Case Report A2 Intervention to Promote the Functional Recovery of the More Involved Side with the Goal of Return to Work Stroke is a leading cause of disability in adults. Recent evidence with neural plasticity leads us to understand that, despite a neurological injury, there is plenty of potential for recovery following a stroke. The existing data of the last several decades provide significant evidence to support that the brain continuously changes its neural circuitry to encode new experiences and promote changes in behaviors.1,2 This research has been demonstrated in the healthy brain3,4,5 and has been expanded to demonstrate neuroplasticity in the injured brain.6,7 In both the healthy and the injured brain, research has demonstrated functional reorganization of the brain when an optimal environment is created for learning to occur. There is evidence indicating differences in how learning occurs in a healthy versus an injured brain.8 To promote rehabilitation, one must understand the principles required to promote learning in an injured brain. Understanding the principles supporting optimal experience-dependent plasticity guides clinicians in the rehabilitation of an individual with an injured brain. Some of these factors include concepts around promoting use of the affected limbs. Studies have demonstrated improvements in the functional use of the involved limb and activation of the motor cortex in the damaged brain when rehabilitative training was combined with constraint of the ipsilesional arm in humans.9,10,11,12,13 There is some suggestion that negative plastic changes occur if the individual continues to compensate and use only the less involved limbs.14 Over an extended period of time the neural circuits are not engaged in tasks the circuits begin to degrade.8 Rehabilitation strategies that promote the use of the involved limbs enhance neuroplasticity. Substantial evidence suggests that focusing on meaningful, functional tasks enhances neuroplasticity and thus recovery because the individual is more engaged.15,16 Richards et al17 noted “many clinical reports and motor learning–related findings indicate the best way to learn an activity is to practice that activity, which means task-specific training.” The constraint-induced movement therapy (CIMT) research suggests that upper extremity (UE) function in individuals after a stroke can improve when therapy involves intensive, task-specific training using activities that are challenging to the individual and relate to real-life scenarios.18 In Lennon and Ashburn’s study,19 therapists recognized that it was important to focus on movement components, such as alignment, transfer of weight, and pelvic tilt, within a functional task. These components of movement are required within many functional tasks. To work within a functional task with our clients who suffer from neurological injury, we need to understand the components of movements for a given functional task. We need to determine what prevents efficient task performance. Dean and Shepherd20 demonstrated that individuals poststroke who practiced seated reaching had improvements in their ability to reach, as well as increased loading through the involved foot and increased activation of leg muscles. Dean et al21 also found these improvements carried over to standing up. They concluded this was likely because there are similar biomechanical demands between reaching forward beyond arm’s length and standing up. Wu et al22 indicated that, when patients participated in reaching activities that were goal directed, there were improvements in the quality, accuracy, and efficiency of the reaching movement in the involved UE. Working within the functional task in all of the foregoing studies thus demonstrated improvements in the performance of the specific task, as well as increased activation in the involved UE and lower extremity (LE). In Ling and Fisher’s23 case report, the subject’s goal was to do his laundry at the community laundromat. To reach this goal, he needed to walk carrying the laundry basket and ascend and descend a curb. Based on this goal, they analyzed his movements and determined the specific system impairments that prevented him from achieving this goal. The intervention involved working within the task by breaking the larger task down into smaller subtask components. The specific subtasks practiced were chosen to address the specific impairments limiting him from obtaining his goal. Knowledge and skill in movement analysis allowed clinicians in the study to understand the sensory and movement demands of tasks. With this task-specific training, the therapists were able to assist this individual to make functional gains and achieve his goal. Although it is not always possible to practice within the exact task or within the exact environment the task is typically performed in, or to use the limb in the way it is typically used for the task with an individual who has minimal to no functional use of the involved UE, there are strategies to assist with task-specific training. As demonstrated in both Ling and Fisher23 and Davis,16 real-life tasks can be broken down into mini- or subtasks. Simulating the task as closely as possible by choosing intervention strategies that incorporate practice of the same or similar movement substrates/components, as well as setting the task and environment up in a certain way and choosing the most appropriate functional subtasks to be practiced, can address specific impairments and promote desired UE and LE movements and trunk control.16,23 Thus it is also critical to evaluate individuals poststroke within functional tasks to determine the specific single-system impairments that are contributing to the individual’s activity limitations and participation restrictions. Tasks that involve excessive effort can frequently cause overrecruitment of muscles and inefficient altered movement patterns.16 Ensuring an individual has an appropriate and stable base of support and an efficient alignment is essential to promoting UE and LE recovery.16,20 In addition, proximal stability can influence functional UE and LE outcomes.20,23 Based on these findings, using tasks, subtasks, and the appropriate environments that both match the ability of the body and limb movement and appropriately challenge within a functional context can help to promote improved UE movement patterns.16 Using either closed or modified chain tasks (see Chapter 9 on session intervention for further discussion of closed, modified, and open chain practice) can moderate the effects of gravity and the recruitment demands necessary for the limb movement. For example, stabilizing on a counter with the more involved hand while the other one reaches into the cupboard for a glass is an example of a closed chain use, and holding a cloth in the more involved hand and wiping a counter or holding a cup in the involved hand and sliding it up an inclined surface toward a higher cupboard are examples of modified chain movements for the UE. These concepts were also clinically applied by Ling and Fisher23 where closed and modified chain tasks were used to train proximal control. The subject in this study demonstrated improvement in both proximal and distal control. This work supports the idea of obtaining proximal control to promote more distal function of the UE. Research supports that individuals who suffer from stroke need practice and repetition to learn or relearn functional activities. The exact amount of repetition each individual requires to make functional improvements is unknown. In Wolf et al18 patients in the CIMT group received 6 hours of therapy per day over a 14-day period and demonstrated functional changes in motor recovery in the affected UE. Taub et al24 suggested that, when conventional physiotherapy is administered 6 hours a day for 10 consecutive days, there is an increase in arm use similar to that seen in CIMT therapy. The conclusion was that some individuals with subacute and chronic stroke changes/deficits could benefit from physiotherapy if they received multiple hours of motor skill practice per day. Our health care systems are not set up to provide 6 hours of therapy a day to each individual who suffers a stroke. Practicing skills outside of or beyond the therapy session is critical to help with skill acquisition.19 Therapists need to consider how clients will practice skills outside of the therapy session to achieve long-term and functional changes. There are many strategies to consider when working with individuals who suffer from stroke, including the volume of practice, incorporating the more involved limbs into the function, the neuroplasticity potential, and task/subtask practice that is meaningful and targets specific impairments. All these strategies can be applied toward the functional goals the individual has identified and the tasks chosen within these goals. Often in research and in clinical practice, the tendency is to use standardized measures to measure change. Examples of these include the Functional Independence Measure (FIM), Barthel Index, Chedoke McMaster Stroke Assessment (CMSA), Fugl–Meyer, Berg Balance Scale, grip strength, and passive and active range of motion. Using standardized measures is important in research and therapy practice, but using only standardized measures does not necessarily allow clinicians and researchers to capture change in tasks that are functional and meaningful to each individual. As evidenced in Ling and Fisher,23 standardized measures do not always detect functional changes nor do many of them consider the quality and efficiency of movement of individuals after a stroke. The importance of quality of movement when performing functional tasks, its contribution to efficient biomechanical function, and the magnitude of its contribution to functional recovery of the involved UE and LE are often overlooked.23 In the study by Ling and Fisher,23 no changes were noted in the Fugl–Meyer UE motor assessment or grip strength, yet the individual demonstrated changes in the use of his limbs, including his hand function, and he achieved his functional goal. These changes were demonstrated through the use of observational movement analysis as part of the pre- and posttesting assessments and as measurements to detect changes in function over time. This case report describes how the Neuro-Developmental Treatment (NDT) Practice Model can be used with a patient poststroke to guide clinical decisions about implementing physiotherapy and occupational therapy interventions that promote functional use of and recovery of the more involved side by incorporating the more involved limbs into the performance of functional tasks and assisting this individual to return to her participation roles. JW is a 51-year-old woman who sustained a large right parietal intraparenchymal hemorrhage with associated mass effect on September 21, 2009, resulting in left-sided hemiparesis. JW had a significant cardiac history, including mitral valve replacement in 2004, atrial fibrillation since she was 23 years old, aortic valve endocarditis, and a bicuspid aortic valve. She had no other known risk factors and was previously active. JW’s acute inpatient stay was complicated by treatment for the endocarditis, and as a result, she spent 6 weeks on an acute unit. JW was transferred to inpatient rehabilitation on November 2 and was discharged home on December 10, 2009. Prior to her stroke, JW had worked full time at a Canadian university as an information technology (IT) training and support coordinator. She engaged in activities of moderate intensity for at least 30 minutes on 5 or more days a week. Her interests included gardening and yard work, participating in Pilates classes, aerobics, canoeing, dragon boat racing, running, and regularly walking her dog. JW described a history of scoliosis but reported no physical symptoms associated with the condition. JW is married and lives in a multilevel home with her husband and their dog. At the time of her admission to this outpatient program, she was walking independently in her home using a rollator walker and relying on a wheelchair for outdoor mobility. She was ascending the stairs using a hand rail on the right and a step-to pattern, and she descended the stairs backward. JW was independent with all self-care activities but without using her left UE. JW initially used a handheld shower and sat on a shower chair in their walk-in shower. Prior to her stroke, she showered in a tub but was not able to negotiate the step into the tub safely after her stroke. JW dressed herself independently from a seated position and needed assistance to tie shoes and to manage buttons. She therefore avoided wearing pants and shirts with button enclosures. Tasks that required bilateral UE function, such as cooking, laundry, and housekeeping, were deferred to her husband and a hired housekeeper. JW was not able to work or drive and required transportation for outside appointments, grocery shopping, and entertainment purposes. JW’s expressed goals were to improve the use of her left upper extremity (LUE) for functional activities, such as stabilizing food objects so she could chop food for cooking, using her left hand to assist with folding laundry and dressing, and walking indoors and outdoors without relying on a walker or wheelchair. She wanted to return to work at the university and perform her specific job as soon as possible. To achieve this last goal, JW needed to be able to walk indoors and outdoors across campus in a timely manner to get to meetings at various locations. She also needed to ascend and descend stairs multiple times throughout her work day to get to her office and other campus buildings. JW would have frequent meetings during the day requiring her to don/doff a jacket multiple times, especially in the fall and winter months. Her job required her to multitask using the computer and phone simultaneously to support staff/students with IT issues. Because JW’s nondominant LUE was the more affected from her stroke, she needed her LUE to, at minimum, act as an active support to perform her responsibilities, but she was interested in eventually using her left hand to type as well. JW attended physical therapy and occupational therapy at our outpatient program (OP) two to three times a week beginning in December 2009. This case describes her intervention from December 2009 until September 2010. A significant life role for JW involved her career. She had worked at the university for more than 20 years and held a senior position in the IT department where she supervised several staff members. Her job required her to walk, travel across campus to other buildings for teaching purposes, ascend and descend stairs, type, carry teaching equipment during lectures, develop and give lectures and presentations, and support staff/students in various functions, including answering e-mails and phone calls, problem-solving computer issues, and instructing staff/students in using computer software. Prior to her injury, she had worked more than 60 hours a week. JW indicated she was passionate about her career and loved the challenge, responsibility, and high-paced environment of her position. Returning to her position at the university was her greatest goal. As such, the focus of this intervention was to help JW return to her position as soon as possible but with minimal accommodations. She was insistent that she would only return to work if it meant not compromising the gains she had already made and would potentially facilitate further gains in her function. There were many positive factors that would facilitate a successful transition back to her place of employment. JW was highly motivated and an active participant throughout her rehabilitation. She consistently transferred suggestions/recommendations from therapy into her home and community environments. Despite significant light touch and proprioception impairments in her left limbs, she readily incorporated her more involved extremities in all functional tasks. JW had an extensive support network, including her husband, family, friends, and colleagues, and her employer. She had no cognitive or visual perceptual system impairments. Her heart condition and scoliosis placed minimal restrictions on our interventions. In regard to her environment, JW was able to access therapy and the community using accessible transportation and family/friends. She was able to independently access her home environment with assistive devices. JW had the flexibility in her work environment to set up her space to ensure involvement of her more involved limbs. Her employer was accommodating in helping her return to work. The predominant environmental barriers were within her community. She required a hand rail on the right side to ascend and descend stairs. JW required physical assistance to access various places within her community secondary to curbs and doors. She walked slowly using a rollator walker and found it difficult to navigate in crowded environments. JW also required frequent standing or sitting rests due to fatigue. She could tolerate walking continuously for only 10-minute intervals. The university has a large campus with many students rushing to classes; thus there were concerns about her ability to safely ambulate in this environment. Table A2.1 JW’s most significant system impairments and activity limitations
A2.1 Introduction
A2.2 Case Description
A2.2.1 Examination and Evaluation
Facilitators—the Positives
Barriers
System impairments | Activity limitations |
• Inability to sustain activity in upper abdominals • Weakness of left hip extensors (primarily gluteus maximus) • Weakness of left knee extensors (primarily quadriceps) • Weakness of left knee flexors (hamstrings) • Weakness of left ankle dorsiflexors (tibialis anterior) • Tightness of shoulder internal rotators (primarily pectorals) • Inability to sustain activity in left scapular approximators (serratus anterior) • Inability to sustain activity in left scapular adductors (rhomboids) • Weakness of left scapular upward rotators (upper/lower trapezius, and serratus anterior) • Weakness of left shoulder external rotators • Inability to sustain activity in left elbow extensors (triceps) • Tightness of wrist flexors and long finger flexors • Weakness of left wrist extensors • Weakness of left finger extensors • Inability to initiate activity in left ankle evertors • Absent light touch and proprioception throughout left side • Decreased cardiovascular endurance | • Unable to use left upper extremity to stabilize vegetables to cut with right upper extremity • Unable to use left upper extremity to stabilize bowls and dishes when preparing meals • Unable to sweep, wash floors, clean high surfaces • Unable to put hair in ponytail or barrette • Unable to drive (i.e., manipulate the steering wheel and use controls for turn signal, operate windshield wipers) • Unable to carry grocery bags and get items out of wallet • Unable to type with left hand • Unable to talk on phone and make notes simultaneously • Unable to push/pull wheelbarrow for gardening/yard work • Unable to use paddle for rowing • Unable to carry laundry basket • Unable to walk dog • Unable to do Pilates or aerobics activities • Unable to open containers • Unable to run and go hiking • Unable to walk community distances in a timely way • Unable to walk at speeds to keep up with friends, family, peers • Unable to walk on uneven terrain |
Activity Limitations and Body System Impairments
At the time of this initial evaluation, JW presented with the following impairments and activity limitations as outlined in Table A2.1.
Outcomes and Outcome Measures
The following objective measures were used both as baseline measures and as outcome measures to demonstrate ongoing change. They were also related to JW’s impairments and identified functional goals.
Standardized Measures
1. Berg Balance Scale: The Berg Balance Scale was developed to measure balance among older people with impairment in balance function by their ability to perform various movement and functional tasks.25 Table A2.2 lists JW’s Berg Balance scores.
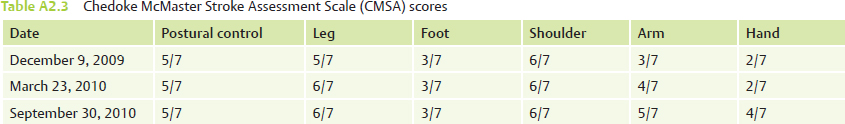
2. Chedoke McMaster Stroke Assessment Scale (CMSA): The CMSA is a 7-point scale that classifies motor recovery. The impairment inventory is used to classify the severity of physical impairments in individuals with stroke. It is divided into six dimensions, in which smaller scores indicate greater motor impairment.26,27 Table A2.3 lists JW’s CMSA scores.
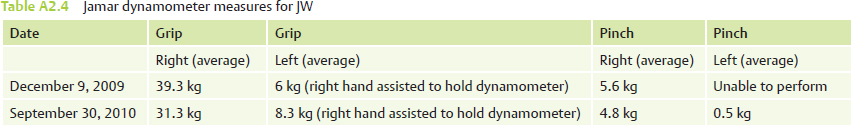
3. Grip/pinch strength: Grip and pinch strength were measured with the Jamar Hydraulic Hand Dynamometer (Patterson Medical Holdings, Inc.). Refer to Table A2.4 for JW’s Jamar dynamometer measures.
4. Two-Minute Walk Test: This test was conducted and timed in the hallway of the therapy area in our rehabilitation hospital. After each 33 m, JW had to turn 180° and walk in the opposite direction. Table A2.5 contains JW’s 2-Minute Walk Test results.
Table A2.2 JW’s Berg Balance Scale scores
Date | Score |
December 9, 2009 | 41/56 |
March 23, 2010 | 52/56 |
September 30, 2010 | 54/56 |
Table A2.5 Two-Minute Walk Test results for JW
Date | Distance traveled | Gait aid |
December 9, 2009 | 58 m | Single-point cane |
March 23, 2010 | 80 m | Single-point cane |
September 30, 2010 | 99 m | No aid |
Self-Referenced and Norm-Referenced Objective Functional Measures
Self-referenced measures, norm-referenced measures, and movement analysis were used to demonstrate changes in a selection of some of the functional activities that were required for JW to reach her goal of returning to work.
Observational Movement Analysis Descriptions
These movements were photographed and/or videotaped on three dates. The measures are outlined in the following six tables along with the observational movement analysis description for four of the tasks.
Putting on a Coat (Table A2.6)
December 9, 2009: The following describes how JW performed the task of putting on her coat. She completed this task sitting on a therapy mat, one-half femur length on the bed, feet hip width distance apart.
JW’s starting alignment is described as follows:
• Sits toward front edge of mat; one-half femur length on mat.
• Feet hip width distance apart.
• Hips slightly higher than knees.
Table A2.6 Time measures for putting on a coat
Date | Time | Time |
December 9, 2009 | 40 s | 100 s |
March 23, 2010 | 34 s | 59 s |
September 30, 2010 | 13 s | 32 s |
• Trunk in slight lumbar extension.
• LUE at her side in slight glenohumeral (GH) abduction, slight internal rotation.
• Right (R) hand grasping collar of jacket and holding it in front of LUE.
JW dons the left sleeve:
• L foot forward of R.
• Weight shifted more to R.
• Trunk in lumbar extension with thoracic flexion, cervical flexion looking at sleeve.
• R hand brings L sleeve to L arm, feeds left hand into sleeve, and slides sleeve up to shoulder with RUE.
• As slides sleeve up LUE, JW laterally side flexes in R lower trunk, pushing through RLE.
• LUE in 30° GH abduction, internal rotation, scapular abduction.
JW dons the right sleeve:
• Trunk rotated to the R with thoracic flexion, cervical flexion, and moving toward posterior pelvic tilt.
• Weight on R ischial tuberosity greater than L.
• L foot forward of R.
• RUE moved into GH extension and adduction, scapular adduction, downward rotation to grasp R sleeve behind her back.
• Once sleeve grasped, RUE then moves into GH abduction, external rotation and elbow extension to slide arm through sleeve.
• Trunk rotated back to midline, moves into posterior pelvic tilt, increased thoracic flexion.
• LUE positioned during this segment as follows:
 Scapular abduction and slight elevation.
Scapular abduction and slight elevation.
 GH abduction ~30°.
GH abduction ~30°.
 GH flexion ~20°.
GH flexion ~20°.
 GH internal rotation.
GH internal rotation.
 Elbow flexion ~110°.
Elbow flexion ~110°.
 Wrist flexion ~20° with fingers in slight flexion.
Wrist flexion ~20° with fingers in slight flexion.
• Cervical flexion, lateral trunk flexion on the L, increased thoracic flexion and posterior pelvic tilt.
• L foot forward, weight bearing primarily through RLE.
• L wrist and finger flexion used to grasp zipper with L arm stabilized by holding it against stomach.
• Once zipper started, L forearm placed across body to stabilize coat with wrist in flexion, forearm pronation, ulnar deviation, and fingers in flexion.
• Movement into neck extension and some thoracic extension with increased L lateral trunk flexion observed as right hand zips up coat.
• Weight bearing through lateral side of R foot.
March 23, 2010: JW completed the task in standing. Feet shoulder width distance apart, L foot forward of R throughout activity. Toed out bilaterally L > R. Weight on RLE > L.
JW’s starting alignment is described as follows:
• Trunk in slight lumbar hyperextension and neutral thoracic extension.
• R hand grasped collar of jacket and brought to LUE.
• LUE in slight GH abduction with slight elbow flexion, wrist, fingers slightly flexed.
JW dons the left sleeve.
• R hand directed sleeve to L hand.
• L elbow extended to direct L UE into sleeve.
• RUE brought sleeve up to L shoulder.
• LUE positioned in GH abduction, internal rotation, scapula abducted, downwardly rotated with wrist neutral with fingers slightly flexed.
JW dons the right sleeve (Fig. A2.1):
• To reach for R sleeve: trunk rotated to the R with thoracic flexion and cervical flexion.
• JW flexed at hips, R knee in slight flexion, L knee hyperextended, increased contact on lateral side of L foot.
• RUE moved into GH extension, internal rotation and adduction, with scapular adduction and downward rotation to grasp right sleeve behind back.
• Once sleeve is grasped, RUE then moved into GH abduction, external rotation and elbow extension with scapular adduction and movement toward upward rotation to slide RUE through sleeve.
• LUE positioned during this segment as follows:
 L scapula in relative abduction and elevation.
L scapula in relative abduction and elevation.
 GH abduction ~30° with internal rotation.
GH abduction ~30° with internal rotation.
 L elbow in ~70° flexion.
L elbow in ~70° flexion.
 Wrist flexion ~10 to 20°, fingers flexed.
Wrist flexion ~10 to 20°, fingers flexed.
JW does up the zipper:
• Trunk maintained in some thoracic flexion and flexed in cervical spine to look at hands to do up zipper.
• Hips moved toward extension but still in slight flexion.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree