaneous coronary intervention or coronary bypass procedures in reducing noncardiac surgical risks.
The requirement for anticoagulants after angioplasty and stenting can increase the risk of perioperative bleeding, especially with spinal surgery (42). Patients who are taking Plavix and Coumadin for medical conditions will require careful presurgical assessment. If the medications can be discontinued safely in the perioperative period, this should be done. Cervical surgery has a significant risk for epidural hematoma and neurologic compromise, especially if the patient is receiving anticoagulants at the time. An assessment must be made as to the absolute necessity for these medications. If they cannot be temporarily stopped during the perioperative period, performing the surgery may not be prudent, depending on the overall risk-benefit evaluation. As with each and every surgery, the potential benefits to the patient are offset by risks involved with the surgery.
PREVENTION FACTORS FOR INFECTION
Olsen et al. (2,43) showed the risk factors for surgical site infections in spinal surgery to be diabetes, elevated perioperative glucose levels (whether diagnosed as diabetic or not), suboptimal timing and dosing of prophylactic antibiotics, postoperative incontinence, dorsal approach, surgery for tumor resection, and morbid obesity. In a pediatric spine population, Linam showed similar risk factors
involving obesity, the use of clindamycin as the prophylactic antibiotic, and inappropriately low doses of antibiotics. What is somewhat disconcerting is that in the infected and control groups, over 90% received antibiotics for greater than 24 hours, 70% to 75% had incorrect redosing, and 40% to 54% had incorrect timing of the antibiotic. Certainly, the antibiotic timing and dosing as well as maintaining appropriate perioperative glucose levels are within the control of the surgeon. These should be protocol-driven patient care pathways because they have been shown to effectively reduce incidence of infection (44).
involving obesity, the use of clindamycin as the prophylactic antibiotic, and inappropriately low doses of antibiotics. What is somewhat disconcerting is that in the infected and control groups, over 90% received antibiotics for greater than 24 hours, 70% to 75% had incorrect redosing, and 40% to 54% had incorrect timing of the antibiotic. Certainly, the antibiotic timing and dosing as well as maintaining appropriate perioperative glucose levels are within the control of the surgeon. These should be protocol-driven patient care pathways because they have been shown to effectively reduce incidence of infection (44).
APPROPRIATE ANTIBIOTIC TIMING AND DOSING
The centers for disease control and prevention (CDC) recommendations have been to give prophylactic antibiotics within 1 hour of incision and to continue them for no more than 24 hours (45). The presence of a drain is not an indication to prolong the antibiotic regime, even though that had been a tradition with no basis. The use of a first-generation cephalosporin is highly recommended if there are no medical contraindications. The cephalosporin should be redosed if the surgery is longer than 4 hours or if the blood loss exceeds 1,500 mL. Vancomycin should be reserved for those cases in which the patient has a known methicillinresistant exposure or contamination. For patients with antibiotic allergies, other medications are indicated. Kanayama et al. reported in the Journal of Neurosurgery Spine a series of 1,600 consecutive spine surgery patients. They compared the CDC guideline to the previous practice of multiple days of antibiotics. The infection rate was cut in half form 0.8% to 0.4%. This did not reach statistical significance; however, the interesting findings were the specific infecting microbiota. Infections in the multiple-day antibiotic group were caused by resistant strains in 83% of the cases. None of the CDC group infections were caused by resistant organisms (46).
In order to minimize the risk of infection, all incidental infection sources should be aggressively evaluated and treated before proceeding to surgery. Open wounds, especially in a diabetic, should be healed before proceeding with elective surgery. Urinary tract and upper respiratory infections should also be cleared with a healthy interval prior to surgery to minimize the risks of infections, postanesthesia respiratory problems, and resistant organisms.
Meta-analysis has not demonstrated a benefit in infection reduction by the use of presurgical antiseptic showers, even though they decrease skin colony counts (47).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree