Spinal Cord Disorders
Michael Ronthal
▪ MYELOPATHY
Introduction
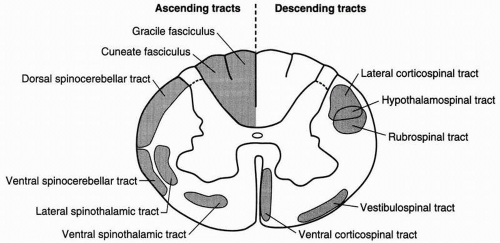
The term “myelopathy” implies dysfunction of the spinal cord, which extends from the craniocervical junction to the level of the L1/2 interspace. The salient feature to suggest cord dysfunction is the presence of bilateral signs or symptoms in the lower limbs, but occasionally a localized intramedullary cervical cord lesion will present with signs or symptoms referable only to the upper limbs, again, usually bilaterally. The clinical diagnosis will depend on a combination of symptoms and signs that suggest root or tract dysfunction (Fig. 16.1). The following discussion excludes acute traumatic spinal cord injury.
Symptoms
Root Related
Motor: Each motor root supplies a group of muscles labeled a myotome. The motor deficit, or weakness, is related to the particular root or myotome involved. Thus weakness in the distribution of C5 may result in the complaint of difficulty lifting objects when the movement requires elbow flexion or difficulty brushing the hair, which requires deltoid action. Weakness in the distribution of C6-7 may result in the complaint of difficulty with pushups when the triceps is weak. Lower cervical root dysfunction results in weak hands.
Sensory: Root pain is typically superficial, sharp, lancinating, shooting down the arm to the hand, or in the thoracic area around the trunk in a girdle distribution. At times the complaint may be of numbness or loss of sensation down the arms or in the hands, but patients rarely report trunk numbness.
Tract Related
Motor: Weakness in the lower limbs results in the complaint of “I can’t walk.” Because of weakness of toe (and also foot) extension the patient may catch the toes and trip, especially when walking on thick rugs. The distal soles of the shoes wear out from constant scraping on the ground with each step, and the patient may be aware of shuffling. Weakness of hip flexion impairs walking up stairs or getting in and out of an automobile.
Sensory: Sensory symptoms depend on which ascending fiber tract is dysfunctional. Posterior column dysfunction may result in deep aching or boring pain caudally. There may be bizarre sensations such as tight garter or stocking sensation in the legs. The fingers may feel “like blown-up sausages.” An occasional complaint is of “water trickling down the leg.” Spinothalamic tract dysfunction may, rarely, result in superficial sharp, root-like pain in the legs. Itching is a pain equivalent. On occasion a pseudo-radicular girdle pain, tight sensation, or sensory loss is due to tract dysfunction in the cervical cord.
Bladder Related
Motor: In upper motor neuron (UMN) bladder dysfunction the bladder is small and contracted. This results in the complaint of frequency of small amounts of urine, nocturia, and, because the bladder is hyperexcitable, urgency and urgency incontinence. Lesions of the thoracic cord may result in bladder dyssynergia—the detrusor contracts on a tight sphincter, with the result of hesitancy.
Sensory: Deafferentation of the bladder leads to a large-volume “sack” with no desire to void and no bladder pain. Ultimately, overflow incontinence occurs. This is termed a tabetic bladder.
Signs
Root Related
Motor: It is fairly easy to detect myotomal weakness in the upper limbs, and the distribution of weakness discloses the root involved. There is considerable overlap; the main muscles involved in particular myotomes are indicated in Table 16.1. With weakness, given time, there is myotomal wasting and sometimes fasciculations, so it is often possible to localize the root level simply by inspection.
Weakness of the abductor digiti minimus (ADM), which abducts the little finger, can be problematic. It may be part of an ulnar neuropathy, but absent a peripheral cause, centrally
mediated ADM weakness is often labeled pseudo-ulnar syndrome generated at cord level, but not at a definite segmental level, and can be seen with lesions as high as C1. This falls into the rubric of false localizing signs.
mediated ADM weakness is often labeled pseudo-ulnar syndrome generated at cord level, but not at a definite segmental level, and can be seen with lesions as high as C1. This falls into the rubric of false localizing signs.
TABLE 16.1 MAIN MUSCLES INVOLVED IN PARTICULAR MYOTOMES | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Weakness in myotome distribution localizes the segmental level of the pathology.
Sensory: The sensory component of root dysfunction is dermatomal, and the dermatomes are illustrated in Figure 16.2. Pinprick, temperature sensation, and light touch sensation are variously involved in an unpredictable manner.
In the upper limbs, dissociated loss of pinprick and temperature sensation, but with retained light touch, suggests central cord dysfunction that could be due to primary pathology in the cord itself or secondary to extramedullary cord compression.
As with hypothenar weakness, dissociated pinprick loss over the hypothenar eminence could be ulnar nerve in origin or it may be a part of the pseudo-ulnar syndrome. If the pinprick level is exactly at the wrist crease, it is more likely to be ulnar nerve in origin, whereas a level above the wrist crease supports root or cord origin.
On the trunk, the finding of a band of sensory loss is referred to as suspended sensory loss and may be secondary to thoracic radiculopathy or is occasionally tract related.
Sensory dysfunction secondary to radicular pathology localizes the segmental level of pathology.
Tract Related
Motor: The lower limbs may be spastic, and clonus at the patella or Achilles tendon is part of the UMN syndrome. The distribution of weakness in the UMN syndrome is all-important in diagnosis. In the upper limbs there is preferential weakness of deltoid, triceps, wrist, and finger extension and finger abduction. In the lower limbs there is preferential weakness of hip flexion, foot and toe dorsiflexion, and hamstring and thigh abduction.
Sensory: Spinothalamic tract (pinprick) sensory loss secondary to cord dysfunction is variable but will result in a “level” either in the legs or on the trunk. As the dysfunction progresses, the level will rise until the radicular segmental level is reached. The normal segment between the tract level and the root level is called a “skip area.” As the level rises, it ultimately reaches the root level of pathology and the skip disappears. The lesson is to never accept trunk or leg level as indicative of the segmental level of pathology until one is sure that there is no more cephalad (radicular) sensory loss. The rising level or skip area is usually attributed to the somatic layering of fiber tracts in the cord, such that, in the spinothalamic tract, the lateral or external part of the tract contains the more sacral or caudal segments and the medial part contains the upper or cervical segments.
Posterior column dysfunction results in loss of position sense in the toes and a characteristic gait—with each step the anterior foot is slapped down, which exaggerates sensory feedback. The Romberg test will usually be positive. Loss of position sense in the fingers indicates a very high cervical cord lesion.
Central cord dysfunction interferes with spinothalamic sensation as the fibers cross over to the contralateral ascending tract, having entered the cord via the dorsal root. Light touch is spared in that a good deal of touch sensory information ascends in the ipsilateral posterior column, thus causing dissociation. Central cord dysfunction is usually seen in the cervical region and affects the cape area, but can occur at any segmental cord level.
Loss of vibration sense at the ankles is common in cord lesions, and if the vibration level is at the costal margin, a cervical pathology is likely. The precise ascending tract for vibratory sense has not yet been established.
Reflexes
In UMN lesions the reflexes are exaggerated below the level of pathology. The plantar reflex can be extensor, but a flexor response in the presence of a multitude of cord signs, as described earlier, should be recorded but does not detract from the diagnosis. An extensor plantar response or Babinski sign indicates a pyramidal tract lesion, but the UMN syndrome is pyramidal and also includes other descending nonpyramidal tracts.
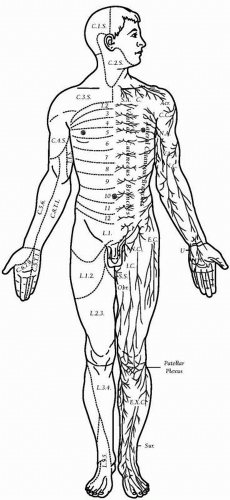 ▪ FIGURE 16.2 Dermatomes (left) and peripheral (right) nerves.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|