15 Spinal Biologics
I. Key Points
– Decision making for the choice of bone graft in spinal surgery is important and should be a part of all preoperative planning.
– The inherent qualities—including advantages, disadvantages, and costs—associated with each type of bone graft should be appreciated by the surgeon.
– Host bone bed preparation is key to enabling bone grafts to achieve their intended function of promoting fusion.
II. Description
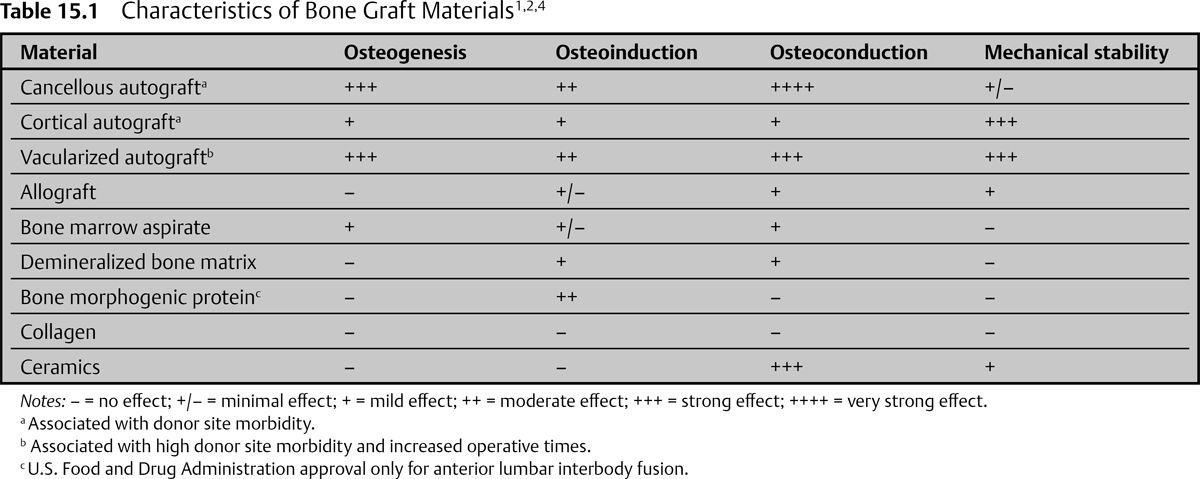
Bone Graft Characteristics (Table 15.1)1,2
– Osteoinduction: the recruitment of mesenchymal cells and the stimulation of these cells to develop into osteoblasts and osteoclasts
– Osteogenesis: formation of new bone by host or graft mesenchymal stem cells transformed into osteoblasts
– Osteoconduction: the scaffolding provided by the graft for the proliferation of new blood vessels and bone
– Mechanical stability: the structural, anatomic, and biomechanical support provided after discectomy, corpectomy, or vertebral tumor resection
– No histocompatibility or disease transmission issues
– Iliac crest (anterior or posterior) is the typical primary donor site.
– Drawbacks
• 20% risk of long-term donor site pain
• Increased surgical risk of blood loss and infection
 Cancellous
Cancellous
 Fulfills all bone graft criteria, except mechanical stability
Fulfills all bone graft criteria, except mechanical stability
 Cortical
Cortical
 Provides superior and immediate mechanical strength
Provides superior and immediate mechanical strength
 Diminished osteoconduction and osteoinduction
Diminished osteoconduction and osteoinduction
 Corticocancellous
Corticocancellous
 Fulfills all of the bone graft criteria
Fulfills all of the bone graft criteria
 Example: tricortical iliac crest wedge
Example: tricortical iliac crest wedge
 Vascularized autograft
Vascularized autograft
 Technically challenging and time consuming
Technically challenging and time consuming
 Very rarely used
Very rarely used
 Consider for host sites that are scarred or irradiated or that span long segments
Consider for host sites that are scarred or irradiated or that span long segments
 Autologous bone marrow
Autologous bone marrow
 Sourceof osteoprogenitorcellsand osteoinductivesubstances
Sourceof osteoprogenitorcellsand osteoinductivesubstances
 Diminished donor site risks
Diminished donor site risks
 Offers no osteoconduction or mechanical stability
Offers no osteoconduction or mechanical stability
Allograft4
– Eliminates risks of autograft harvesting
– Acquired through multiple organ procurement agencies
– Mainly prepared frozen or freeze-dried
– Available in various sizes and types
• Ilium tricortical block, bicortical plug, or unicortical dowel
• Corticocancellous matchsticks or crushed
• Cancellous cubes, block, crushed, bone powder
• Sections from tibia, fibula, or femur
– Drawbacks
• Recommended for use with other types of grafts that may be osteoinductive or osteogenic
• Minimal but present risk of disease transmission
– Prepared by acid extraction, reducing antigenicity but preserving osteoinductive and some osteoconductive properties
– Several formulations
– Putty, gel, chips, granules, or powder
– Primarily to be used as adjunct to other grafting material or graft extender
– Drawbacks
• Increased cost
• Variable efficacy between different preparations
• No mechanical or structural properties
• To be used with patient’s own bone
Bone Morphogenetic Proteins2–5
– Molecules that induce the transformation of mesenchymal stem cells into osteoblasts, capable of inducing ectopic bone formation
– Approximately 20 different bone morphogenetic proteins (BMPs) from the transforming growth factor–β family
– Produced using recombinant DNA technology
– A carrier matrix is necessary to maintain the soluble factor at the graft site, keeping the BMP solution from diffusing within the adjacent tissues.
– U.S. Food and Drug Administration approval only for anterior lumbar interbody fusion (ALIF)
• Recombinant human BMP-2 commercially available as Infuse (Medtronic, Minneapolis, MN)
– Increases fusion rates
– Drawbacks
• Increased cost
• Ectopic bone formation, bone resorption, or remodeling at the graft site is a potential problem if BMP is used in transforaminal lumbar interbody fusion (TLIF), posterior lumbar inter-body fusion (PLIF), or corpectomy applications.
• Hematoma, neck swelling, and painful seroma are potential problems with use in the cervical spine.
Collagen1
– Contributes to vascular ingrowth, mineral deposition, and growth factor binding, improving bone regeneration
– Used primarily as a carrier for other osteoinductive, osteoconductive, or osteogenic materials and as a composite with other graft extenders
– Drawbacks
• Minimal structural support
• Potential immunogenicity
Other Graft Extenders2
– Ceramics
• Tricalcium phosphates, calcium carbonate, and hydroxyapatite
• No risk of disease transmission
• Engineered, biocompatible osteoconductive materials
• Recommended for use only as bone graft extenders
• Combined with autograft, bone marrow aspirate, BMP, or other materials
III. Surgical Pearls
– Decortication and facet joint/end plate preparation, though time consuming, are mandatory for excellent fusion.
– The costs and risks associated with pseudoarthrosis are high; therefore, achieving arthrodesis is of paramount importance.
Common Clinical Questions
1. What are the three principal properties of graft material in relation to fusion?
2. What is the “gold standard” for bone graft material (assuming no contraindications)?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree