Sleep-onset delay is a common problem and probably accounts for most patients who present with a complaint of insomnia. It usually has psychogenic causes. Sleeplessness may develop from a continued association with stimulating practices and objects at bedtime. Such patients sleep better away from their bedrooms and usual routines, for example, while on vacation. A conditioned internal factor also may develop in the form of apprehension about unsuccessful and excessive efforts to sleep. Conscious efforts to fall asleep result in CNS arousal. These patients consider themselves “light sleepers.” They often have multiple somatic complaints such as back pains, headaches, and palpitations that lead to occasional abuse of alcohol, barbiturates, minor tranquilizers, and hypnotics. The sleep of such patients in the sleep laboratory is usually better than at home because the conditioning factors that are active at home are reduced in the laboratory. Multiple specific psychiatric illnesses associated with anxiety, such as personality disorders (e.g., anxiety and panic disorders, hypochondriasis, obsessive-compulsive disorders), and schizophrenia, also can be associated with sleep-onset difficulty.
Drugs also can compromise the initiation of sleep. When obtaining a history, the physician should inquire specifically about possible precipitants of drug-induced insomnia. In addition to steroids and dopaminergic agents, xanthine derivatives (e.g., caffeine and theophylline) may cause sleep disruption. A frequently overlooked class of agents is the beta-adrenergic agonists, such as terbutaline and phenylethylamine derivatives (used as stimulants, appetite suppressants, and decongestants). If such medications are taken late in the day, and in increasing amounts because of the development of tolerance, they easily can cause sleep-onset delay as well as sleep fragmentation and “lightening” of sleep. Such inadequate sleep provokes daytime symptoms such as sleepiness, which is responsible for a further increase of ingestion of the drug to promote alertness.
Similar delay in sleep onset may result from misalignment between the natural body’s circadian rhythm and work schedule (shift work disorder). Other conditions that may induce similar clinical presentation of troubles falling asleep and/or sleepiness include jet lag disorder, and irregular circadian rhythm sleep disorders, related to either lack of sleep hygiene. Infrequent free-running circadian sleep rhythm disorder is most frequently seen in blind persons; lack of entrainment of the circadian rhythm results in non-24-hour rhythm.
Treatment
The treatment of chronic insomnia is a significant challenge. It is highly individualized, and no uniform approach can be recommended. The physician should first identify any underlying conditions, which may include psychiatric disorders such as depression, alcohol or substance abuse, chronic medical disorders, sleep apnea, aging, and alteration in the circadian rhythm. Treatment then should be based on concurrent problems, age, and hepatic and renal function. The mainstay of treatment is the exploration and correction of maladaptive nighttime behaviors. This behavioral therapy, typically involving a series of meetings with the managing physician or therapist can be supplemented with carefully chosen, typically short-term, pharmacological therapy. Specific interventions that are typically used in this setting are discussed below.
▪ SPECIAL CLINICAL POINT: In treating sleep-onset delay, pharmacologic treatment should be used judiciously and should be combined with nonpharmacologic treatments.
Counseling plays an important role in the therapy of sleep disorders. If the physician spends time talking with these patients, he or she may find that they actually are attempting to discuss problems that they find difficult to raise, such as impotence, marital discord, or alcoholism in a family member. The complaint may be resolved if attention is given to these problems, regardless of whether sleep behavior actually is altered.
Sleep hygiene includes setting a fixed hour for retiring each night, eliminating daytime naps, avoiding drinking caffeine-containing beverages and engaging in anxiety-producing activities at night, and ensuring that the bedroom is quiet, dark, and comfortable. Because patients may not think of over-the-counter preparations as drugs, mentioning the need to avoid sympathomimetic substances may prove fruitful. Physical exercise is advised, if taken at least a few hours before bedtime.
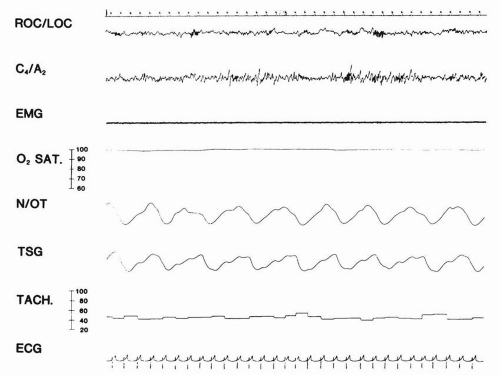
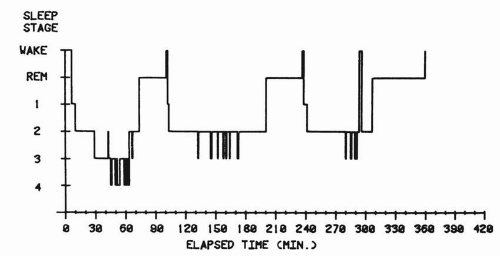
Only a few practical points concerning
behavioral therapies need to be reviewed here. Techniques that attempt to increase relaxation, either through biofeedback or more conventional learning paradigms, may be valuable if they are aimed at a specific physiologic disturbance. For example, a patient whose PSMG indicates a large amount of muscle activity prior to falling asleep might benefit from EMG biofeedback. These techniques generally will
require the facilities of a sleep laboratory. Attempts at operant and classic conditioning as aids in treating insomnia also have had some limited success. A widely accepted behavioral modification technique—stimulus control—is especially useful in correcting maladaptive association of arousal with bedtime routine. Other techniques aimed at reducing tension include progressive muscular relaxation and autogenic training.
Sleep restriction relies on restricting time spent in bed to the estimated sleep time the patient accumulates during the night, as documented by sleep logs, and then gradually increasing it until an optimal sleep time is achieved. This treatment is based on the observation that insomniacs spend too much time in bed in an attempt to obtain more sleep. Reduction of time spent in bed leads to a state of mild sleep deprivation, which is likely to result in faster sleep onset, improved sleep continuity, and deeper sleep. Stimulus control therapy is a formal set of behavioral advices and entails going to bed only if sleepy, getting out of bed when unable to sleep, using the bed and bedroom for sleep only, arising at the same time every morning, and avoiding naps.
Cognitive therapy focuses on maladaptive thoughts that produce an emotional arousal, such as unrealistic expectations about sleep requirements, negative consequences of insomnia, and misattributions of daytime difficulties to poor sleep.
Pharmacologic treatment can be used in the management of insomnia; however, the use of medications must be considered carefully. These medications are most helpful when their use is self-limited, such as during acute hospitalization or as part of a more comprehensive program of sleep hygiene. In the latter case, they may allow the physician time to explore the roots of the sleep disturbance more thoroughly and implement behavioral treatments.
The choice of a sedative agent is dictated primarily by the duration of clinical sedation; ideally, the hypnosedative effect should cease by the time the patient arises. An effective hyp notic drug should decrease sleep latency and increase the total sleep time. The value of a hypnotic depends on the balance of its efficacy and side effects. The efficacy is defined by its ability to induce and maintain sleep, and it directly depends on the drug’s dose, absorption, and duration of action. Thus, an efficacious hypnotic is absorbed rapidly and has duration of action consistent with the sleep period (usually around 8 hours). Ideally, such a hypnotic has no adverse effects. However, hypnotics with duration of action that exceeds the sleep period usually lead to residual sedation during daytime. In contrast, use of short-acting hypnotics in doses higher than required often is associated with major adverse effects such as rebound insomnia and anterograde amnesia. Dependence is also an undesirable possibility with the use of hypnotics. This possibility can be minimized by the intermittent use of low doses, together with limited duration of drug intake and gradual withdrawal if treatment has been continuous for more than a month. The available drugs have a surprisingly heterogeneous set of effects on sleep architecture.
Although almost all agents used as hypnosedatives will suppress REM sleep when given in sufficiently large quantities, two patterns of effects are seen at lower doses. Barbiturates, chloral hydrate, anticholinergics, tricyclics, and ethanol demonstrate REM suppression, whereas most benzodiazepines decrease stage N3 sleep. They all appear to decrease sleep latency and reduce the number of spontaneous awakenings. Although the drugs that have the least effect on sleep architecture may offer a theoretic advantage in the therapy of insomnia, there is no clear demonstration that they induce “better” sleep. Data on commonly used sleep-promoting medications and some miscellaneous agents are summarized in
Table 10.1.
Sleep latency usually is decreased with these agents, and there is seldom a reason to use more than a single agent in the treatment of insomnia. A failure to obtain an adequate response on the first night does not imply a need to increase the dosage immediately; a trial of at least two
or three nights is indicated. Sleep induction is related to the rate of drug absorption. Sleep maintenance is related to dosage and half-life. The timing of the intake of the medications is, therefore, important. Hypnotics with longer half-lives (lasting more than 24 hours) show increased efficacy with two or three nights of administration, but they also show increased residual daytime effects. Some benzodiazepines, such as flurazepam, produce persistent long-acting metabolites and cause definite impairment in alertness, motor performance, and cognitive function in the morning. Because of the intrinsic “tapering” effect of compounds with long halflives, rebound and/or withdrawal phenomena appear to be unlikely; when they do occur, such effects are delayed in onset and are relatively mild. However, there is a much higher likelihood of rebound or withdrawal effect after abrupt discontinuation of short-half-life hypnotics, for which dose tapering is appropriate. When the initial therapy is unsuccessful, changing classes of medications may be useful.
In the last two decades, sleep medicine has seen an almost complete replacement of barbiturates by benzodiazepines, followed by an introduction of nonbenzodiazepine hypnotics in place of benzodiazepines. Only five benzodiazepines are currently marketed for hypnotic purposes in the United States: triazolam, temazepam, quazepam, flurazepam, and estazolam. Various benzodiazepine anxiolytics (e.g., diazepam, alprazolam, lorazepam, or oxazepam) also are prescribed for insomnia associated with anxiety disorders. Unfortunately, there is limited evidence to support their efficacy for these disorders. The drug of choice for sleep-onset insomnia differs from that for sleep-maintenance insomnia (i.e., triazolam for the former, and temazepam for the latter).
Onset of action after an oral dose depends on rapidity of absorption from the gastrointestinal tract. Duration of action of a single dose of a benzodiazepine hypnotic depends on its distribution (e.g., it may concentrate in sites such as adipose tissue, where it exerts no pharmacologic activity) and on elimination and clearance. With repeated administration at a fixed dosing rate, a drug will accumulate in plasma and brain until a steady state is reached. Time necessary to reach a steady-state condition depends only on the drug’s elimination half-life. For a drug such as triazolam with a very short elimination half-life, accumulation will be complete within 1 day;
that is, the mean plasma concentration will be no higher after multiple days of therapy than after the first day. At the other extreme is a drug such as flurazepam, with its principal active metabolite desalkylflurazepam. This compound has a very long elimination half-life; 2 weeks or more of long-term treatment will be necessary for a steady state to be attained. The rate of drug disappearance following discontinuation after long-term treatment will mirror the rate of accumulation (i.e., the longer the elimination halflife, the more time will be needed for the drug to disappear). A potential benefit of accumulating a benzodiazepine is that persistence of drug at the receptor sites throughout each 24-hour dosing interval increases the likelihood of a daytime anxiolytic effect, a potential benefit for patients with both anxiety and insomnia. For short halflife hypnotics such as triazolam, however, increased daytime anxiety has been reported in some studies, possibly attributable to wide fluctuations in plasma and receptor-site concentrations between doses. Estazolam, a relatively new benzodiazepine, remains effective as a hypnotic for at least 6 weeks of continuous administration at a dosage of 2 mg at bedtime, with no evidence of clinically significant tolerance. It improves sleep latency and total sleep time, reduces the number of nocturnal awakenings, and improves both depth of sleep and sleep quality in adults with chronic insomnia.
▪ SPECIAL CLINICAL POINT: In the last decade, several nonbenzodiazepine hypnotics have become the most commonly prescribed medications for insomnia. Their main advantage compared to the benzodiazepines is their favorable side effect profile, less potential for residual daytime effects, and less potential for abuse.
Zolpidem, and its slow-release formulation, is a benzodiazepine receptor ligand structurally unrelated to benzodiazepines (an omega 1-selective nonbenzodiazepine hypnotic). It has an elimination half-life of 3.5 to 5.1 hours (mean, 4 hours). In young adults, zolpidem leads to a marked increase in slow wave sleep, with reduction of N2 and no change in REM sleep. In middle-aged patients, there is a reduction of wakefulness after sleep onset (WASO) time and increase of N2 sleep, without changes in REM sleep.
Zaleplon is a nonbenzodiazepine hypnotic from the pyrazolopyrimidine class. It interacts with the GABA-BZ receptor complex, selectively on omega-1 receptor on the alpha subunit of the GABA A receptor complex. In controlled trials it shortened sleep latency. It is metabolized by aldehyde oxidase and to a lesser degree by CYP 450 3A4. Inhibitors of these enzymes may decrease its clearance and enhance sedative/hypnotic effect. Due to its short half-life of only 30 minutes, it may be used for initial as well as maintenance insomnia.
Eszopiclone is a cyclopyrrolone compound, a nonbenzodiazepine hypnotic that has been approved by the U.S. Food and Drug Administration (FDA) for treatment of insomnia. It has an onset of action of 1 hour and half-life of about 6 hours. Eszopiclone has been shown to decrease sleep latency and improve measures of sleep continuity. It has not been associated with the development of tolerance over 6 months of use.
A structurally new compound with a distinct mechanism of action was recently introduced in treatment of insomnia. Ramelteon is a nonsedating melatonin receptor agonist that is rapidly absorbed from the GI tract, gives a peak concentration at 0.5 to 1.5 hours and has the half-life of 1 to 2.5 hours. It then undergoes extensive liver metabolism, yielding weak, active metabolites that have an elimination halflife of 2 to 5 hours. Ramelteon produces modest shortening of sleep latency.
Precautions
Patients who are pregnant, who are alcoholic, or who have sleep apnea should not be given hypnotics, except in low doses and only in special circumstances. Preference for nonbenzodiazepines over benzodiazepines is based on the former’s lower toxicity and potential for abuse. The prescribing of hypnotics to children is not recommended, except for rare use in the
treatment of night terrors or severe somnambulism. Benzodiazepine metabolism varies and is largely age dependent. The elimination halflife of diazepam in healthy men may increase threefold to fourfold from 20 years of age to 80 years of age. The elimination of hypnotics is decreased in elderly people who might have a low renal glomerular filtration rate, a reduced hepatic blood flow, and a decreased activity of hepatic drug-metabolizing enzymes. The choice of hypnosedatives for elderly patients with sleeponset delay, especially when they are acutely hospitalized, is complicated by the risk of a paradoxical excitation at nighttime (sun-downing), which may be precipitated or exacerbated by medication. Although diphenhydramine has been useful in many of these patients, there is a risk of increasing their confusion because of its anticholinergic effect. These problems can be minimized by adjunctive measures, such as leaving a light on in the patient’s room, and by frequently reorienting the patient to the unfamiliar surroundings. A family member occasionally may be required to stay with the patient.
Because of the intrinsic “tapering” effect of long-half-life compounds, rebound and withdrawal phenomena appear to be unlikely; when they do occur, such effects are delayed in onset and are relatively mild. However, there is a much higher likelihood of rebound or withdrawal effect after abrupt discontinuation of short-half-life hypnotics, so dose tapering is appropriate.
Although many of these drugs, especially the benzodiazepines, have been marketed with emphasis on their short duration of action, many have long-acting active metabolites. This is often a problem in the patient who experiences a decrement in liver function. Sedative effects are additive and may convert what would have been a mild metabolic encephalopathy into a coma days after the initiation of treatment.
Non-benzodiazepine hypnotics are generally better tolerated and associated with fewer side effects. Dizziness, hypersomnolence, and headache are the most common side effects of zolpidem, zaleplon, and eszopiclone. Zolpidem has been associated with complex behaviors in sleep, including sleep eating. Patients taking eszopiclone may report an unpleasant taste in the mouth.
Alternative Therapies
The most popular and well-studied herbal treatment of depression is St. John’s wort (Hypericum perforatum), a remedy used for wound healing, sedation, and pain relief. Its use as a hypnotic has not been studied systematically, but it may promote “deep sleep” and prolong REM latency.
Valerian root (Valeriana officinalis) has been used widely for its hypnotic properties. A limited number of human studies suggest that valerian could be used as a mild hypnotic with minimal side effects. It seems to affect GABA metabolism and reuptake, mainly GABA A receptors, 5HT-1a, and adenosine receptors. Numerous herbs are used in combinations by traditional Chinese medicine. However, there are no well-designed studies to document their effectiveness and safety.
Anxiety disorders often are linked to insomnia. Anxiety may respond to kava kava (Piper methysticum). Its mechanism of action is thought to involve GABA A receptors.
Melatonin is used to reset the circadian clock and help proper positioning of the sleep cycle within a 24-hour period, but it also has a mild direct sedative-hypnotic effect (the most common doses are 2-10 mg 30 minutes to 2 hours before bedtime). Caution should be exercised in patients with known cardiovascular disease because melatonin reportedly causes vasoconstriction in coronary and cerebral arteries of rats. Other possible side effects are inhibition of fertility, increased depression or induced depression, suppression of male libido, retinal damage, and hypothermia. Melatonin’s interactions with other drugs are not fully understood, which is of particular concern in the elderly population. As with other dietary supplements, there is a concern about purity of the product. Catnip
(Nepeta cataria) is used as a
“tonic” for sleep, as is chamomile
(Marticaria recutita). Several other herbs are used as sleep aids because of their reported sedative effects: gotu cola
(Centella asiatica), hops
(Humulus lupulus), lavender
(Lavandula angustifolia and others), passionflower
(Passiflora incarnata), and scullcap
(Scutellaria lateriflora). Hepatoxicity was described for scullcap when used in combination with valerian root, but this may have resulted from substitution of a particular herb with species of germander
(Teucrium).The FDA recalled all products of L-tryptophan in the United States, but it still is manufactured worldwide. It has resurfaced in the form of 5-hydroxytryptamine. It was found that the new product contains the same impurities previously found in L-tryptophan responsible for eosinophilia-myalgia syndrome. L-tryptophan also is found in some protein supplements.