Chapter 80 Recurrent Lumbar Disc Herniation
Lumbar discectomy represents the most commonly performed spinal surgical procedure.1 Approximately 300,000 lumbar discectomy procedures are performed each year in the United States.2 In general, the clinical outcome for this procedure is favorable, with 80% to 90% of patients undergoing surgery reporting good or excellent results.3–6
Despite these favorable results, a relatively small number of patients who have had an initial good outcome following surgery will redevelop symptoms similar to those of their preoperative state owing to a recurrence of herniated disc material at the previous surgical site. The reported incidence of these recurrent lumbar disc herniations ranges from 5% to 15%.7–11
The patient with a symptomatic recurrent disc herniation typically undergoes several weeks or months of conservative management. This treatment may be followed by surgical reexploration in those individuals whose symptoms remain unresponsive. Surgery may involve simply removing the reherniated disc material or a fusion and fixation across the affected disc space. Regardless of the management approach, a recurrent disc herniation creates a substantial economic impact.12 This impact is compounded by time lost from work and the need for many of these patients to be retrained for lighter-duty positions.
Risk Factors for Recurrent Disc Herniations
The risk factors for a primary disc herniation have been noted to include exposure to repetitive lifting, exposure to vibrations, smoking, and a constitutional weakness of the anular tissue.13–15 Isolated trauma or injury has not been found to be a consistent risk factor, occurring in only 0.2% to 10.7% of adults with a herniation.14,16 Conversely, Cinotti et al. found that 42% of patients with a recurrent disc herniation related the onset of radicular pain to an isolated injury or precipitating event.17 Similarly, Suk et al. reported the rate of an isolated injury as a cause of recurrence in 32.1%. This study also noted that 71.4% of the patients with recurrence were males and 57.1% were smokers.18
Despite these findings, other studies have found that gender, age, smoking status, level of herniation, and duration of symptoms were generally not associated with higher rates of recurrence.8,9,17–19 Additionally, the degree of anular incision and the extent of the discectomy (partial or complete) have not been found to affect the potential for recurrence. 9,17–19
One factor that potentially increases the likelihood of a recurrent disc herniation is diabetes. In general, patients with diabetes have been noted to have lower clinical success rates following the initial lumbar discectomy than do nondiabetic patients. Simpson et al. reported an excellent to good outcome following the initial discectomy of 95% in nondiabetic patients but only 39% in diabetic patients.20 Mobbs et al. reported success rates of 86% in nondiabetic patients and 60% in diabetic patients.9 Although these clinical outcome differences were generally felt to be attributable to lower quality-of-life indicators in diabetic patients, Robinson et al. investigated the differences in the proteoglycan profile of the discs in the two groups. This study found that diabetic patients had fewer proteoglycans in the disc material, potentially increasing their susceptibility to recurrent disc prolapse.21
Another proposed risk factor is the configuration of the initial disc herniation. Suk et al. and Grane et al. noted that preoperative disc configuration does not affect the rate of recurrence.18,22 Alternatively, Carragee et al. prospectively evaluated herniated disc configurations along with the rate of reherniation and the rate of reoperation. Disc herniations were divided into four shaped-based groups: (1) fragment-fissure herniations (disc fragment and small anular defect), (2) fragment-defect herniations (large disc fragment with massive dorsal anular tear), (3) fragment-contained discs (incomplete anular tear), and (4) absence of fragment-contained herniations (anular prolapse). Of the four groups, the fragment-fissure type herniations (group 1) were associated with the best outcomes and the lowest rate of reherniation (1%) and required the fewest reoperative procedures (1%). Those with anular prolapse (group 4) were associated with poorer clinical outcomes, with 38% of patients experiencing recurrent or persistent symptoms.8
Evaluation of Recurrent Disc Herniation
The patient who presents with a recurrent disc herniation has generally had a period of clinical improvement following the initial discectomy procedure. A retrospective review of 28 patients with recurrent disc herniation found a pain-free interval ranging from 7 to 168 months (mean of 60.8 months).18 Patients typically report radicular signs and symptoms similar or identical to those of their preoperative clinical state.
Pathologic changes in the ventral epidural space may reflect mass effect due to perineural scarring or recurrent disc herniation.7,23 Scarring is most pronounced before 9 months and primarily involves the anulus fibrosus.24 The scar may surround the nerve roots and cause symptoms by means of neural tension, decreased axoplasmic transport, restriction of blood flow, or restriction of venous return.7
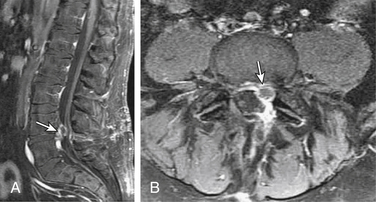
MRI, with and without gadolinium contrast, is the preferred imaging modality for the assessment of a recurrent disc herniation.7,10,25,26 The use of contrast material helps to differentiate normal postoperative anatomic changes from a recurrent herniation. Peridural scarring will typically enhance heterogeneously because of its vascular supply. A recurrent disc herniation usually appears as a polypoid mass with a low signal on T1- and T2-weighted sequences. It is usually contiguous with the parent disc unless sequestered. There can be a hypointense rim of the posterior longitudinal ligament and outer anular fibers that outline the herniation. This rim will enhance with contrast administration (Fig. 80-1). The disc itself will not enhance, because it has no blood supply.7,27
MRI findings will vary according to the time period during which the study is obtained relative to the primary procedure. In the early (1- to 6-month) postoperative period, MRI demonstrates a high-intensity signal band extending from the nucleus pulposus to the site of anular disruption. This is particularly noticeable in the first 2 months following surgery. The anulus is typically hyperintense, and the nucleus is typically hypointense. There is loss of disc space height. The end plates and marrow will frequently have a low signal on T1-weighted images and a high signal on T2-weighted images, suggesting inflammation and edema. The ventral epidural space initially reveals an increase in soft tissue mass, evidence of tissue disruption, edema, and hemorrhage, with the appearance of mass effect.10
Nerve root enhancement with gadolinium in the first few months following surgery is normal. This typically indicates a breakdown of the blood-nerve barrier but usually resolves within 6 months. Postoperative changes at the laminectomy site depend on the extent of surgery, the extent of ligamentum flavum removal, and whether a fat graft was placed in the epidural space. Facet joint enhancement occurs as a local response to dissection and persists long (>6 months) after surgery in more than half of the patients in whom imaging is performed.7,28,29
Late (>6 months) MRI findings include a low-intensity signal band in the disc space representing a healing anular defect. The mass effect that was seen earlier in the ventral epidural space may have resolved29 or may persist as a masslike scar.23 The laminotomy defect contains mature scar with peripheral enhancement identifying granulation tissue. Facet joint enhancement is visible after contrast administration in approximately half of the patients 6 months postoperatively.7
Retraction of the thecal sac toward a soft tissue lesion is suggestive of scar, while displacement away from such a mass is suggestive of a herniated disc.10 Although a pseudomeningocele may also be seen as a mass, its signal characteristics are different, demonstrating cerebrospinal fluid intensity on T1- and T2-weighted images and often an enhancing fibrous capsule.7
Despite the imaging advantages that MRI provides over other techniques, there can be a significant degree of discordance between MRI findings and intraoperative findings. This discordance can occur in 18% to 33% of cases that are proven surgically.30 As with the initial procedure, the successful outcome of any surgery for recurrent disc herniation depends on close correlation between the clinical and radiographic findings.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree