Role of BMP in Cervical Spine Surgery
Jeffrey S. Earhart
Wellington K. Hsu
The clinical success of ventral and dorsal cervical fusion is often dependent on the surgeon’s ability to induce solid bony healing. Tricortical autograft harvested from the iliac crest has historically been the gold standard in this setting due to its structural integrity and its combination of osteoconductive and osteoinductive properties. However, donor-site morbidity and complications from graft harvest (1, 2, 3, 4 and 5) have led to the investigation of alternative agents. The use of structural allograft bone has increased in the last decade because it is readily available, limits operating room time and blood loss, and eliminates complications at the donor site. However, allograft use is potentially complicated by disease transmission, host rejection, and higher pseudarthrosis rates, especially with multilevel procedures (6). Because of the inherent challenges of iliac crest autograft or allograft bone use, other bone graft substitutes have gained interest in the cervical spine.
FUSION RATES WITH BMP IN THE ANTERIOR CERVICAL SPINE
The discovery of bone morphogenetic proteins (BMPs) by Marshall Urist (7) in 1965 has led to a diverse area of research dedicated to the identification and characterization of osteoinductive growth factors. Members of the TGF-β superfamily, BMPs have been proposed for a number of applications in orthopaedic surgery (8). Although at least 20 different BMPs have been reported (9), much of the clinical study has focused on recombinant human BMP-2 (rhBMP-2) (INFUSE; Medtronic, Sofamor-Danek, Memphis, TN) and rhBMP-7 (osteogenic protein-1 or OP-1).
rhBMP-2 and BMP-7 have been evaluated in numerous preclinical models, and successful healing in long bone defects has been reported (8,10, 11 and 12). Similar findings have been demonstrated in spinal arthrodesis models in animals (13, 14, 15 and 16). Food and Drug Administration (FDA) approval has been granted for the use of rhBMP-2 to enhance anterior lumbar spinal fusion (17) and rhOP-1 to supplement posterior spine fusions. In a prospective, randomized controlled pilot study, Baskin et al. (18) compared cancellous iliac crest autograft to rhBMP-2 (0.6 mg per level) reconstituted within a type I collagen sponge in a structural fibular allograft (CORNERSTONE-SR Allograft Ring; Regeneration Technologies, Alachua, FL) in 33 patients after a one- or two-level anterior cervical discectomy and fusion (ACDF) with 2-year follow-up. Statistically significant improvement for both groups at all postoperative intervals were noted in Neck Disability Index (NDI), composite neck pain, and composite arm pain scores. Although both groups significantly improved overall, NDI and arm pain scores demonstrated statistically greater improvement in the rhBMP-2 group at the 24-month time point (p< 0.055). Donor-site pain in the control group was statistically significantly greater up until 6 weeks postoperatively (p < 0.007), but not at the 24-month follow-up. All patients in both groups met radiographic criteria for fusion at 6, 12, and 24 months.
Similarly, Buttermann (19) reported results from a nonrandomized prospective study of rhBMP-2 and allograft (0.9 mg per level) compared with tricortical iliac crest autograft in one-, two-, and three-level ACDF. Notably, in the investigational group, a portion of the BMP-soaked type I collagen sponge was placed outside the allograft ring in the disk space along with autograft obtained from anterior osteophytes. Furthermore, the iliac crest donor site in control patients was reconstructed with fibular allograft. Over the 2- to 3-year period of follow-up, both groups showed statistically significant improvement in all primary outcome measures (p < 0.01), and at no point was there a significant difference between groups.
Although no postoperative complications were reported by Baskin et al. (18), the rhBMP-2 group in Buttermann’s study experienced a significantly higher rate of neck swelling, dysphagia, and ICU readmissions for postoperative monitoring. Based on this experience, the author concluded that postoperative complications related to anterior cervical edema were concerning enough to warrant further investigation (19).
Although the quantity of published data is limited, preliminary evidence suggests that fusion rates with the
use of rhBMP-2 in the ventral cervical spine are at least equivalent, if not superior, to iliac crest autograft. Ongoing randomized controlled clinical trials studying the use of rhBMP-2 in multilevel ventral cervical fusions, where a greater difference in pseudarthrosis rate may be seen, will further develop guidelines for the potential role for growth factor therapy in anterior cervical spine procedures.
use of rhBMP-2 in the ventral cervical spine are at least equivalent, if not superior, to iliac crest autograft. Ongoing randomized controlled clinical trials studying the use of rhBMP-2 in multilevel ventral cervical fusions, where a greater difference in pseudarthrosis rate may be seen, will further develop guidelines for the potential role for growth factor therapy in anterior cervical spine procedures.
COMPLICATIONS
Despite the clinical success of rhBMP-2 reported in the cervical spine, a host of associated complications have been reported in the literature. Respiratory difficulty, dysphagia, postoperative edema, hematoma/seroma formation, heterotopic ossification (HO), end plate resorption, and graft subsidence have all been associated with the use of rhBMP-2 in an ACDF. Collectively, this body of evidence has led to both manufacturer (20) and formal FDA (21) warnings against the use of rhBMP-2 during anterior cervical procedures.
VENTRAL NECK SWELLING
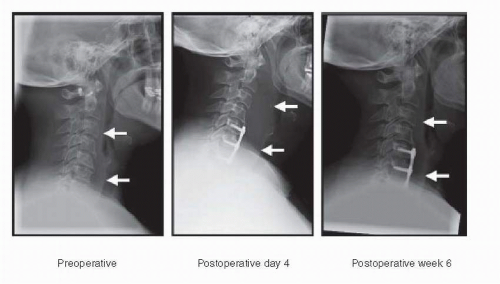
The most commonly reported complication related to ventral cervical BMP use has been local, diffuse soft tissue swelling leading to dysphagia and other respiratory complications (19,22, 23, 24, 25, 26 and 27). Smucker et al. (25) compared ACDF outcomes in experimental and control cohorts, noting a significantly increased rate of swelling complications among patients exposed to rhBMP-2 (27.5% vs. 3.6%, p< 0.0001; Fig. 133.1). The authors further described several swelling-related complications entirely unique to the rhBMP-2 cohort of 69 patients including visible neck swelling (n= 2), reintubation (n= 2), incision and drainage of the swollen site (n = 3), and outpatient ENT consultation (n = 2), which were statistically significantly greater compared to the control group (odds ratio 10.1, p < 0.0001) (25). Both Tumialan et al. (26) and Shields et al. (24) have also reported significant rates of dysphagia after use of rhBMP-2 (7% and 7.9%, respectively). These findings have been confirmed by other additional comparative studies (19,27). Several studies of rhBMP-2 in the anterior cervical spine have found the onset of clinically significant dysphagia to be delayed when compared to routine ventral approaches (19,22,24, 25, 26, 27 and 28). Prevertebral soft tissue swelling following routine ACDF has historically been reported on the second or third postoperative day (29), while swelling from rhBMP-2 are commonly delayed after postoperative day 4 (19,27).
The severity and duration of swelling also appears to increase with rhBMP-2 use as compared to ACDF utilizing autograft or allograft. Vaidya et al. found statistically significant differences in soft tissue distension measured on lateral plain radiographs up to 6 weeks after surgery with moderate clinical symptoms for 12 months after surgery. This was significantly greater than the control cohort (0.5 months of symptoms) (27). Tumialan et al. (26) observed severe dysphagia in 2.5% of patients in his study, 80% of whom required percutaneous endoscopic gastrostomy tube placement. Other studies have confirmed these findings (19,24,25).
HEMATOMA/SEROMA
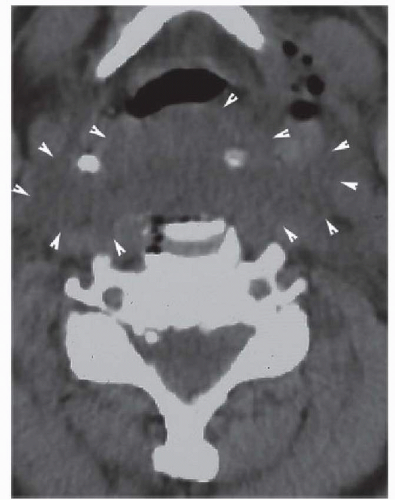
Hematoma and seroma formation in the ventral cervical spine risks similar devastating consequences seen with severe diffuse soft tissue swelling. Tumialan et al. found a 2% incidence of hematoma/seroma with the use of rhBMP-2, each requiring operative evacuation. Interestingly, a dose reduction during this study did not significantly impact the incidence of hematoma or seroma, with cases noted in both high-dose (1.1 to 2.1 mg per level) and low-dose (0.7 mg per level) cohorts. This report was in contrast to the higher incidence of dysphagia with greater rhBMP-2 exposure in the same patient cohort (26). In a cohort of ACDF and ventral corpectomy patients, Shields et al. (24) reported a 9.9% incidence of postoperative hematomas in a retrospective review (7.9% of ACDFs, 38.8% of corpectomies), with 11 of 15 patients diagnosed on postoperative day 4 or 5 (Fig. 133.2). This time course is similar to the delayed onset of soft tissue swelling noted in other studies (19,27). Although direct causation has not been proven in these studies, the
delayed presentation of these complications suggests a common mechanism in which rhBMP-2 may be associated with these problems.
delayed presentation of these complications suggests a common mechanism in which rhBMP-2 may be associated with these problems.
ECTOPIC BONE FORMATION
Ectopic bone formation in the anterior cervical spine has potentially devastating consequences because of the presence of nearby vital anatomic structures. In a retrospective review of 24 patients (39 levels) undergoing ACDF with polyetheretherketone (PEEK) cages and 2.1 mg of rhBMP-2 per level, Boakye et al. (30) reported three instances of heterotopic bone formation in postoperative CT imaging 8 months after implantation. None of these cases were clinically symptomatic; however, ectopic bone growth was found in the spinal canal despite placement of rhBMP-2 entirely within the PEEK spacer. The authors suggested a dose-dependent phenomenon through reference to their unpublished data, in which a reduced dose led to no subsequent cases of HO (30).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree