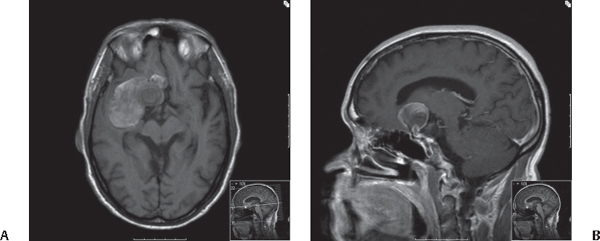
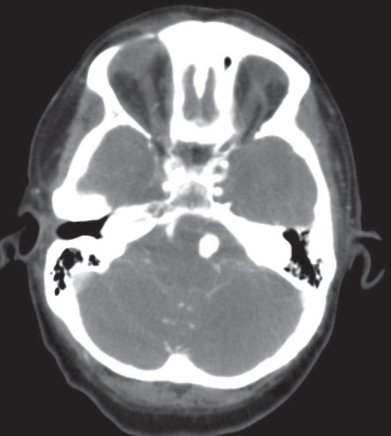
44 What are some of the basic principles of skull base surgery? 1. Removing as much bone as safely possible to avoid brain retraction 2. Sharp dissection is usually safer than blunt dissection especially in proximity to cranial nerves or major arteries or veins. 3. Planning closure is indispensable prior to beginning the procedure, which may include vascularized flaps and grafts harvested from distal sites. 4. The use of the high-speed drill is crucial and must be mastered in a laboratory environment prior to its practice in the operating room. 5. It is best to aim for total resection in case of tumors during the first procedure, as a second procedure is always more difficult and poses further challenges.1 What adjuncts are typically used in the operating room when performing skull base surgery? 1. The operating microscope and/or loupe magnification 2. Microdissectors (such as the Rhoton micro-dissecting instruments) 3. The high-speed drill with cutting and diamond burrs 4. Intraoperative monitoring such as cranial nerve monitoring as well somatosensory and motor evoked potentials 5. Preparation for a lumbar drain or ventriculostomy placement 6. Preparation of the abdomen or thigh for harvesting of fascia lata or fat grafts 7. Adequate self-retaining retractors, such as the Greenberg, Fukushima, or Budde halo retractor system 8. Arm rests for the surgeon 9. An assistant well versed in cranial surgery 10. Two suction catheters with a suction reducer as well as microsuction tips of various sizes and lengths 11. Various-sized bipolar 12. Ultrasonic aspirator 13. Imaging guidance neuronavigation or intra-operative ultrasound 14. Mayfield head holder 15. A central line, arterial line, and precordial Doppler probe if operating near a venous sinus2 What is meant by the term subfrontal approach and what are its most common variations? The subfrontal approach includes a bifrontal craniotomy, and, depending on the site of the lesion that is being addressed, can also include removal of the supraorbital rims alongside with the anterior aspect of both orbital roofs. What areas can be exposed with the extended subfrontal approach? 1. Anterior cranial fossa 2. Middle and posterior fossa between the petrous and cavernous ICA 3. Foramen magnum 4. Anterior portion of the third ventricle3 How inferior is the craniotomy performed and what are the landmarks for the osteotomies? Down to the level of the anterior cranial fossa, performing a cut at the nasofrontal suture through the frontal sinus. This provides a view flush with the fossa without any obstruction. Once the frontal sinus has been opened, how can infections be prevented? 1. Exenteration of the mucosa and opening of the posterior wall of the sinus into the cranial cavity 2. Packing of the nasofrontal ducts with fat or muscle How is the frontal dura containing the frontal lobes separated from the dural base without injury to the superior sagittal sinus (SSS)? This is done by ligation of the inferior portion of the SSS and sharp dissection toward the falx. The subfrontal approach can give access to the interpeduncular cistern; what is the structure that needs to be respected while gaining access to this region and why? The Liliequist membrane, which protects important vascular structures, including the basilar and posterior cerebral arteries and perforators from the posterior circulation What is the most common transient complication of approaches that include removal of the roof of the orbit? Swelling of the tissues surrounding the orbit, especially if the periorbita was violated during the dissection from the orbital roof The first maneuver to release pressure from the optic nerves is unroofing the optic canal. What is the general direction of the optic canal from the perspective of this approach? The optic canals is directed downward and outward at an angle of 45 degrees. Does the anterior cranial fossa need to be reconstructed? No. Reconstruction is not always necessary, especially if a vascularized pericranial flap is used for closure. What areas can be reached through a middle fossa approach? The middle fossa approach with its variants and extension can be safely used to approach lesions of the petrous apex, infratemporal and pterygopalatine fossa, clivus, and sphenoid region. When the condyle of the mandible has to be resected, what deficit is expected? It is usually tolerated very well. At times the patient can have a slight difficulty chewing on the side of the condylectomy. What is the most important landmark in the middle fossa to safely control the petrous carotid? The greater superficial petrosal nerve usually lies 0.5 cm superiorly to the horizontal segment of the carotid artery.2,4 How can the petrous ICA be controlled if needed during removal of lesions of the middle and infratemporal fossa? In two ways: either at the neck or by the unroofing of the petrous ICA and inflation of a Fogarty balloon compressing the artery.5 Approaching clival lesions through this approach at times requires removal of the tympanic bone; what are the landmarks to do it safely without injuring the eustachian tube? Lateral to the genu of the petrous ICA, the tensor tympani muscle is directly above the eustachian tube. After the bone flap of middle fossa craniotomy is turned additional bone is rongeured to have an exposure flush with floor of the temporal fossa. What are the risks associated with this maneuver? What structure is at risk? Excessive force can fracture the external auditory meatus. How can the sphenoid sinus be approached through the middle fossa approach? Drilling the bone between V2 and V3 provides access to the lateral compartment of the sphenoid sinus. What are the most common complications of the middle fossa approach? Lesion to the ICA, CSF leak through the eustachian tube or sphenoid, malocclusion When elevating the dura from the petrous pyramid, what are the landmarks to be reached? The internal acoustic meatus and the crest at the ridge of the pyramid6 The extradural middle fossa approach allows for a multiplicity of working angles and the possibility of reaching and safely removing infratemporal, intramaxillary, intrasphenoidal, intraorbital, cavernous sinus, and posterior fossa extensions (through the enlarged mouth of Meckel’s cave).7 In lesions of the middle fossa involving the tentorium, which cranial nerve is at risk of injury? The trochlear What surgical maneuver improves basal exposure in the middle fossa approach? The zygoma is detached using the B1 drill attachment with oblique anterior cuts through the malar eminence and the through the root posteriorly. The temporal muscle is detached at the level of the superior temporal line and reflected down with the zygoma to access the middle fossa. What does the cranioorbitozygomatic (COZ) approach involve? It involves a craniotomy centered around the pterion that is further extended to includes the superior and lateral orbital wall as well as the vertical and sometimes the horizontal part of the zygoma. What is the primary advantages of the COZ approach? This approach brings the structures in the base of the anterior and middle fossa in closer proximity to the surface and facilitates their being reached via multiple directions, while obviating the need for retraction of the brain.8 What lesions can be treated using the COZ approach?8,9 • Tumors such as sphenoid wing meningioma, clinoidal or cavernous sinus meningiomas, craniopharyngioma, or large pituitary adenomas • Complex aneurysms of the circle of Willis such as complex anterior communicating artery aneurysms or basilar apex aneurysms • Certain craniosynostosis and cranial deformities Fig. 44.1 T1-weighted MRI with contrast. Axial (A) and midsagittal (B) sections showing large paraclinoid aneurysm with thrombosis, which is optimally surgically approached via the cranio-orbitozygomatic approach. What medial landmark can be used as a medial limit for the craniotomy anteriorly, while performing a COZ approach? The craniotomy should not extend beyond the supraorbital notch, as beyond that notch typically the frontal sinuses are entered. What complication can arise from excessive compression of the orbital apex during the COZ approach? Bradycardia may be experienced secondary to the oculocardiac reflex when excessive compression is performed along the orbital apex. What complication can arise from lack of reconstruction of the orbital roof/wall at the end of the COZ approach? Enophthalmos If the original bone cannot be used for reconstruction of the orbital wall, how can this be circumvented in the COZ approach? • On certain occasions due to the use of the high-speed drill or rongeurs the orbital roof or lateral wall may be thinned down to the point where it cannot be reconstructed primarily at the end of the procedure. • In such cases titanium mesh with or without a combination of synthetic bone agents may be used to reconstruct the superior and lateral wall of the orbit to prevent enophthalmos postoperatively. What is the petrosal approach? It is an approach centered on the petrous temporal bone that enables access to the region of the clivus and petrous apex. What is the difference between the anterior and posterior petrosal approaches? • The anterior petrosal approach provides exposure and access to lesions mainly located in the middle fossa, cavernous sinus, and upper clivus. • The posterior petrosal approach provides access to lesions of the posterior fossa laterally, the cerebellopontine angle, and the lower clivus. What are some of the indications for the anterior petrosal approach? • Tumors involving the cavernous sinuses area and upper clivus such as meningioma, dermoids, epidermoids, schwannoma, and other extraaxial skull-based tumors of the middle fossa • Low-lying basilar apex aneurysms and other aneurysms of the posterior circulation at the level of the upper clivus What are some of the indications for the posterior petrosal approach? • Extraaxial tumors located in the lateral aspect of the posterior fossa such as petroclival or tentorial meningioma, vestibular schwannoma or other lower cranial nerve schwannoma, dermoids, epidermoids, and other lower clival skull-based tumors10 • Intraaxial tumors involving the brainstem along its anterior or anterolateral aspect • Certain aneurysms and vascular lesions located in the lateral aspect of the posterior fossa such as per the vertebrobasilar junction or basilar trunk aneurysms When is the combined petrosal approach used? This approach is used in cases of tumors or lesions extending from the middle fossa to the posterior fossa such as the spheno-petroclival meningioma or other extensive type of surgical skull-based disease.11,12 When performing a mastoidectomy, how are the semicircular canals and facial nerve differentiated from the mastoid air cells? The density of the bone changes when proceeding with drilling the mastoid air cells with a diamond burr. When the area appears to be of higher bone density, this usually means that the semicircular canals or the facial canal have been reached. What are some key steps in the closure in a posterior petrosal approach? • The pericranial graft (or fascia lata) is typically harvested to close the dura in a watertight fashion so as to prevent CSF leaks. • A fat graft is harvested from the abdomen or thigh and laid over the mastoidectomy defect. • The superficial wall of the mastoidectomy may be reconstructed with titanium plates or bone substitutes. • Closure of the soft tissue and skin is done in layers with a running nylon suture for the skin. • A tight mastoidectomy dressing is then applied to the scalp to prevent pseudomeningocele formation. Where is the tentorium sectioned in the petrosal approach? It is typically sectioned behind the trochlear nerve. What are the advantages of the petrosal approach as compared with the retrosigmoid approach? 1. Minimal retraction into the cerebellum and temporal lobe 2. Shorter distances to the clivus 3. More direct visualization of the anterior and lateral aspect of the brainstem 4. Preservation of the venous structures such as the sigmoid sinus and vein of Labbé Around which venous sinus are burr holes made when performing the petrosal approach? The transverse sinus13 What is the anatomical structure located within the mastoid above which it is safe to drill the mastoid air cells without having to worry about injuring the facial nerve or semicircular canals? The antrum What are the three approaches used most commonly to treat acoustic schwannomas? 1. Retrosigmoid14 2. Middle fossa6 3. Translabyrinthine15 When is the translabyrinthine approach typically indicated? When there is no functional hearing on the side ipsilateral to tumor15 When is the middle fossa approach typically indicated? In cases of small intracanicular tumors16 When is the retrosigmoid approach typically indicated? In most cases of acoustic schwannoma, especially in those schwannomas that are large, in a patient with functional hearing or with compression of the brainstem What are typical complications encountered with the retrosigmoid approach? Cerebellar contusion, hydrocephalus, damage to the brainstem with vegetative state, cranial nerve injury including hearing loss, facial nerve injury, loss of facial sensation, lower cranial nerve injury with dysphagia and dysphonia, cerebrospinal fluid leak, tumor recurrence or regrowth, cosmetic defects How is a cerebrospinal fluid leak prevented in the retrosigmoid approach? • A watertight dural closure must be completed with the use of a pericranial graft or other dural replacement such as fascia lata or synthetic graft. • Tisseel fibrin glue or other type of sealants are typically applied over to dura. • Hydrocephalus should be managed with ventriculostomy or shunt placement to decrease the transmural pressure of CSF along the dural opening. • The mastoid air cells must be adequately sealed with bone wax when performing mastoidectomy, and a fat graft can be harvested and placed along the mastoid area. • The skin is closed in a watertight fashion using a running or a running and interlocking nylon suture. • The head should be wrapped tightly with a mastoid dressing to prevent pseudomeningocele formation.17,18 How is a cerebrospinal fluid leak treated once it occurs in the retrosigmoid approach? Treatment measures are described from simple to more complex: • The patient’s head is elevated and the skin closure is reinforced. • The patient is kept dry with diuretic agents such as acetazolamide. • In the event that the leak persists after 24 to 48 hours, a lumbar drain should be placed. • A CT scan of the head should also be obtained to evaluate for hydrocephalus or pseudomeningocele as well as for the need of ventriculostomy placement in such cases. • If these measures are unsuccessful, then wound revision surgery and better watertight closure with sealants and fascial grafts should be considered.17,18 What lesions are typically treated using the far lateral approach? • Foramen magnum tumors such as meningiomas, schwannomas, chordomas, brainstem gliomas, etc. • Certain vascular lesion such as aneurysm or arteriovenous malformations of the posterior circulation located laterally such as posterior inferior cerebellar artery (PICA) aneurysms or vertebral artery aneurysms • Other lesions of the craniovertebral junction Fig. 44.2 CT angiogram, axial cut, showing large vascular lesion consistent with an aneurysm located along the lateral aspect of the medulla, consistent with either a vertebral artery or a PICA aneurysm.
Skull Base Approaches and Targets
44.1 General Operative Principles
44.2 Anterior Fossa: The Subfrontal Approach
44.3 Middle Fossa
44.3.1 The Middle Fossa Approach
44.3.2 The Cranio-Orbitozygomatic Approach
44.3.3 The Petrosal Approach (Anterior, Posterior, and Combined)
44.4 Posterior Fossa and Craniocervical Junction
44.4.1 Acoustic Schwannomas and the Retrosigmoid Approach
44.4.2 The Far Lateral Approach
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Skull Base Approaches and Targets
Only gold members can continue reading. Log In or Register to continue




