Chapter 22 Respiratory Physiology
Understanding the Control of Ventilation
Abstract
During sleep, the relative regularity of breathing in resting wakefulness is replaced by marked respiratory variability due to changes in the drive to both the respiratory pump muscles and the upper airway dilating muscles. Breathing during wakefulness is controlled by several factors including voluntary and behavioral elements; chemical factors, including low oxygen levels; high carbon dioxide (CO2) levels and acidosis; and mechanical signals from the lung and chest wall (see Chapter 21 for more information). During sleep, there is loss of voluntary control and a decrease in the usual ventilatory responses to both low oxygen (hypoxemic) and high carbon dioxide (hypercapnic) levels. Both the hypoxemic and hypercapnic responses are most depressed in rapid eye movement (REM) sleep.
Introduction
Chemical Information
The carotid body senses PaO2 (arterial concentration of O2) which sends impulses to the medulla via the ninth cranial nerve. Ventilation usually increases only when PaO2 is less than 60 mm Hg. When PaO2 drops acutely below 30 to 40 mm Hg, the medulla (see Chapter 21 for more information of the brainstem network associated to the control of breathing) may be depressed by the hypoxemia; thus, ventilation may decrease. Carbon dioxide is sensed in both the carotid body and a region of the medulla called the central chemoreceptor. As PaCO2 (arterial concentration of CO2) increases, there is a brisk linear increase in ventilation. Drugs that depress central nervous system function (e.g., some benzodiazepines, opioids) may profoundly depress chemical drives to breathe in normal altitude (see Chapter 24 for the paradoxical effects of benzodiazepines on respiration during sleep in high altitude).
Physiology of Ventilatory Control During Sleep
Hypoxic Ventilatory Response during Sleep
Adult Human Beings
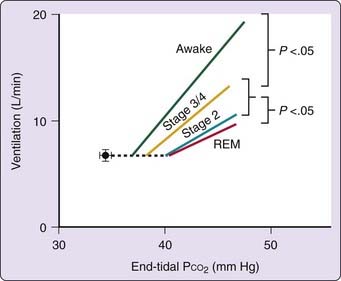
The ventilatory response to hypoxia falls during sleep in healthy adults (Fig. 22-1).1–4 The hypoxic ventilatory response was lower during non–rapid eye movement (NREM) sleep than during wakefulness in the studies in which the subjects were exclusively or mostly men1,2 but the responses were similar in wakefulness and NREM sleep in the studies in which women predominated.3–5 It is not clear why there is such a difference between the genders in the effect of sleep on the hypoxic ventilatory response and whether hormonal factors might be important. Comparison of the results in men and women (Fig. 22-2) shows that the major gender difference is in the levels of ventilatory response during wakefulness, which is much higher in men than in women,4 whereas the responses in NREM sleep were not different between the genders. During NREM sleep both the ventilatory responses to hypocapnic hypoxia and the posthypoxic ventilatory decline were similar between the genders.6 It was also found that the posthypoxic ventilatory decline in NREM sleep was not associated with a decline in respiratory frequency nor with any change in airway mechanics.7
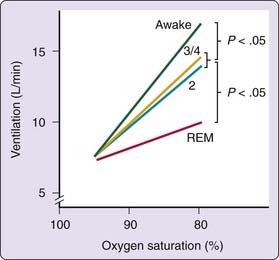
Figure 22-1 Mean relationship between expired ventilation and decreasing O2 saturation in the different sleep stages in 12 subjects, 6 male1 and 6 female.4
(From Douglas NJ. Control of ventilation during sleep. Clin Chest Med 1985;6:563.)
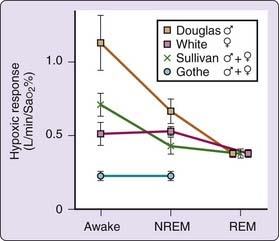
Figure 22-2 Comparison of hypoxic ventilatory responses in different sleep stages in four studies1,3,5 in healthy subjects indicating the unchanged responses in NREM sleep in women, and the similarity of responses in REM sleep in all studies.
