Chapter 130 Smoking and the Spine
Tobacco is responsible for one in five deaths, and tobacco use is the single largest preventable cause of death and disability in the United States.1 Smoking has been linked to numerous health conditions, including cancer, respiratory disease, cardiovascular disease, and peripheral vascular disease1; however, the delayed onset of these diseases makes it difficult for users to realize the potential consequences of tobacco use until significant damage has been done. The addictive properties of tobacco use, both chemical and psychological, make cessation difficult for even the most determined quitter. Despite numerous public health efforts, tobacco use continues to have significant adverse effects on the health of people everywhere.2
Tobacco use affects the entire body and has been identified as a risk factor for six of the eight leading causes of death in the world: malignancies, heart disease, cerebrovascular disease, lower respiratory infections, chronic obstructive pulmonary disease, and tuberculosis2–5 (Table 130-1). Associated with increased osteoclast and decreased osteoblast activity, smoking has been implicated as a risk factor for osteoporosis, delayed fracture healing, and fusion pseudarthrosis. In general, multiple studies have indicated that spine-related disorders are more common in smokers, and spine surgeries are up to four times more frequent in cigarette smokers.6 Symptomatic fusion pseudarthrosis is believed to be three to five times more common in smokers than nonsmokers.6
TABLE 130-1 Common Adverse Health Effects due to Tobacco Use
| Adverse Effect | Signs |
|---|---|
| Cancer | Lung, trachea, bronchus, oral, esophageal, stomach, liver, pancreatic, bladder, kidney, and cervical cancers; leukemia |
| Cardiovascular | Atherosclerosis, cerebrovascular disease, coronary artery disease, abdominal aortic aneurysm |
| Dental | Implant complications and failure |
| Dermatologic | Advanced skin aging, wrinkles |
| Gastrointestinal | Peptic ulcer disease |
| Immunologic | Infectious disease susceptibility, tuberculosis |
| Ophthalmologic | Cataracts |
| Orthopaedic | Decreased bone mineral density, delayed fracture healing, increased fracture risk |
| Respiratory | Chronic obstructive pulmonary disease, pneumonia, impaired lung development |
| Reproductive | Maternal infertility, miscarriage, low birth weight, still birth, sudden infant death syndrome |
| Spinal | Back and neck pain, prolonged disability, poor surgical outcomes |
| Surgical | Surgical site infections, delayed healing |
Data from Brunnhuber K, Cummings KM, Feit S, et al: Putting evidence into practice: smoking cessation, 2007. www.clinicalevidence.bmj.com/downloads/smoking-cessation.pdf; and Wipfli H, Samet JM: Global economic and health benefits of tobacco control: part 1. Clin Pharmacol Ther 86:263–271, 2009.
Adverse Health Effects of Tobacco Use
Initially linked to lip, mouth, and throat cancers in the 18th and 19th centuries, tobacco use has been shown to result in significant damage throughout the body.7 Typically associated with lung cancer, smoking actually results in more deaths from cardiovascular and respiratory diseases.8 Lung diseases linked to smoking include cancer, bronchitis, emphysema, and a predisposition for pneumonia.1 Injuries to the cardiovascular system resulting from smoking include coronary artery disease, myocardial infarction, cerebral vascular attack, aneurysm, and peripheral vascular disease.1 Coronary artery disease is two to four times more common in smokers than nonsmokers.1 In nonsmokers, exposure to secondhand smoke has been associated with a 25% to 30% increased risk for the development of coronary artery disease.9 Smoking has also been associated with the development of insulin resistance, cataracts, and bacterial infections.1,10,11 Smokeless tobacco has been associated with increased risk of oral cancers, gingival recession, and oral leukoplakia.5
Spine-Specific Consequences of Tobacco Use
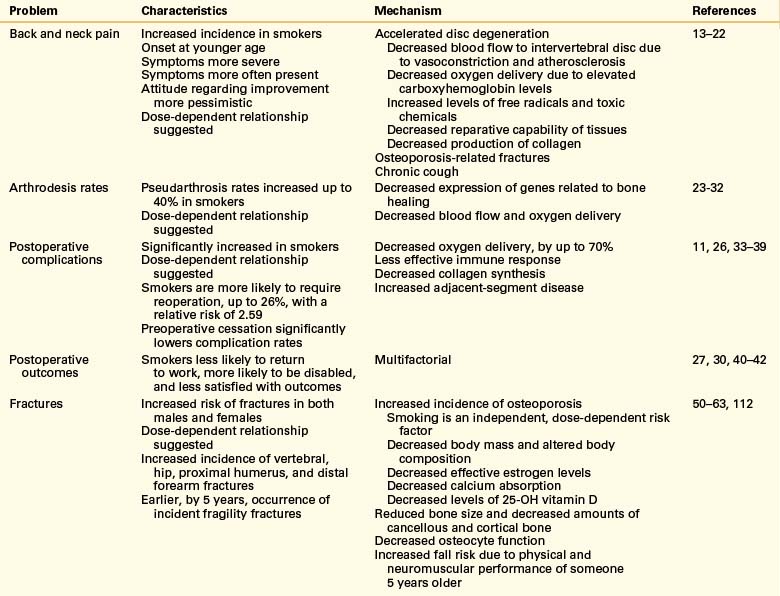
Although smoking has been the form of tobacco use most often studied, any type of tobacco use has been shown to affect the spine adversely in multiple ways (Table 130-2). Not only are tobacco users more likely to have back and neck pain or injuries, they are less likely to have significant improvement following treatment.
Back Pain
An estimated 15% to 20% of adults have at least one episode of low back pain every year, and 50% to 80% experience low back pain at least once in a lifetime.12 Similarly, neck pain is experienced by approximately 20% of the adult population in one year and by 66% of the population in a lifetime.12 A majority of evidence on the epidemiology of neck and back pain indicates that cigarette use is associated with higher rates of pain.13–18 Although authorities have suggested the existence of a causal relationship between smoking and neck and back pain, a relative lack of prospective studies makes it difficult to confirm this theory.
Compared with nonsmokers, smokers who have back pain are often younger, report more severe symptoms, and indicate that the symptoms were present for a larger portion of the day.16 Smokers are also more often extremely dissatisfied by their current health, more likely to report depression, more pessimistic regarding the resolution of their pain, and less likely to show a trend toward improvement following surgery.16 Adolescent smokers are significantly more likely to develop back pain than nonsmokers, with evidence supporting a dose-response relationship.17,18
Disc Degeneration
Degeneration of the intervertebral disc is believed to be pivotal in the development of lower back pain. In addition to the effects of aging, variable dynamic and biologic stresses contribute to disc degeneration.19 Following exposure to nicotine, catecholamine-mediated vasoconstriction results in decreased blood flow to the intervertebral discs.19 Elevated carboxyhemoglobin levels in smokers and the expected presence of free radicals and toxic substances could further contribute to inadequate nutrition of intervertebral disc tissues. Alterations in cell morphology, increased levels of proinflammatory cytokines, decreased glycosaminoglycan levels, and decreased production of collagen with a shift toward production of type I collagen have been demonstrated following exposure of intervertebral disc cells to nicotine.19,20
Chronic cough has been linked to the development of back pain in the general population, and cigarette smokers are three times more likely to have a chronic cough than people who have never smoked or previous smokers.21 Vertebral body or end-plate fractures resulting from smoking-induced decreased bone mineral density are also likely to lead to back pain.22
Fusion
Smoking has been associated with decreased fracture healing rates and increased incidence of nonunion; thus, it is not surprising that smokers also tend to have similar difficulties following arthrodesis procedures.23–30 A rabbit model of intertransverse process fusion found reduced fusion rates in those receiving nicotine up to the day of surgery and a 0% fusion rate in those continuing to receive nicotine postoperatively.31 Nicotine exposure resulted in decreased expression of genes for vascular endothelial growth factor, basic fibroblast growth factor, types I and II collagen, and bone morphogenetic protein (BMP)-2, BMP-4, and BMP-6.32
Following dorsal lumbar fusion procedures, smokers have been found to have pseudarthrosis rates increased up to 40% higher than nonsmokers.26–29 Smokers able to stop prior to surgery and remain abstinent in the postoperative period have improved rates of fusion compared with people who continue to smoke.27 The use of rhBMP-2 has been shown to significantly increase fusion rates in smokers.28 Following surgery, smokers were less likely to return to full-time work, more likely to be disabled, and less satisfied with the outcome.27
Analysis of results from ventral cervical arthrodesis procedures indicate that there is an increased pseudarthrosis rate following multilevel discectomy and interbody grafting using autogenous grafts in smokers compared with nonsmokers.30 The clinical outcome is significantly better for nonsmokers than smokers.30
Surgical Complications
Surgical site infections have been reported to be more common in smokers following spine surgery,33 and chronic hypoxia decreases collagen synthesis and deposition in healing wounds.34,35 Published results are mixed, but smoking has also been suggested as a risk factor for the development of deep venous thromboses following surgical procedures.36
Tissue oxygenation is compromised in smokers due to multiple factors, including increased levels of carboxyhemoglobin, atherosclerosis, and vasoconstriction. Subcutaneous tissue oxygen tension begins to decrease 10 minutes after initiation of cigarette smoking, reaches a low of 22% to 48% below baseline after approximately 30 minutes, and remains below normal for up to one hour.35 The combination of nicotine-mediated vasoconstriction and increased levels of carbon monoxide in smokers results in an estimated 70% decrease in subcutaneous tissue oxygenation in regular smokers.35
The presence of oxygen is crucial for effective prevention of infection,26,34 and smokers have demonstrated increased susceptibility to a number of bacterial infections, including meningitis, periodontitis, otitis media, and infection of the respiratory and urinary tracts.11 Reactive oxygen species produced by neutrophils and monocytes are necessary for effective functioning of the immune system, and levels are decreased in smokers.34 Increased subcutaneous oxygen levels postoperatively result in decreased surgical site infection rates, and smokers quitting smoking 4 to 8 weeks prior to surgery have shown a decreased incidence of surgical site infection.34
Following fusion with segmental fixation for adult spinal deformity, smoking was found to be a risk factor for adjacent-segment problems; the overall relative risk of reoperation for any reason was 2.59 in smokers, with 25.8% requiring another procedure.37 Prior to elective general surgery or orthopaedic procedures, smokers randomized to receive smoking cessation counseling and offered nicotine replacement therapy had cessation rates significantly higher than the control group, up to 58%, and significantly lower postoperative complication rates.38,39 Cessation had the largest effect on reducing surgical site complications.39 The number needed to treat to prevent one complication has ranged from three to five patients.38,39
Overall Outcomes
After surgical procedures for isthmic lumbosacral spondylolisthesis or chronic low back pain, smokers were more likely to be dissatisfied and have worse results.40–42 Patients actively serving in the military were significantly less likely to return to full-time work following a lumbar microdiscectomy if they were smokers.43
Musculoskeletal Consequences of Tobacco Use
General Adverse Effects
The remainder of the musculoskeletal system suffers similar consequences due to tobacco use. Smokers experience decreased rates of healing of fractures, fusions, and tissues, which results in poorer outcomes overall and an increased incidence of posttraumatic and postoperative infections. Postoperative smoking predicts failure of fingertip replantations44 and reduced success of anterior cruciate ligament reconstruction.45 Following tibial and femoral shaft fractures, smokers are more likely to experience delayed union or nonunion than nonsmokers.46,47 Smokers are also at increased risk for rotator cuff tears48 and are likely to have delayed tendon to bone healing following rotator cuff repair based on findings in a rat model.49
Osteoporosis
Smoking has long been associated with the development of osteoporosis and increased risk of fractures. Evidence indicates that smoking is an independent, dose-dependent risk factor for decreased bone density.50,51 This finding is not limited to older patients. A study of young male military recruits found smoking to be a risk factor for decreased spine and hip bone mineral density.52 Research has also shown that smokers have reduced bone size and amounts of cancellous and cortical bone. Estradiol activity is routinely decreased in smokers due to multiple mechanisms. This results in decreased intestinal absorption of calcium and increased risk of osteoporosis.53,54 Smoking-related alterations in body mass and composition, estrogen metabolism, calcium absorption, and osteocyte function are thought to have important effects on bone health.53,54
Smoking is believed to increase fracture risk through multiple mechanisms; low bone mineral density cannot account for the entire increase in risk.55 Effects are seen in both premenopausal and postmenopausal women, although effects are often more significant following menopause and in women with decreased body mass.56,57 Men who smoke are also affected and have been found to have a 4% to 15.3% lower bone mineral density than men who had never smoked.58 Twin studies of same-sex pairs discordant for smoking indicate a possible dose-dependent relationship.56,59
Smokers can have significantly reduced bone mineral density at the lumbar spine, forearm, and calcaneus, with more substantial deficits noted in the hip.50 Smoking has been shown to increase the lifetime risk of vertebral and hip fractures in both men and women who smoke.50,55,57,60–62 Current smoking has also been implicated as a risk factor for proximal humerus and distal forearm fractures.63 Smokers have been shown to be at risk for sustaining fractures up to 5.2 years earlier than nonsmokers, and fracture risk increased as tobacco consumption increased.63 Smoking cessation results in a rapid drop in fracture risk during the first 10 years, but the risk of fracture remains elevated for more than 30 years.63
There is also evidence that smokers may be more likely to fall than nonsmokers due to relative weakness, poorer balance, and impaired neuromuscular performance.54 It has been estimated that smokers have the physical and neuromuscular function of someone 5 years older.54
Epidemiology of Tobacco Use
Worldwide
Tobacco use, which is linked to 100 million deaths in the 20th century and currently accounts for 5.4 million deaths a year, has been classified as an epidemic by the World Health Organization.2 At current rates, tobacco use will result in over 8 million deaths a year by the year 2030 and an estimated 1 billion deaths in the 21st century.64 Tobacco kills one third to one half of all people who use it—one person every 6 seconds—resulting in death approximately 8 to 16 years prematurely65 More than 40% of men and approximately 12% of women smoke tobacco worldwide.4
In the United States
In the United States, cigarette smoking kills an estimated 440,000 people each year. This is more than the number of people killed as a result of car accidents, alcohol abuse, illegal drug use, homicide, and AIDS combined.1 In the 40 years between 1964 and 2004, more than 12 million Americans died prematurely due to smoking-related illnesses. At the current rate, 25 million smokers alive today will die due to the adverse effects of smoking.1 Cigarette-related residential fires result in more than 1000 deaths each year, making cigarettes the number one cause of residential fire fatalities.1
The 2007 National Survey on Drug Use and Health found that 70.9 million Americans 12 years of age and older were current tobacco users.66 As shown in Table 130-3, a majority of these, 60.1 million, were current cigarette smokers.66 The rate of tobacco use varies greatly between age groups, with people 18 to 25 years of age having the highest rate of tobacco use in the previous 30 days, 41.8%.66 Of youths 12 to 17 years of age, 12.4% (3.1 million) had used a tobacco product in the past 30 days.66
TABLE 130-3 Current Tobacco Use among Americans 12 Years of Age and Older in 2007
| Number of People (in millions) | Percent of U.S. Population | |
|---|---|---|
| Cigarette smokers | 60.1 | 24.2 |
| Cigar smokers | 13.3 | 5.4 |
| Smokeless tobacco users | 8.1 | 3.2 |
| Pipe smokers | 2 | 0.8 |
| Any tobacco use | 70.9 | 28.6 |
Data from Substance Abuse and Mental Health Services Administration: Results from the 2007 national survey on drug use and health: national findings, Rockville, MD, 2008, Office of Applied Studies.
Financial Costs
The financial burden of tobacco use on society is overwhelming. It is estimated that tobacco use is directly responsible for more than 96 billion dollars of the U.S. health care budget each year.1 An additional burden of 97 billion dollars annually can be attributed to lost productivity due to tobacco use.1 By not accounting for other costs associated with tobacco use, such as diseases due to secondhand smoke and burns related to tobacco use, the estimated annual cost associated with tobacco use of 193 billion dollars is likely a significant underestimate.1
Secondhand Smoke
Passive, or secondhand, smoke has also been shown to increase the risk of smoking-related illness. It is estimated that approximately 3000 lung cancer deaths and 46,000 deaths from coronary artery disease are due to passive smoke exposure each year.67 Children exposed to tobacco smoke are at increased risk for sudden infant death syndrome and respiratory and ear infections. In addition, they are more likely to develop asthma and to have more severe symptoms.1,9
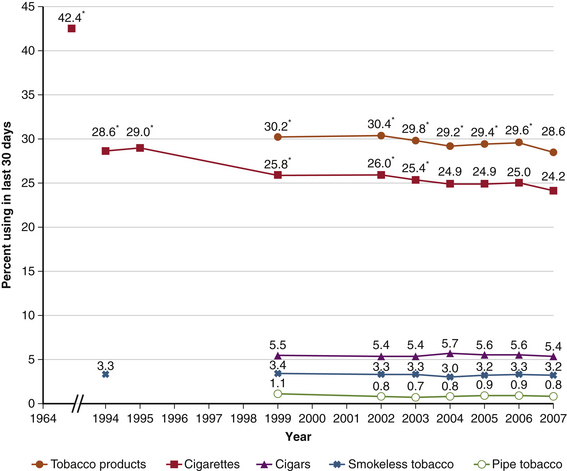
Recent Trends of Tobacco Use
As of 1960, approximately 50% of adult men in the United States were cigarette smokers.4 Since the 1946 release of the Surgeon General’s report on smoking and health, increased awareness of the harms of tobacco use have led to an almost 50% decrease in the number of Americans using tobacco1,66 (Fig. 130-1). Between 2000 and 2007, there was an 18% decline in cigarette sales in the United States. The average price of a pack of cigarettes increased from $2.93 to $3.93 during the same period.68 Although the rates of cigarette use and overall tobacco use by 18- to 25-year-olds decreased from 2002 to 2007, the rates of cigar and smokeless tobacco use slightly increased.66
In 2007, there were approximately 6100 new cigarette smokers 12 years of age and older every day, for a total of 2.2 million new smokers.66 Of these, 59.7% were younger than 18 years of age.66 In that same year, a higher percentage of males than females (53.2% vs. 22.4%) reported tobacco use during the previous 30 days.66
There is significant variability in the rate of tobacco use between the different ethnic groups in the United States. In 2007, the prevalence of past month tobacco use in those 12 years of age and older was 15.4% for Asians, 22.7% for Hispanics, 26.8% for blacks, 30.7% for whites, 35.2% for groups reporting two or more races, and 41.8% for American Indians or Alaska Natives.66 Educational level inversely influences cigarette use, with use decreasing as education increases.66
As of 2006, Utah had the lowest smoking rates, with 10.4% of men and 9.3% of women 18 years of age or older reporting current cigarette use.8 Kentucky had the highest smoking rates, with 29.1% of men and 28.0% of women, for the same period.8
People with mental illness compose one group that has not seen an appreciable decrease in smoking rates. Although smoking rates have been reported near 90% in people with schizophrenia, smoking rates are two to four times greater in people with bipolar disorder, major depression, posttraumatic stress disorder, and other mental illnesses than in the general population.69 People with psychiatric disorders are believed to purchase more than 40% of cigarettes sold in the United States.1
Also associated with increased cigarette use, current illicit drug use was reported in 20.1% of smokers compared with 4.1% of those not currently using cigarettes.66 Similarly, alcohol use was reported by 66.9% of cigarette smokers compared with 46.1% of nonsmokers.66 Cigarette users were also more likely to be heavy drinkers and participate in binge drinking than those not currently using cigarettes.66
A corresponding increase in sales of other tobacco products negated approximately 30% of the decline in cigarette sales. For example, cigar sales increased by 37% from 2000 to 2007,68 and use of noncigarette smoked tobacco products, including bidis, kreteks, and shisha, has also increased.2
Tobacco and Tobacco Smoke
The composition and behavior of tobacco smoke is a complex subject that is not fully understood. The identities, behaviors, and health consequences of many of the components of tobacco smoke have yet to be well defined. Tobacco and tobacco smoke contain approximately 6700 compounds, about 4000 of which have been identified. At least 63 of these compounds are known to be carcinogenic in mammals, and 11 are known to be human carcinogens.70 An average commercially produced cigarette in the United States is filled with 700 mg of tobacco, which contains 10 to 14 mg of nicotine.71,72 Nicotine (C10H14N2, 1-methyl-2-(3-pyridyl)-pyrrolidine) is a naturally occurring plant alkaloid and is responsible for a majority of the addictive properties of tobacco.
Some compounds in tobacco smoke that are considered hazardous include formaldehyde, acetaldehyde, benzene, carbon monoxide, arsenic, isoprene, toluene, acetone, styrene, ammonia, hydrogen cyanide, and vinyl chloride.73 Almost all of the common elements have been identified in tobacco, including a number of radioactive isotopes and free radicals.73 Many, including cadmium, mercury, titanium, and lead, are also found in tobacco smoke. When inhaled, tobacco smoke is an aerosol with a gas phase containing approximately 8% particulate material on a weight basis.74,75 There are approximately 109 to 1010 particles/cm3 in tobacco smoke, with 50% to 90% being retained in the lungs after expiration.73
Although cigarettes are a roll of tobacco wrapped in a substance not containing tobacco, cigars consist of tobacco wrapped in leaf tobacco or in any substance containing tobacco.70 Cigar tobacco is high in nitrate, and the fermenting process unique to cigars converts the nitrate to very high levels of carcinogenic nitrogen-containing compounds.70 Cigar smoke also contains elevated levels of tar, ammonia, nitrosamines, and nitrogen oxides.70 Having a higher pH than cigarette smoke, cigar smoke contains higher concentrations of free nicotine in the particulate and vapor phases.70 This is absorbed through the oral mucosa and does not require the cigar to be lit. Some cigars contain as much tar and nicotine as a pack of cigarettes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree