The initial management of any trauma patient involves protection of airway, breathing, and circulation. Following initial stabilization, a preliminary neurologic examination should be performed to assess for any signs of injury to the central nervous system. This preliminary neurologic examination involves palpation of the vertebral column to identify step deformities as well as a digital rectal examination to assess for deep sensation and control of the anal sphincter. A more detailed neurologic examination should be performed once the full trauma assessment has been completed.
A patient with spinal cord injury may also have cardiovascular abnormalities, which are important to recognize early. Patients with cervical or high thoracic lesions may have loss of sympathetic innervation and unopposed parasympathetic signaling of cardiovascular functions (
4). This combination of autonomic dysfunction may manifest as hypotension (due to loss of vascular tone), bradycardia, and relative hypovolemia. Prolonged hypotension may lead to injury of other organ systems and may exacerbate secondary injury of the spinal cord (
5). These patients require diligent management through the use of fluid resuscitation and vasopressors to support their blood pressure (
6). In addition to hemodynamic instability, patients with spinal cord injury have a high incidence of respiratory illness. One study suggests that the incidence of respiratory complications in the acute period following spinal cord injury is 50% (
7). Respiratory illness also accounts for a large proportion of deaths observed in the first year following spinal cord injury (
8).
For this reason, protection of the patient’s airway from secretions and gastric contents during the acute period of injury may prevent many of the respiratory complications that occur.
Aside from the initial efforts at resuscitation, current management guidelines mandate proper immobilization and positioning of the patient (
9). All patients with significant trauma, loss of consciousness, pain along the vertebral column, and/or neurologic symptoms should be treated as having a spinal cord injury until proof exists to the contrary. Immobilization of the cervical spine should be maintained using a cervical collar. The patient should also be kept supine, and any transfers should be performed using a backboard. Note, however, that the patient should be removed from the backboard as soon as possible to prevent the formation of decubitus ulcers.
DIAGNOSTIC IMAGING
Imaging studies are of crucial importance to those physicians responsible for managing a patient’s spinal cord injury. However, the timing and extent of imaging is dependent on the extent of traumatic injury to the patient as well as the neurologic examination. Several guidelines have emerged, which serve to inform decisions around the need for diagnostic imaging.
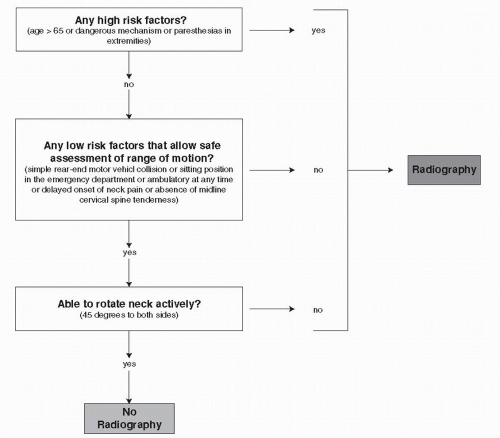
There are two commonly used decision paradigms for determining whether a patient requires radiography of the cervical spine—the Canadian C-spine rules (
10) and the National Emergency X-Radiography Utilization Study (NEXUS) Low-Risk Criteria (
11). The first bases the decision on risk factors for cervical spine injury (see
Fig. 40.1). Another set of guidelines uses five criteria to decide on the likelihood of cervical spine injury following blunt trauma (see
Table 40.1). Though both criteria have been validated and demonstrate excellent interrater reliability, a comparison (
12) of the guidelines suggests that the Canadian C-spine rules may be more sensitive and specific for cervical spine injury in patients who are alert. Though there is evidence (
13) that clinical examination alone will miss some cervical spine injuries, the current guidelines for clearing of the cervical spine remain the same in a
patient who is awake, alert, and nonintoxicated and who does not have any distracting injuries (
14). If the cervical spine cannot be cleared based on the aforementioned criteria, further diagnostic imaging is warranted. Though plain x-ray was the standard radiographic evaluation, an overwhelming body of literature (
15) has demonstrated that plain x-rays have a sensitivity of 52% whereas CT scans of the cervical spine have a sensitivity of 98% in detecting traumatic changes. Thus, the current recommendation is that CT scanning of the cervical spine should be used to rule out C-spine injury over plain cervical x-rays in the acute setting although several centers continue to start with plain x-rays and use CT scan in a more selective manner.
Imaging of the obtunded or comatose patient remains a significant challenge. Given its excellent sensitivity in detecting injury, initial investigations for patients who are obtunded or comatose should begin with a CT scan of the cervical spine (
16). If there is evidence of injury, then an MRI is warranted to further assess the neural elements given the lack of a reliable neurologic physical evaluation. A more challenging scenario, however, is where the CT scan of the cervical spine does not identify any injury in the obtunded or comatose patient. In this scenario, there is tremendous controversy about the need for further imaging. The practice of obtaining flexion/extension views of the cervical spine in an obtunded patient is felt to add little information and is considered dangerous by some (
9,
17). The need for magnetic resonance imaging, however, has not been well established (
13). Some authors have demonstrated significant injuries based on MRI whereas others have not found MRI to be as useful (
13,
18,
19 and
20). Factors such as mechanism of injury, neurologic examination, and safety of obtaining an MRI in an obtunded patient all warrant consideration before this form of imaging is performed.
Though the guidelines for imaging of the cervical spine have been established, decision trees for imaging of the thoracic and lumbar spine are not as well prescribed. Currently, it is accepted by most that certain mechanisms of injury and clinical presentations increase the likelihood of thoracolumbar fractures (
21). High-velocity impact or collisions, falls from >10 feet, and generalized tonic-clonic seizures are all recognized as mechanistic risk factors for the development of thoracolumbar fractures. Clinical features such as intoxication, head injury, distracting injuries, neurologic deficit, and fractures elsewhere in the spine are recognized risk factors for having fractures of the thoracolumbar spine. Thus, all patients with the aforementioned mechanisms of injury or clinical presentation warrant further investigation with radiography. Asymptomatic patients do not require further investigation. The gold standard for imaging of the thoracolumbar spine has been plain x-ray radiography (
16). However, with the increasing use of CT scans for imaging of the chest and abdomen, reformatted CT images of the thoracolumbar spine have come into favor for evaluation of injury. There are currently no standardized guidelines for the use of CT scans in imaging of the thoracolumbar spine following blunt trauma though a recent consensus statement (
22) considers the need in the context of the need for imaging of other areas of injury. The indications (
16) for magnetic resonance imaging of the thoracolumbar spine include (a) the presence of neurologic deficits in the setting of identified spinal fractures, (b) abnormal CT scan findings, and (c) pain on clinical examination without x-ray evidence of ligamentous injury. Such an approach should allow for identification of injury to the cord and soft tissue structures following trauma.