The hypoxic ventilatory response during rapid eye movement (REM) sleep is lower than in NREM sleep in both men and women.1–4 The hypoxic ventilatory response during REM sleep was remarkably similar in all three directly comparable studies:1,2,4 about 0.4 L/min/percentage SaO2 (see Fig. 22-2).
Hypercapnic Ventilatory Response during Sleep
Adult Human Beings
The hypercapnic ventilatory response is depressed during sleep in adult human beings (Fig. 22-3). Studies performed in either electroencephalogram-documented11–14 or presumed15–17 NREM sleep showed that the slope of the ventilation-CO2 response line falls during NREM sleep, compared with wakefulness. Two large studies12,13 suggested that the decrease in response from wakefulness to NREM sleep is approximately 50%. Although Bülow12 reported lower responses in stages 3 and 4 sleep than in stage 2 sleep, later researchers13,18 found no such difference. In fact, Bülow did not apply statistics, and his data indicate considerable overlap (see Figs. 21, 26, and 27 in reference 12). Indeed, no separation is evident until high CO2 levels are reached when the number of data points is small.
NREM sleep does not significantly change the position of the ventilation-CO2 response line, as assessed by the rebreathing technique with extrapolation of the CO2 response line to the intercept at zero ventilation.13,18 However, as the slope of the response line decreases during NREM sleep, the CO2 increment between the awake resting ventilatory set-point and the ventilatory response line is increased significantly during NREM sleep (see Fig. 22-3).12,13
Berthon-Jones and Sullivan18 found that healthy women did not change the hypercapnic ventilatory response from wakefulness to NREM sleep, a result consistent with the finding by Davis and colleagues19 of higher ventilatory responses during sleep in women than in men. In contrast, neither Douglas and colleagues13 nor Gothe and colleagues20 identified any difference between the genders in any stage. Three groups have measured the hypercapnic ventilatory response during REM sleep in adults. Douglas and colleagues13 found that in 10 of 12 subjects, the hypercapnic response was lowest in REM sleep, compared with either wakefulness or NREM sleep. The mean hypercapnic ventilatory response during REM sleep was 28% of the level during wakefulness (see Fig. 22-3). These authors were unable to accurately define the position of the hypercapnic ventilatory response line because some responses during REM sleep had negative slopes. Berthon-Jones and Sullivan18 and White21 found a tendency for the lowest responses to occur during REM sleep.
Adult Animals
As in adult human beings, the hypercapnic ventilatory response is lower in NREM sleep than in wakefulness in dogs22,23 and cats,24 with a further drop in response from NREM to REM sleep.22–25 Sullivan and colleagues23 found that the hypercapnic ventilatory response was lower in phasic than in tonic REM sleep in dogs.
Added Resistance and Airway Occlusion During Sleep
Adult Human Beings
Sleep modifies the ventilatory response to added inspiratory resistance.26–29 All studies agree that NREM sleep blunts the respiratory timing response to added resistance,26–30 with some reporting a net effect on ventilation as well.27,29,30 In adults with asthma, the ventilatory response to induced bronchoconstriction is not modified by sleep.31 Issa and Sullivan32 reported that, in response to airway occlusion, there was a progressive increase in respiratory effort during NREM sleep and rapid, shallow breathing during REM sleep.
Animals
In both dogs33,34 and cats,24 ventilatory compensation for added loads is maintained during NREM sleep at the level found in wakefulness. However, when the respiratory system is further stressed by combining resistive loading with hypercapnia, the ventilatory and airway occlusion responses to loading are found to be impaired during both NREM and REM sleep.24
Arousal Responses
Isocapnic Hypoxia
In normal subjects, isocapnic hypoxia is a poor stimulus to trigger arousal from sleep (Fig. 22-4), with many subjects remaining asleep with SaO2 as low as 70%1,2,5 and no difference between NREM and REM sleep in arousal threshold. Conversely, the arousal sensitivity to hypoxia is decreased in REM sleep in patients having obstructive sleep apnea with asphyxial hypoxia,35 in dogs with isocapnic hypoxia,8,9 and in cats with hypocapnic hypoxia.36 Carotid body denervation reduces arousal sensitivity in dogs7 but does not alter the arousal threshold in cats.36
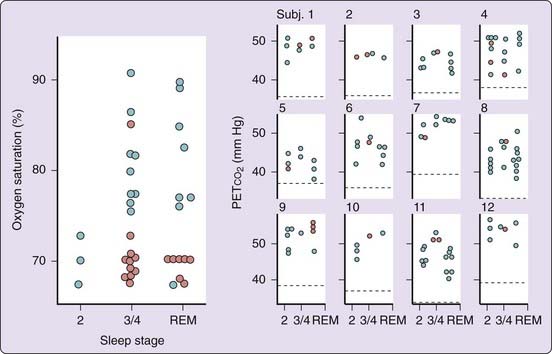
Figure 22-4 Arousal responses to hypoxia and hypercapnia13 in different sleep stages, indicating whether the subjects remained asleep (red circles) or aroused (blue circles). The hypoxic responses are total data for 9 subjects; the hypercapnic plots are for each of 12 individuals, 6 females (1-6) and 6 males (7-12), indicating with the dotted line mean PETCO2 in wakefulness in each subject.
(From Douglas NJ. Control of ventilation during sleep. Clin Chest Med 1985;6:563).
Hypercapnia
Hypercapnia also produces arousal from sleep at variable levels3,11,13 but awakens most subjects before the end-tidal CO2 has risen by 15 mm Hg above the level in wakefulness.3,11–13 Berthon-Jones and Sullivan16 reported arousal thresholds up to 6 mm Hg higher in slow-wave sleep than in either stage 2 or REM sleep in male but not in female subjects, whereas Douglas and associates13 found no gender or sleep stage-related differences. Hypoxia increases the sensitivity to CO2 arousal.35
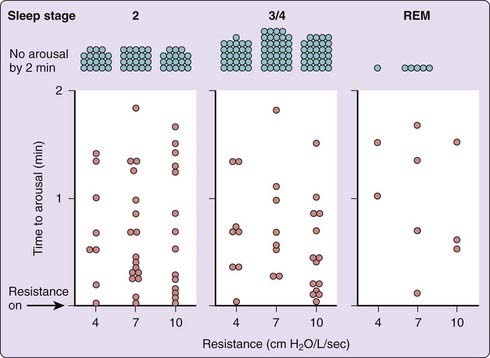
Added Resistance
Human beings tend to arouse from sleep following either the addition of an inspiratory resistance28 or the occlusion of inspiration.37 Added inspiratory resistance was found to produce a similar percentage increase in arousal frequency in stages 2 and 3/4 and REM sleep.26 However, the arousal frequency during control sleep periods was lowest in stages 3/4 sleep and remained significantly lower during slow-wave sleep than in REM sleep after the addition of inspiratory resistance (Fig. 22-5).24,25
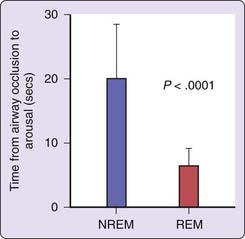
Arousal from REM sleep after airway occlusion32,38 is far more rapid than arousal from NREM sleep (Fig. 22-6; nearly 3 times quicker in REM), whereas patients with obstructive apneas have longer apneas during REM sleep. Upper airway receptors would be exposed to respiratory pressure changes in normal people with airway occlusion but in patients with sleep apnea receptors above the level of occlusion would not experience pressure swings. However, it is unclear why these upper airway receptors should be more effective in REM sleep than in NREM sleep in normal subjects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree