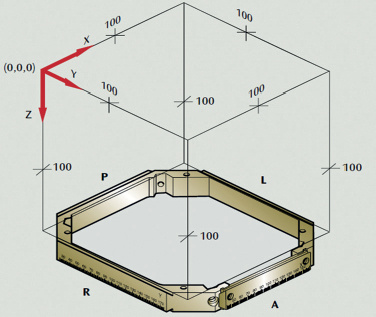
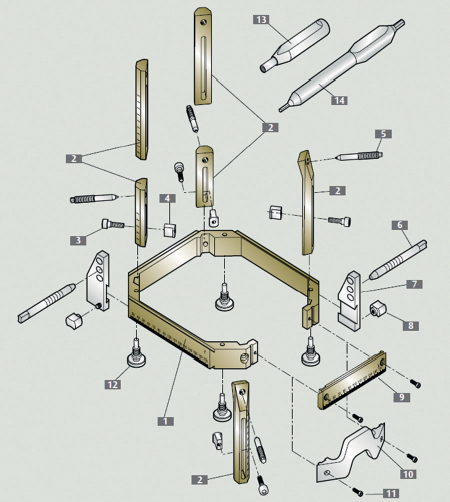
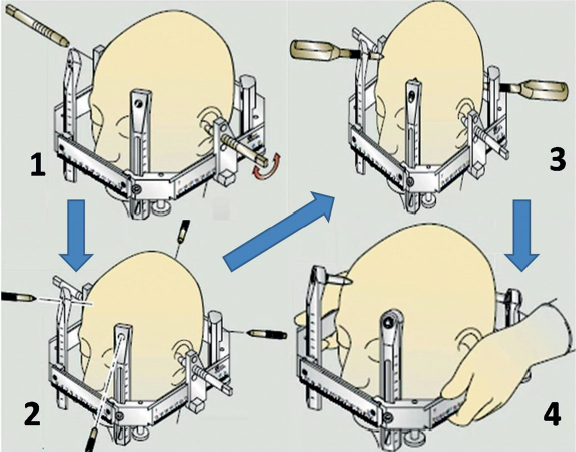
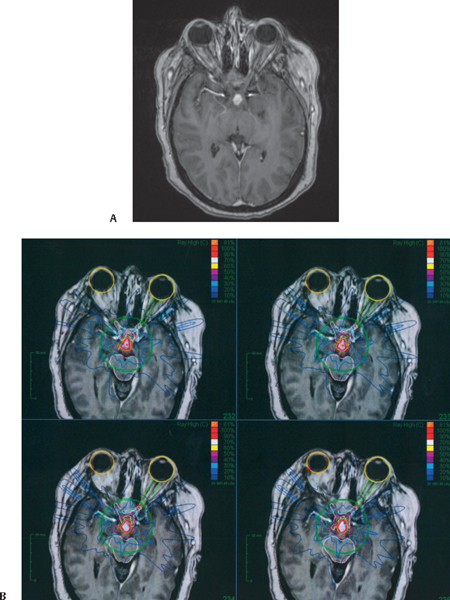
39 What are the basic steps to stereotactic radiation delivery? 1. Application of the frame or some other form of immobilization to the skull 2. CT/MR/angiographic imaging with frame and localizer attached 3. Merging of other imaging modalities (e.g., PET, previously obtained MRI, etc.) 4. Treatment planning a. Outline of target of interest and other important structures to be avoided (typically performed by the neurosurgeon) b. Dosimetry and analysis (completed by the physicist and radiation oncologist) 5. Patient positioning 6. Delivery of radiation 7. Postradiation care (steroids, follow-up, and scheduled imaging) What does frame fixation achieve? A constant geometrical relationship between the frame and the target anatomy What frame is used in GKS? The Leksell frame • Origo (Latin) = origin • It’s the point where all the coordinates (X, Y, and Z) have a zero value. • For the Leksell frame, the point is located superoposterior and lateral on the patient’s right side. • In imaging (typically axial CT or MRI scan), the point is on the very top of the inferior left corner fiducial • Medial to lateral is defined by X. • Anterior to posterior is defined by Y. • The Z-axis is calculated by the position of the oblique rod of the reference frame on an axial image relative to the vertical rods (i.e., supero-inferior or rostrocaudal) Fig. 39.1 Drawing of Leksell frame for Gamma Knife™ SRS. (Courtesy of Elekta™ AB, Norcross, GA.) Why is this important, especially when using GKS? If the frame is not placed so that the lesion is as close as possible to the center of the “Leksell space,” the frame can collide with the collimator, resulting in greater imaging distortion.1 What are the components of the Leksell stereotactic frame? 1. Frame base 2. Fixation posts 3. Locking screws (5 × 19 mm) 4. Locking pieces 5. Fixation screws 6. Earplugs 7. Earplug holders 8. Knob for ear plug holder 9. Straight front piece 10. Curved front piece 11. Securing screw, 4 × 10 mm 12. Connection feet 13. Socket wrench 14. Screwdriver Fig. 39.2 Drawing of individual parts of Leksell G-frame for Gamma Knife™ SRS. (Courtesy of Elekta™ AB, Norcross, GA.) How do you put on a stereotactic frame? 1. With the frame over the patient’s head, the assistant holds the anterior portion of the frame with the index finger. Place the frame in the appropriate alignment to the patient’s skull. This may be done with use of the earplug holder center or inferior hole; place the earplug and gently lock it in the external auditory meatus by gently rotating it. 2. Select the screw length anteriorly and posteriorly and apply local anesthetic through the pinholes. Insert the screws in opposite diagonals and finger-tighten them until they touch the scalp. Some prefer to place the posterior screws first. 3. Then use the socket wrench and tighten the screws a quarter of a turn. Do the same for the other diagonal. Repeat tightening the diagonal screw pairs alternately, a quarter turn at a time, until the frame is secure. 4. Remove earplugs if used. Check firm attachment of the frame by holding it and gently attempting to lift it. Fig. 39.3 Placement of Leksell G-frame for Gamma Knife™ SRS. (Courtesy of Elekta™ AB, Norcross, GA.) Why does the frame need to be attached to the table during imaging and treatment? To ensure orthogonal alignment and rigid stabilization of the frame Where is the center coordinate in the Leksell frame? X = 100 mm Y = 100 mm Z = 100 mm How can you determine the center point from an axial image obtained with the frame on? By drawing two diagonal lines from each corner (fiducial point) of the frame The Z coordinate can be calculated: it is the distance from the ipsilateral fiducial to the diagonal coordinate + 40 mm.1 What substance fills the fiducials in the localizer placed on the frame? Copper-Sulfate (CuSO4) solution. Remember to check the localizer first as sometimes the fiducials have not been refilled in time and they can be degraded and not seen after the MRI has already been done. What other frames exist (typically used for stereotactic brain biopsies, and not GKS)? • BRW: Brown-Robert-Wells (historical interest) • CRW: Cosman-Robert-Wells2 • Patil • Zamorano-Dujovni What are some limitations of the BRW frame? Difficult access to posterior fossa lesions What are some of the improvements found in the CRW? MRI-compatible frames and easier arc-frame applications that allow access to posterior fossa lesions1 What is a phantom frame? A device used to test the accuracy of the target. This is present in the CRW and BRW systems. This phantom frame and base can be sterilized prior to using it.2 To what does the word registration refer? The method through which we define a correlation in space between a point in the patient and the same point on imaging studies obtained for that purpose What imaging study is typically used for target selection? • CT: more accuracy • MRI: more anatomical definition; typically a contrast-enhanced T1 sequence is the method used for localization. FLAIR sequences are also useful. • Sometimes it is possible to fuse both CT and MRI, obtaining the advantages of both. • Integrating MRI or CT with angiograms for the treatment of AVMs is also possible, augmenting the accuracy of the treatment plan. Why is CT more accurate than MRI when planning targets for SRS? Unlike CT images, MR images are susceptible to spatial distortions (particularly at the peripheral edges of the images obtained). Causes of these distortions include3: • Inhomogeneities of the magnetic field • A nonlinearity gradient field • Linear scale error • Instrument imperfections • Magnetic susceptibility artifacts • Local magnetization effects How much distortion would you expect with MRI when using, say, a Leksell frame? An in vitro study of cadaver heads found ±2 mm accuracy when using MRI for target planning with a Leksell frame.4 Who participates in the target selection process? The neurosurgeon, assisted by the physicist and radiation oncologist True or false: Not all the fiducials need to be visible in the study performed preprocedure. True. All fiducials do not need to be seen for the study to be accurate and used for stereotactic imaging, though it is preferred to have all fiducials visualized. What are the typical doses used in SRS? Benign tumors: 10 to 20 Gy (margin dose) AVMs: 18 to 25 Gy (margin dose) Metastasis: 16 to 22 Gy (margin dose) Pituitary: 12 to 30 Gy (margin dose) Trigeminal neuralgia: 70 to 80 Gy (maximal dose) What is the target-volume ratio (i.e., the conformality index)? The relation between the prescribed dose and how it adapts to the target boundaries • Ideally this relationship should be 1:1. What is the efficacy of SRS for treating meningioma? Overall disease stabilization rates of 89%5 What is the efficacy of SRS for treating vestibular schwannoma? 91.1% according to meta-analysis5 What kinds of local control rates may be achieved using SRS for patients with brain metastases? 59.6 to 96.8%5 How long can a patient diagnosed with glioblastoma expect to live after conventional treatment plus nonfractionated SRS, and what percent of such cases have complications? 13.5 to 26 months; 11.4% of those patients experienced complications5 How effective is SRS in the management of a cerebral arteriovenous malformation? 72 to 96% obliteration for small AVMs (≤3 mL).6–8 The risk of bleeding after SRS is not changed until the AVM is completely obliterated (which may take as long as 5 years post-SRS, especially in new experimental techniques for larger lesions).9 What is the physiological theory behind SRS management of AVMs? Radiation may multiply endothelial cells in the vessels, which increases clot formation, which decreases blood flow in the nidus. Is SRS or fractionated SRT considered more efficacious in controlling acoustic neuroma growth? SRS and SRT are equally efficacious; both offer excellent control of acoustic neuroma (approximately 95%)10–12 Which system and mode best preserve hearing in SRS therapy of acoustic neuromas? One study showed that SRT yielded significantly higher hearing preservation, but it was not a randomized trial, so it is difficult to say if there is a significant difference.10 Another study showed an increase in trigeminal neuropathy after SRS but no significant difference in hearing outcomes in SRS vs. SRT.11 What is the most common side effect from SRS? Late radiation necrosis, usually at 6 months to 2 years postexposure. It can include focal deficits, seizures, and intracranial hypertension. CT may show low-density white matter change as well as the white matter edema seen on MRI.13 What are some other complications of SRS? • Alopecia • Scalp damage ranging from erythema to necrosis • Cranial nerve injury • Cataracts • Cerebral damage (edema or necrosis) • Cyst formation • Radiation-induced neoplasia or transformation13 What structures need to be excluded/avoided when performing SRS? Brainstem Optic apparatus: Optic nerves/chiasm Lens Pituitary gland Auditory apparatus Spinal cord What are the maximal doses that these structures can tolerate? Brainstem (10–12 Gy) Optic apparatus: Optic nerves/chiasm (10–12 Gy) Lens Pituitary gland (approximately 20 Gy) Auditory apparatus (cochlea <6 Gy, cerebellopontine angle <12–13 Gy) Spinal cord (10 Gy; thecal sac max dose 14 Gy)14,15 Fig. 39.4 (A) T1-weighted MRI with contrast of a 40-year-old woman with a diagnosis of metastatic plasma cell granuloma with metastasis to the brain; a 1.5-cm lesion is shown behind the optic chiasm. (B) Cyberknife™ planning MRI showing target lesion of interest highlighted in red as well as critical anatomy also delineated including the brainstem and both globes as well as optic nerve and chiasm. The colored lines surrounding the targets represent the isodose lines of the treatment.
Radiosurgical Techniques
39.1 Procedure Pearls and Frame Placement
39.2 Preprocedure Planning
39.3 Clinical Application Concepts
39.4 Postprocedure Complications and Management
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






