Chapter 111 Sleep in Patients with Asthma and Chronic Obstructive Pulmonary Disease
Nocturnal Asthma
The airways of asthmatic patients are hyperresponsive. Bronchoconstriction can follow exposure to allergens (pollen, animal dander) or nonallergenic stimuli (e.g., viral infections, low environmental temperature, fumes). In many patients, asthma is worse at night or in the early morning, causing cough, wheeze, or breathlessness. These symptoms reflect overnight bronchoconstriction, which occurs in more than two thirds of asthmatic patients.1
I have observed the fit always to happen after sleep in the night. … At first waking, about one or two of the clock in the night, the fit of asthma more evidently begins, the breath is very slow … the diaphragm seems stiff and tied. … It is not without much difficulty moved downwards.2
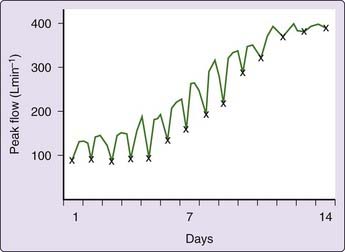
The forced expiratory volume in 1 second (FEV1) and peak flow rates fall overnight in patients with asthma,3 the fall being more than 50% in some patients. Patients with such overnight bronchoconstriction have been called morning dippers (Fig. 111-1).4 In asthmatic patients recovering from exacerbations, about one third have bronchoconstriction during the night and another third have bronchoconstriction before sleep and continue to have it overnight.1 Thus, two thirds of such patients have their lowest flow rates between 10 PM and 8 AM, with a mean amplitude of variation of peak flow rates of 29%.1
Circadian Rhythm of Airway Caliber
Most normal people also have circadian changes in airway caliber, with mild nocturnal bronchoconstriction.5 The largest series comparing circadian changes in peak flow in healthy subjects and unstable asthmatic patients5 shows that the changes in flow rate are synchronous in asthmatic and normal subjects, whereas the amplitude of peak flow rate changes is far greater in asthmatic patients (50%) than in normal subjects (8%). Thus, nocturnal bronchoconstriction in asthma appears to be an exaggeration of the normal circadian changes in airway caliber. Asthmatic patients are hyperreactive to constrictor stimuli; thus, nocturnal bronchoconstriction in asthmatic patients is probably an expression of hyperresponsiveness to the factors that produce mild nocturnal bronchoconstriction in normal subjects.
As with other circadian rhythms, the major synchronizing factor is sleep, although overnight sleep deprivation reduces, but does not abolish, nocturnal airway narrowing (Fig. 111-2).6,7 In asthmatic shift workers, sleep time determines the timing of “nocturnal” airway narrowing,8 and airway caliber changes rapidly invert with inversion of sleep pattern. That some overnight airway narrowing persists even if patients are kept awake all night could be due to a lag between altered sleep times and readjustment of circadian rhythms.
Pathogenesis of Nocturnal Airway Narrowing
Factors that have been suggested but that seem unlikely primary causes of nocturnal airway narrowing include the sleeping posture, interruption of bronchodilator or other treatment, and allergens in bedding. Posture is not a major factor because patients who lie in bed throughout the 24-hour period continue to exhibit overnight bronchoconstriction,3 and lying down does not produce sustained bronchoconstriction.9 Neither is the treatment interval critical, because regular spacing of treatment throughout the 24 hours does not abolish nocturnal bronchospasm,4 and nocturnal wheeze is a presenting complaint of many untreated asthmatic patients.
Allergens
It is unlikely that allergens in bedding are prime causes of nocturnal asthma, because avoidance of such allergens does not abolish nocturnal airway narrowing.10 In addition, overnight bronchoconstriction occurs in both allergic and nonallergic asthmatic patients1 and in normal subjects.5 Allergic factors can, however, produce nocturnal wheeze; experimental allergen inhalation can cause bronchoconstriction on subsequent nights,11 and scrupulous exclusion of allergens can reduce circadian changes in peak flow rates and the frequency and severity of asthmatic attacks.12
These findings suggest that allergic reactions—and particularly, perhaps, late or delayed allergic reactions—are important in the development of nocturnal wheeze in some patients. There is a close relationship between the extent of nocturnal airway narrowing and the degree of airway twitchiness or bronchial reactivity.13 It seems likely that such allergen exposure increases bronchial reactivity in predisposed patients and thus might result in enhanced nocturnal bronchoconstriction.
Airway Cooling
Cold, dry air causes bronchoconstriction in asthmatic patients. It had been suggested that nocturnal asthma might be caused either by breathing cooler air at night or by bronchial wall cooling as a result of the overnight decrease in body core temperature. However, overnight bronchoconstriction persists in normal subjects even when temperature and humidity are maintained throughout the 24-hour day at levels present during diurnal wakefulness.14 However, it has been reported that breathing warm, humid air (36° C to 37° C, 100% saturation) overnight, compared with breathing room air (23° C, 17% to 24% saturation) overnight, abolished nocturnal bronchoconstriction in six of seven asthmatic patients in whom sleep was not documented.15
Gastroesophageal Reflux
There seems to be a high incidence of gastroesophageal reflux (GER) in people with asthma, especially in those with nocturnal wheeze,16 and the GER may be clinically silent. There is no convincing evidence that spontaneous GER causes nocturnal bronchoconstriction.17 Gastric acid suppression with proton pump inhibitors has at best a marginal effect on nocturnal asthma.16,18,19
Bronchial Hyperreactivity
Bronchial responsiveness to inhaled histamine and allergens increases throughout the night.20 However, the airways are narrower at this time, and thus the increased response could reflect greater initial bronchomotor tone at night rather than any change in mucosal permeability or receptor or neuromuscular function. A skin prick test for allergens and histamine shows marked circadian variation: Maximal effects are in the late evening, and a minimum is reached by early morning.21 Thus, there may be circadian variations in reactivity, although the changes in sensitivity to skin tests are about 8 hours ahead of the circadian changes in airway reactivity.
Is Nocturnal Wheeze Related to Sleep Stage?
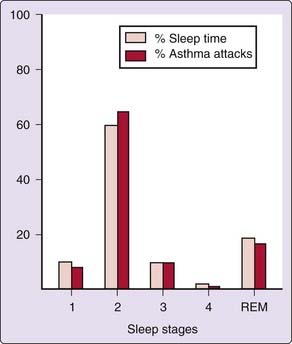
Several groups have recorded electroencephalograms (EEGs) in sleeping asthmatic patients and noted the stage when patients awoke with attacks of asthma. A suggestion that patients awoke more often from REM sleep than would be expected by chance has not been confirmed, asthmatic attacks being randomly distributed throughout the stages of sleep in proportion to the amount of time spent in each sleep stage (Fig. 111-3).22 Esophageal pressure measurements suggest that pulmonary resistance does not differ between sleep stages.7 It thus appears unlikely that there is any difference in the degree of airway narrowing between sleep stages.
Breathing Patterns during Sleep
Like normal subjects,23 asthmatic patients decrease their ventilation from wakefulness to sleep, ventilation being lower during NREM sleep than during wakefulness, with the lowest levels tending to occur in REM sleep.24 Whether there is any abnormality of breathing pattern during sleep in asthmatic patients is unclear. We found a small, but significant increase in irregular breathing in asthmatic patients due almost entirely to more apneas in asthmatic patients,25 but others found no such changes.24 The increased number of apneas that we observed might have been the result of the study’s having been performed in the early summer, when the patients might have had mild rhinitis, which can increase apneas. In addition, the apneas were few and brief and were not associated with significant hypoxemia; thus, their clinical significance is dubious.
Lung volume falls during sleep, and this could contribute to increasing resistance to airflow because lower airway caliber drops as lung volume decreases. However, this is not a major cause of sleep-related airway narrowing.26
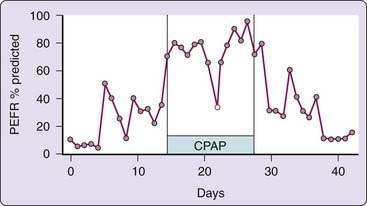
There is some evidence that smaller airways may be preferentially narrowed at night in nocturnal asthma.27 However, the cause and the significance of this observation are clear. Some nocturnal asthmatic patients who snore or have obstructive sleep apnea develop worsening of their asthma, perhaps as a reflex response to their upper airway vibration. This appears to be a relatively uncommon cause of nocturnal asthma, but it is important that it is recognized, because nasal continuous positive airway pressure (CPAP) therapy may be helpful in such cases (Fig. 111-4).28
Relationship between Nocturnal Asthma and Obesity
There has been speculation that asthma is directly related to obesity and thus might be commoner in patients with the obstructive sleep apnea–hypopnea syndrome. However, the evidence of an association between asthma and obesity is still conflicting, with some evidence suggesting the “association” is due to increased awareness of breathlessness in the obese, whereas some studies suggest an increase in airways hyperreactivity in obese subjects.29,30 Further studies are needed to clarify the relationship.
Mechanisms Narrowing Asthmatic Airways at Night
Autonomic Function
Parasympathetic Nervous System
Parasympathetic tone is increased at night. Studies using cholinergic blockade31,32 indicate that an increase in airway parasympathetic tone contributes significantly to the development of nocturnal asthma.32 However, increased vagal tone does not account for all the nocturnal airway narrowing.32
Sympathetic Nervous System
There have been no studies of intrinsic sympathetic tone in nocturnal asthma. The bronchodilator response to infused epinephrine is unchanged at night,33 and thus circadian changes in beta-adrenergic receptor sensitivity cannot explain nocturnal asthma.
Nonadrenergic, Noncholinergic Nervous System
The other autonomic nervous system affecting the airway is the nonadrenergic, noncholinergic bronchodilating system. The precise role of this nervous system and the neurotransmitters involved are still unclear. However, there is some evidence that the activity of this bronchodilating system is impaired in the early morning,34 and this might contribute to tipping the balance of airway caliber toward the development of overnight bronchoconstriction.
Circadian Variation of Hormones
Cortisol
Nocturnal breathlessness in asthmatic patients is most marked when the urinary excretion of 17-hydroxycorticosteroid is at its nadir and peak flow rates parallel changes in the levels of circulating steroids.1 This relationship is not causal; overnight falls in peak flow rate remain unchanged if plasma levels of 11-hydroxy-corticosteroids are kept constant by infusion of hydrocortisone. In addition, therapy with large doses of steroids does not abolish morning dipping.3 Thus, it seems that circadian changes in circulating cortisol levels are not important in the pathogenesis of nocturnal bronchoconstriction.
Catecholamines and Other Mediators
Circulating catecholamine levels show diurnal changes, with a nocturnal nadir. Urinary catecholamine excretion falls to a minimum coincidental with the lowest peak flow rates in some patients.35 However, catechol infusion does not abolish nocturnal airway narrowing.36
Airway Inflammation
Despite considerable interest, there is conflicting evidence whether there are consistent changes in airway inflammatory cell populations or mediators in nocturnal asthma.37–44 Increased inflammatory cells in bronchoalveolar lavage specimens at 4:00 AM have been found in some,39,40 but not all37,43,45 studies. Bronchial biopsies at 4:00 AM showed no change in cell populations.39,43 Further, there is no evidence of any causal relationship between changes in inflammatory cell numbers and nocturnal airway narrowing.39,43,45 One study has suggested a correlation between the FEV1 at 4:00 AM and CD4+ cells in alveolar tissue38 but no causative role has been established. Increases in bronchoalveolar lavage cytokines, eosinophil cationic protein39 and IL-1β44 have been found in some studies. There is no evidence of increased expression of vascular adhesion molecules at 4:00 AM in patients with nocturnal asthma.41 Thus, this confusing situation could be summarized by stating that some inconsistent changes in inflammatory markers have been found overnight in the lungs of patients with nocturnal asthma, but their relevance is not yet clear. Similarly, there is no clear link between obesity-related systemic inflammation and inflammation related to either nocturnal asthma or obstructive sleep apnea.
Clinical Features of Nocturnal Bronchoconstriction
Nocturnal bronchoconstriction and wheezing cause inconvenience and disturbed sleep and probably also hypoxemia and death. Nocturnal symptoms are still being overlooked by patients and physicians46,47 and must be actively sought to minimize the harm caused.
Sleep Disturbance
The major complaint of patients with nocturnal wheeze is that their sleep is interrupted and that they might feel tired in the daytime (Video 111-1![]() ).47,48 This sleep disruption has been confirmed by EEG studies.22,49 The sleep disruption probably impairs daytime cognitive function in patients with nocturnal asthma in comparison with age- and education-matched normal subjects.49 There was no evidence that the observed impairment resulted from drug therapy.49 Indeed, treatment of nocturnal asthma has been reported to improve cognitive function, but this improvement could have been due to increased familiarity with the tests used to assess neurocognition.50 Nevertheless, the potential damage to daytime cognitive function, work, and school performance caused by nocturnal sleep disruption underlines the importance of improving therapy in patients with nocturnal asthma.
).47,48 This sleep disruption has been confirmed by EEG studies.22,49 The sleep disruption probably impairs daytime cognitive function in patients with nocturnal asthma in comparison with age- and education-matched normal subjects.49 There was no evidence that the observed impairment resulted from drug therapy.49 Indeed, treatment of nocturnal asthma has been reported to improve cognitive function, but this improvement could have been due to increased familiarity with the tests used to assess neurocognition.50 Nevertheless, the potential damage to daytime cognitive function, work, and school performance caused by nocturnal sleep disruption underlines the importance of improving therapy in patients with nocturnal asthma.
Death
Fortunately, deaths from asthma are uncommon, but there are more deaths from asthma per hour at night than by day.51 When subdivided according to place of death, there was an excess nocturnal rate for the 146 deaths that occurred at home (P < 0.05), and the same trend was seen for the 73 deaths occurring in hospital (0.15 > P > 0.10). The death rate is, of course, higher at night than by day in the general population, but this averages only a 5% increase between midnight and 8 AM, in contrast to the 28% increase observed in these asthmatic patients.51
Excess nocturnal mortality could result from many factors, including the inability of hypoxia,52 hypercapnia,53 or increased airflow resistance54 to awaken sleeping subjects rapidly, with resultant delays in taking treatment; reluctance to summon family or medical help at night; and delay in the arrival of medical assistance. Eight of 10 ventilatory arrests in asthmatic patients in the hospital occurred in the early morning,55 suggesting that unavailability of medical assistance is not a major factor.
One of the most important causes of nocturnal death seems to be nocturnal bronchospasm. The two asthmatic patients who died at night during a prospective study were both morning dippers,56 which suggests that nocturnal bronchoconstriction can be life threatening. Thus, the morning dip pattern of asthma should be sought and recognized as potentially dangerous when it is marked in patients with unstable asthma.
Treatment
Nocturnal bronchoconstriction is a sign of inadequately controlled asthma, and the new development of nocturnal wheeze in a patient must be regarded as a dangerous sign requiring monitoring and urgent treatment. Nocturnal wheeze often responds to increasing conventional daytime maintenance treatment with either prophylactic agents or bronchodilators, and recent evidence indicates that inhaled steroids can help overnight airway narrowing within 12 hours.57 Only when optimal daytime control does not abolish nocturnal symptoms should additional treatment be directed at nocturnal wheeze.
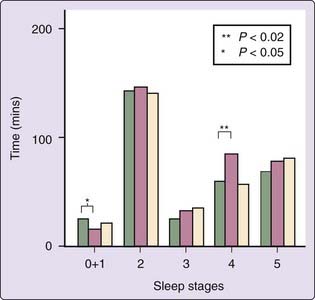
In patients for whom these treatments are insufficient, long-acting bronchodilators—either inhaled or oral—should be used. Salmeterol improves symptoms, overnight peak flow rates, and sleep quality58 and also quality of life59 in nocturnal asthma (Fig. 111-5). Formoterol, another long-acting inhaled agent, has been shown to improve overnight lung function.60
In terms of oral bronchodilators, there appears to be little to choose, from the bronchodilation point of view, between oral theophyllines61 and oral beta2 agonists.62 Both can markedly reduce nocturnal symptoms, and the choice will largely be determined by whether the patient develops side effects. These agents can often be taken effectively once a day immediately before going to bed, thus reducing daytime side effects.61 Theophylline absorption tends to be lower at night than in the morning. This is not due to diurnal variations in theophylline absorption or disposition but probably results from differences between nocturnal and morning gastric content, physical activity, and posture. However, it is important to be aware of this difference, because larger dosages can be given at night.
Oral theophylline can disturb sleep, as judged by the EEG in patients with nocturnal asthma, despite improving nocturnal symptoms and overnight changes in flow rates.63 However, there was no evidence of sleep disturbance in a medium-term study of normal subjects taking theophylline.64
There have been relatively few studies comparing long-acting inhaled beta2 agonists with other agents in the management of nocturnal asthma.65,66 One study showed no major difference in efficacy between salmeterol and oral theophylline, although there were marginal benefits in favor of salmeterol in terms of frequency of arousals from sleep and improved quality of life.65 Another study showed that salmeterol resulted in less deterioration in nighttime lung function and improvement in subjective sleep quality compared with theophylline.66 Salmeterol was superior to oral slow-release terbutaline in terms of the number of nights free of awakenings, morning peak flow rates, and assessment of clinical efficacy.67 Salmeterol 50 µg twice daily was similar in efficacy to fluticasone 250 µg twice daily in improving nocturnal asthma.68 Inhaled long-acting bronchodilators have taken over from oral long-acting bronchodilators, as side effects are fewer.69 However, the U.S. Food and Drug Administration requires that, for safety reasons, long-acting beta agonists be used in combination with inhaled corticosteroids.69a
The role of proton pump inhibitors remains unclear.18,16 Their continued widespread use constitutes, at best, a non–evidence-based approach.
In the small minority of asthmatic patients whose nocturnal airway narrowing relates to their snoring or obstructive apneas, weight loss, if appropriate, and CPAP should be tried.28 In my experience and that of others,70 such therapy does not often improve nocturnal asthma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree