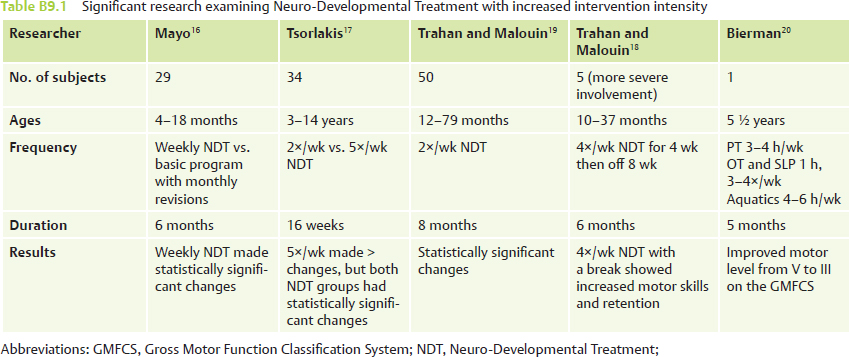
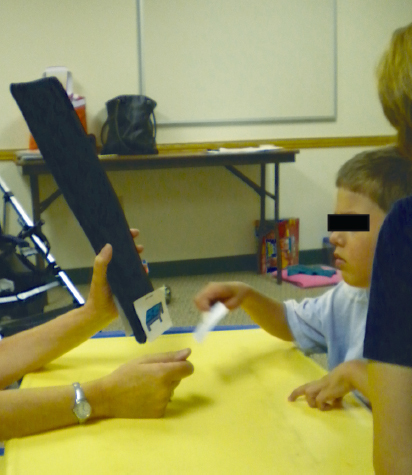
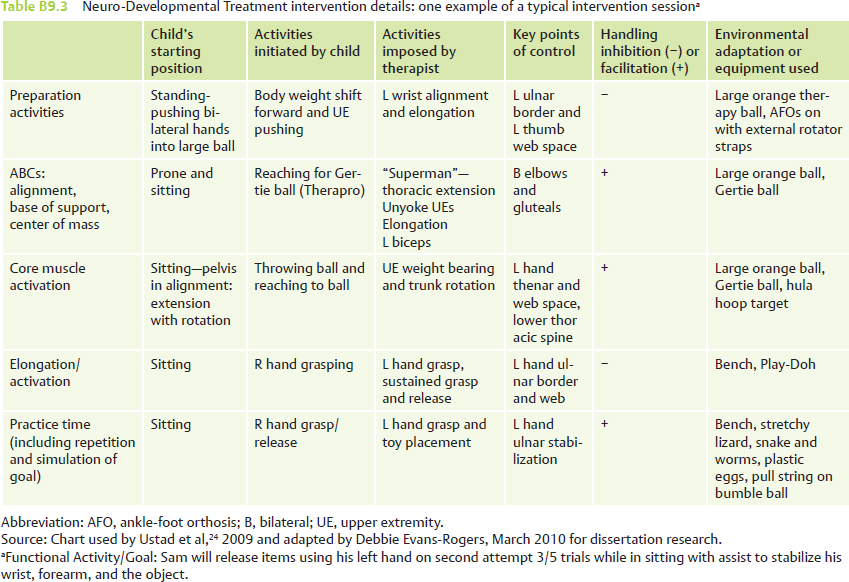
Case Report B9 Examining Neuro-Developmental Treatment with Increased Intensity for a Child with Spastic Quadriplegic Cerebral Palsy and Dystonia Therapists are often plagued with the following questions, How much intensity best meets a particular patient’s and family’s needs? Does a different intensity from the traditional once weekly intervention make a difference in a client’s everyday functioning? This case report examines a young boy whose significant medical history and multiple medical needs require daily nursing intervention. In addition, this case report explores how daily intensive Neuro-Developmental Treatment (NDT) provided by a team consisting of occupational, physical, and speech therapists positively influenced a child and his family. Documented changes in the child’s functional outcomes in family-identified areas of greatest priority are outlined as well. Exploring different interventions of varying intensities and their effectiveness continues to be a focus and need of pediatric therapy research. Pediatric therapists—occupational therapists (OTs), physical therapists (PTs), and speech-language pathologists (SLPs)—in North America are often educated in NDT and use the NDT Practice Model with children having neuromotor difficulties.1,2 The theoretical framework surrounding NDT aligns with the World Health Organization’s (WHO’s) International Classification of Functioning, Disability and Health.3 The dynamic systems theory (DST), neuronal group selection theory (NGST), and principles of motor learning and control all contribute to NDT Practice Theory.4 Intervention using NDT can be provided at varying intensities. In many settings, therapy in the United States is often provided at a weekly frequency for up to 1 hour in duration, often limited by insurance and other health care benefits.5 In the research on intervention, intensive treatment may refer to many different delivery methods of intervention.6 Intensive treatment can relate to specific interventions (direct, consultative, or adjunctive therapy), frequency of intervention sessions (ranging from one time a month to more frequently), or specific length of time of a session or length of time of therapy. In the information specifically on cerebral palsy, the optimal intervention frequency has not been definitively documented in the research.7 The importance of evidence-based research guiding clinicians’ decisions in physical therapy is known.8,9,10 Integrating the best published research evidence, using clinical expertise and patient values, is the essence of evidenced-based practice.11 Optimal intervention intensity for the best functional results with quality research is what caregivers, clinicians, health care providers, including third party payers, and even clients themselves are interested in reviewing. A review of research examining the use of NDT is provided here, with specific analysis of NDT research with increased intensity in recent years. In the past 20 years, many studies have included some aspect of NDT intervention. A few studies have examined using NDT with an increased intervention intensity surrounding NDT certificate courses (Arndt et al12 during a baby course, and Slusarski,13 Knox and Evans,14 and Herndon et al15 during pediatric NDT/Bobath certificate courses). Three of these four studies had positive findings.12,13,14 Since 1991, five studies by researchers—Mayo,16 Tsorlakis et al,17 2 studies by Trahan and Malouin18,19 and Bierman20—used NDT as the type of handling intervention while specifically researching intervention intensity. These five studies are reviewed in Table B9.1. Increased interest by therapists and caregivers about optimal therapy frequency continues. Due to the limited but supportive findings for NDT at an intensive level, more research is required on intervention with increased intensity. This case report explores the effects of NDT using a collaborative team of OTs, PTs, and SLPs with an increased intervention intensity of 4 hours per day for a duration of 2 weeks with a 6-year-old boy with spastic quadriplegia with dystonia cerebral palsy (CP). The unique nature of this intensive program involving extensive team collaboration had added benefits to the client. The team collaboration provided the opportunity for outcomes to be reinforced in different contexts and more easily incorporated into his daily routine. Sam is a 6-year-old boy with the diagnoses of spastic quadriplegia CP with greater involvement on the left side, dystonia, periventricular leukomalacia (PVL), seizure disorder, gastroesophageal reflux (GER), and hypothyroidism. He is the youngest of three children (with an older brother and sister) and has a loving and active family. He enjoys music and singing. Books are one of his favorite hobbies. He is a happy child who is quick to smile, and he squeals with delight and happiness, which can be felt and seen throughout his entire body. Sam also enjoys playing with peers and likes outside play, including swinging, riding a bike, and going down playground slides. He has attended NDT intensive programs held in the past and was treated by all three disciplines during this program. He attended the intensive program for the first time for a 2-week period last year, and he previously attended the weekly intensive sessions to address client and family needs. The NDT intensive program offers daily intervention with OT/PT/SLP, depending on the client’s needs identified by the family. The client participates in 2 hours of intervention in the morning, an hour break for lunch, and then more intervention for 2 hours in the afternoon. In this case report, Sam participated in both the morning and the afternoon sessions. In addition, the intervention is offered for 1- or 2-week sessions based on the client’s needs, and our client participated in the 2-week program. The intensive program Sam attended this year continued to have collaboration among physical, occupational, and speech therapies. He participated in two daily, 2-hour sessions with a total of 4 hours of therapy for 2 consecutive weeks (with weekends off). He was out of town for 1 day the first week due to a family function. Family concerns and goals for the 2 weeks of the intensive included “using a cane or other device less restrictive than a walker” for his walking, working on using his augmentative communication device, especially focusing on how it can be used in the classroom, using name stamping in the classroom, and increasing left-hand use. Please see Fig. B9.1, Fig. B9.2, Fig. B9.3 for the pretest of these goals. Sam was born prematurely at 27 weeks’ gestation. He weighed 1 lb 10 oz and was 13 in long. He was initially placed on a ventilator and was weaned after 6 days. On day 13, Sam had an air embolus resulting in cardiac arrest and a coding episode 10 minutes in duration. He required ventilation for an additional 14 days. He came home from the hospital after 80 days. He had a hernia surgery before he was released from the hospital. Sam was bottle fed until 1 year of age when a gastrostomy tube (G-tube) was placed. The G-tube was changed to a gastrostomy–jejunostomy (G-J) tube in March 2007 and is required to be changed every 3 months. Eye surgery was performed at 1 year of age. Reflux medication was initiated at birth in the hospital and continues to be needed at this time. Sam began to have seizures in October 2006 (almost 3 years old). He continues to have seizures, but they are managed with his current seizure medications. Ear tubes were placed in March 2007. The left pressure equalizer tube has fallen out, but the right tube remains. Hypothyroidism was resolved in January 2010. Present medications include oral baclofen (tone management), Felbatol (Meda Pharmaceuticals, Inc.), Dilantin (Pfizer, Inc.) (seizures), milk of magnesia (constipation), and Prevacid (Takeda Pharmaceuticals USA, Inc.) (acid reflux). Seizures have significantly decreased over the last year. Break-through seizures have occurred since the first seizure in October 2006 with sickness (croup) and change of routines. Sam had phenol and Botox (Allergan) injections in February 2010 and Botox again in May 2010 to further manage his tone and prevent loss of range and skills. Botox injection sites include left biceps, hip adductors, bilateral hamstrings, and right gastrocnemius–soleus muscles. He currently receives physical therapy, occupational therapy, and speech-language therapy each two times per week for 30 minutes through school to address educational needs and one time per week privately to address more medical-based needs. Fig. B9.1 On Sam’s occupational therapy pretest, he needed hand over hand assistance to successfully grasp the name stamp, align the stamp on the line, and push with adequate pressure to leave his name imprinted clearly on the line. Sam functions at the Gross Motor Function Classification System (GMFCS) level IV (able to walk short distances with assistance but needs wheeled mobility in community, and he sits with support of his trunk to maximize hand function).21 In the last year he has grown over 2 in. He currently has a nurse with him throughout the day and will be getting a specially trained dog for his seizures. When asked why the family continues to participate in an intensive program, the family reported that the program has provided a more thorough understanding of Sam’s skill level using collaboration from a multidisciplinary team with good suggestions for future intervention. The basic foundation of NDT encourages therapists to examine the client’s needs from a holistic team approach, which may contribute to the family’s satisfaction in this intensive program.4 Sam attends regular kindergarten (started half days and then transitioned to full days Tuesday–Friday and a half day on Monday in January; typically a child his age attends full days Monday–Friday) and enjoys social interactions with three close friends at school. Although Sam did not enjoy assemblies at school initially due to the noise, he now tolerates and participates in these without difficulty. He is now able to go outside in the winter to play on the playground with his classmates and tolerates hats and mittens. He participates in regular physical education (PE) with assistance from his school PT. Sam is playing regular tee-ball while wearing his ankle-foot orthoses (AFOs) and using his walker. He is eating lunch (self-feeding with utensils and finger-feeding a variety of consistencies) in the lunchroom with his peers, and socializing using an augmentative communication device (has 45 cells), which is used throughout the day. He drinks from a hard, insulated cup with a straw spout. He enjoys participating in all family activities, including recently attending a family wedding out of state requiring Sam and his family to travel by airplane. He attends Sunday school at his church regularly. Fig. B9.3 The physical therapy pretest picture demonstrates Sam using his quad cane walking with assistance from his mom at his right shoulder and left trunk. Sam started kindergarten in 2010 with a one-on-one aide provided by the school, and full inclusion has been a challenge. His home nurses follow him to school to address his medical needs, which include medications given on a regimented schedule, and they are designated as first responders for medical care. In addition, his nurses provide nutrition and medication throughout his day as prescribed. Despite his complex medical needs, Sam is still able to attend school and be included. He needs assistance for pudding-consistency foods during his lunch time, which limits his ability to engage socially with his peers. He is restricted in participation at recess at school due to decreased independent mobility. He is unable to speak and requires his alternative augmentative communication (AAC) device, except for a few signs (i.e., yes, all done, talker, hi/goodbye, thank-you, blows kisses, shakes head no [inconsistently]). He continues to need diapers for bladder and bowel control, but he is working on independent toilet training and is successful two to four times per day. He attends Sunday school at church with the help of a physical therapy student from a local university. Sam enjoys social interactions with peers, and outings, such as going to the water park. It is difficult for him to communicate in all situations (e.g., at the water park because his AAC device cannot be used there). Sam walks with a walker under close supervision. He is able to walk with his mom or the nurse’s assistance holding his two hands. He is able to sit on the floor (W-sitting) and bench-sit independently. He is unable to move from the floor to standing without support, and other transitions require assistance. He uses his right hand for functional use with the left hand as a support. He uses his right index finger to access his AAC device. He easily engages his right hand in play and manipulation, such as turning pages in books, grasping and throwing balls, and playing with water toys. He uses his left hand to engage in batting tasks. He needs assistance for bilateral activities that need more precision, such as assistance to open his left hand and maintain left-hand grasp with resistance. Sam is most often positioned sitting in his wheelchair or on a bench, or he is supported in standing. Postures requiring postural stability, control, and graded movement are difficult for Sam. Functional rotational components use is limited with rotation seen often with lateral flexion of the trunk on the right side (immature weight shift). Asymmetry is noted with the left upper extremity held close to the body with elbow and wrist flexion. The lower extremities (LEs) are often in a crouched posture with hip and knee flexion, and ankle dorsiflexion (in AFOs). External support is often required with transitions and activities requiring stability. See Table B9.2 for a summary of single-system body structure and function. Sam tends to keep a wide base of support (BOS) in sitting on the floor (W-sitting) and a narrower BOS often crossing his LEs in stance with support. When Sam is relaxed, his center of mass (COM) is forward over his BOS (and pelvis posterior). He is unable to actively maintain his COM evenly, with weight bearing often noted asymmetrically shifted to the right side. His COM is maintained at a lower level in stance (crouch gait) over his BOS. Sam does not distribute his weight evenly when sitting or standing. He tends to keep his head laterally flexed to the right and rotated to the left. Bilateral shoulders are elevated, and his scapulae are anteriorly tipped and abducted. The left upper extremity (UE) is held in humeral extension, internal rotation, abduction, elbow flexion, forearm pronation, ulnar deviation, and wrist flexion. His fingers are often flexed and his thumb is collapsed at the carpometacarpal (CMC) joint. Right UE alignment dynamically changes based on the activity. His trunk is laterally flexed to the right, and pelvic obliquity is noted with the pelvis rotated posteriorly on the right side. The LEs are maintained with bilateral hip flexion, adduction, and internal rotation, knee flexion, and ankle dorsiflexion (although the gastrocnemius–soleus is tight; atypical midfoot mobility is noted). Sam moves asymmetrically using the right side for mobility and the left side for stability (poor static and dynamic postural control and stability). Sam maintains posturing of the left UE with minimal active engagement. Sam often does not demonstrate the anticipatory control needed for postural adjustments based on demands external to his body. He demonstrates movement components biased toward flexion with the influence of gravity, but he initiates movement with trunk extension and limited rotational components. Sagittal plane movements are preferred over frontal plane lateral weight shifts and limited transverse plane rotation. He demonstrates increased stiffness both proximally and distally in the left UE and bilateral LEs with stiffness greater in the UE versus the lower and the left greater than the right in the LEs. Limited step and stride length is noted as left greater than right. A crouched gait is often noted while wearing his hinged AFOs. Difficulty is observed maintaining erect posture for independent stance and gait using the gluteal and abdominal muscles simultaneously for postural support. The quadriceps femoris is maintained in an overlengthened position, and terminal knee extension in stance (vastus medialis) is difficult to maintain. Weight bearing is noted with the feet collapsed medially (mid-foot) with the heel maintained in a valgus position. Sam receives milk of magnesia daily to assist with regular bowel movements, and this has significantly reduced his constipation. In addition, he receives high-calorie Ensure (Abbott), which softens stools. Gastroesophageal reflux is controlled with Prevacid taken nightly while sleeping (administered through G-tube). Sam has had retching difficulties in the past, but this has decreased with Prevacid. A G-J tube is used for nutritional and medication needs. The G-tube is used during the day and the J-tube is used only for night medication. After attending kindergarten with 24 classmates this past winter, he was sick from February to May, which included croup, enlarged tonsils and adenoids (scheduled to be removed in August), and strep throat three times. Deep inhalation is limited. Supportive positioning stroller, commercial dynamic stander, posterior walker with bilateral forearm troughs (with TheraBand, The Hygenic Corporation, on the left) and lateral trunk support, a quad cane, bilateral hinged AFOs with free dorsiflexion (these are worn all day except when playing on the floor), bilateral resting night splints to increase dorsiflexion, a left bicep elongation cast, a left wrist and thumb splint, knee immobilizers, and an alternative augmentative communication device (AAC) with 45 space cells wrist talker. Sam is hypersensitive to loud, unexpected noises. Sam is part of an active family, and he has consistently received therapy throughout his life. The family is moving to a new home in a few months with increased wheelchair accessibility. Due to the complex medical needs, extensive motor involvement, and the need for collaboration among team members and family, two outcome measures were used. The Goal Attainment Scale (GAS)22 and the Canadian Occupational Therapy Measure (COPM)23 were used by all disciplines (physical therapy, occupational therapy, and speech therapy) during the 2-week NDT intensive program (see Instrumentation Using the GAS and COPM later in the chapter). These measures were used to capture the functional changes he would make during this time frame. Most standardized measures on the market at this time are not normed on children with complex medical and motor involvement, do not show minimal or qualitative changes, and do not allow collaborative goal setting. The PTs, OTs and SLPs wrote individualized goals using the GAS after discussing priorities with the family. For this case report, Sam’s mom was interested in Sam working on using a less cumbersome walking device, improving his use of his augmentative communication device, and working on stamping his name on papers for school. The intervention described in this case report used the NDT Practice Model. Intervention was provided by two NDT instructors and two NDT-educated therapists. The protocol for the intervention consisted of a thorough assessment; individualized direct handling with problem solving throughout the session; preparatory activities; core postural muscle activation with attention to alignment, BOS (primary weight-bearing surface), and center of mass; elongation (if needed) followed by activation of muscles; practice; repetition of skills; and team collaboration. An example of a typical therapy session is included in Table B9.3. Guidance (facilitation or inhibition) was provided by direct handling for improving body alignment, weight bearing, weight shifting, midrange control, proximal holding, and variety of movement. Refer to Thieme MediaCenter to view a photo sequence that accompanies this table. There are additional photos and videos of other intervention sessions with Sam as well. Sam completed 9 out of the 10 sessions consisting of 4 hours per day of NDT intervention during the 2-week period. One session was missed due to the family having an out-of-town obligation. The pre- and postintervention GAS goals are charted later in the chapter (see Fig. B9.7). Please refer to Summary of GAS Goals for Sam at the end of the chapter.
B9.1 Introduction
B9.2 Research on Neuro-Developmental Treatment with Increased Intensity
B9.3 Case Description
B9.3.1 Relevant Medical History
B9.3.2 Participation
B9.3.3 Participation Restrictions
B9.3.4 Activity and Activity Limitations
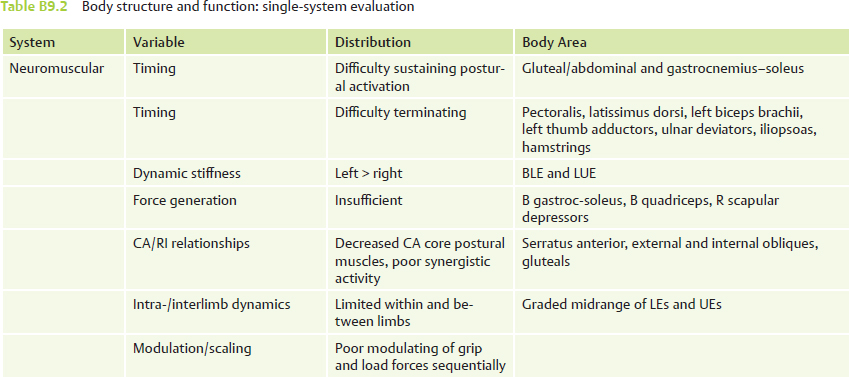
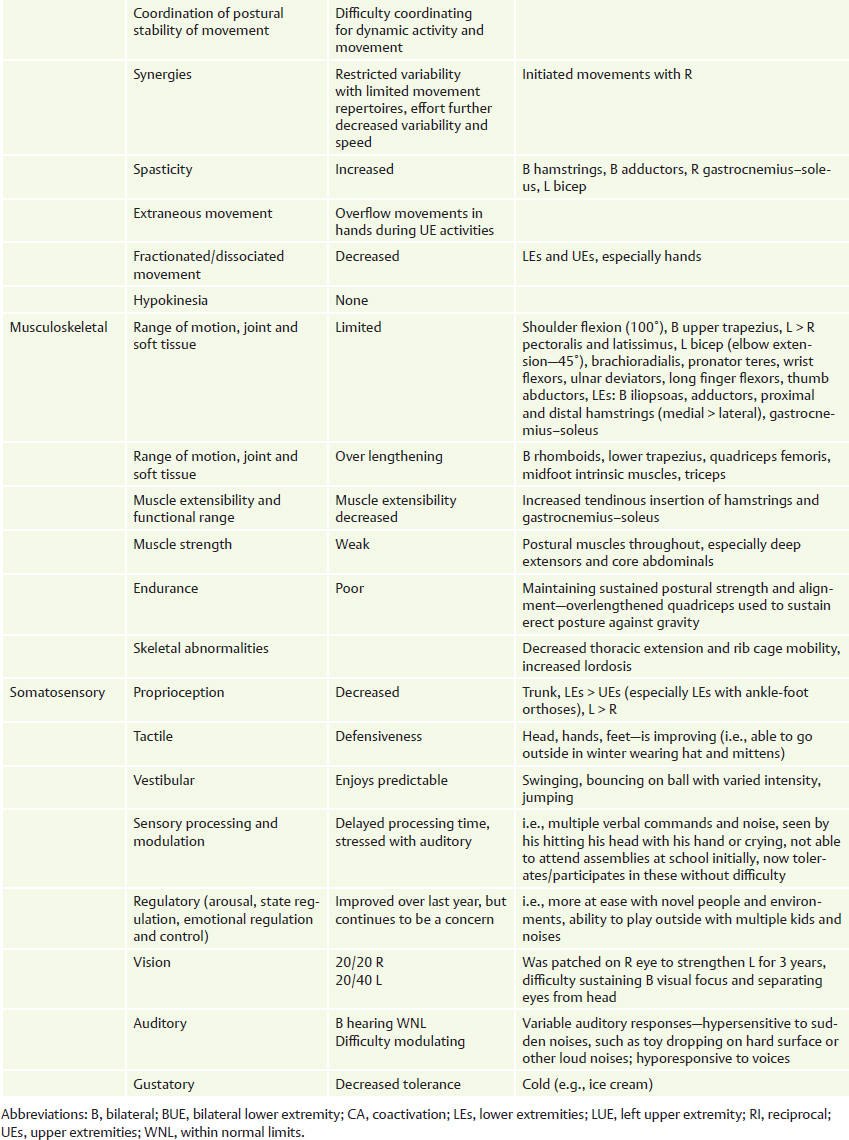
B9.3.5 Body Structure and Function
Relationship of Center of Mass and Base of Support
Alignment
Anticipatory Postural Adjustments and Weight Shift
Movement Components
Muscle Stiffness/Tone
Gait
Gastrointestinal
Respiratory
B9.3.6 Equipment
B9.3.7 Contextual Factors: Environmental and Personal (Facilitators/Barriers)
B9.3.8 Instrumentation/Outcome Measures
B9.3.9 Intervention
B9.3.10 Results
B9.3.11 Preintervention Goals for Physical, Occupational, and Speech Therapy
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree