8 Spinal Imaging
I. Key Points
– A complete history and physical should be the initial step in evaluating a patient to formulate a preliminary clinical diagnosis and to select the appropriate imaging modality.
– Findings on imaging exams must be clinically correlated to prevent a high false-positive rate.
– Multiple imaging modalities are available to supplement evaluation of spinal pathology, to confirm diagnosis, and to guide treatment.
II. Description
– Plain radiographs
• Convenient, universally available, and inexpensive
• Initial imaging modality for degenerative disorders, deformity, trauma, neoplasm, and infection (for spinal deformity, consider 36 in long-cassette standing x-rays)
• Limited ability to define subtle bony pathology and at least 30 to 40% bone loss needed for detection on plain radiographs
• Inability to directly visualize neural structures and allow bone and soft tissue discrimination
• Appropriately timed dynamic radiographs may help assess instability and the presence of spondylolisthesis.
 Important in evaluation of patients in the postoperative period to assess instrumentation and successful arthrodesis
Important in evaluation of patients in the postoperative period to assess instrumentation and successful arthrodesis
– Computed tomography (CT)
• Provides optimal visualization of bony detail and high sensitivity in detecting fractures, with accuracy rates ranging from 72 to 91% (Fig 8.1)
• Can help distinguish neural compression due to soft tissue versus bony pathology
• CT scan alone is limited in visualization of neural structures and demonstration of intrathecal and soft tissue pathology.
• For optimal bony detail, multiple thin cuts (1.5 to 3 mm) can be obtained with the gantry parallel to the plane of the disc.
• Multirow detector rapid thin-slice acquisitions allow contiguous 3 mm slices to be obtained from L1 to S1 in less than 30 seconds.
• Cognizance of radiation exposure to patients is essential.
– Myelography
• Intrathechal water-soluble contrast material mixes with cerebral spinal fluid and outlines the dural sac.
• Diagnosis is indirectly inferrable from changes in the contour of the contrast agent–filled thecal sac.
• Compression is demonstrated by extradural impression on the dye column and filling defects of the nerve root sleeve (Fig. 8.2).
• CT myelography improves visualization of foraminal and lateral recess stenosis with axial and reconstructed images.
• Advantageous in patients with stainless steel implants that cause significant metal artifact with MRI and patients with implantable devices (e.g., pacemaker) who cannot obtain MRI, and in evaluating fusion in postoperative patients with suspected nonunion
• Disadvantages of myelography include invasiveness and lack of diagnostic specificity.
– Magnetic resonance imaging (MRI)1
• The imaging modality of choice for the majority of spinal pathology

Fig. 8.1 Sagittal CT scan image demonstrates C5–6 perched fracture facet dislocation.
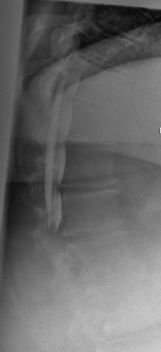
Fig. 8.2 Lateral plain radiograph after intrathecal contrast demonstrating complete block due to massive central herniated disc.
• Enhanced, noninvasive depiction of soft tissue pathology, including hematoma, infection, tumor, and ligamentous disruption, and identification of compression of neural elements (Fig 8.3)
• Utilizes pulsed radiofrequency (RF) and requires no radiation exposure
• T1-weighted images
 Short repetition time (TR), 400 to 600 ms; echo time (TE), 5 to 30 ms
Short repetition time (TR), 400 to 600 ms; echo time (TE), 5 to 30 ms
 MRI findings: cortical bone, low; free water, low; adipose, high
MRI findings: cortical bone, low; free water, low; adipose, high
• T2-weighted images
 TR = 1500 to 3000 ms, TE = 50 to 120 ms
TR = 1500 to 3000 ms, TE = 50 to 120 ms
 MRI findings: cortical bone, low; free water, high; adipose, low
MRI findings: cortical bone, low; free water, high; adipose, low
• Gadolinium contrast can help distinguish postoperative scar (vascular, enhances) from recurrent disc herniation (avascular, does not enhance) on T1-weighted sequence images.
• Contrast may also be helpful in detecting tumor and infection.2
 Infection: decreased signal on T1, increased signal on T2, enhancement with gadolinium, and often involves disc space
Infection: decreased signal on T1, increased signal on T2, enhancement with gadolinium, and often involves disc space
 Tumor: intervertebral disc often spared, similar homogeneous changes present involving entire vertebral body. With metatastic disease, may show multiple noncontiguous vertebral bodies involved, indicating skip lesions and involvement of the pedicle.
Tumor: intervertebral disc often spared, similar homogeneous changes present involving entire vertebral body. With metatastic disease, may show multiple noncontiguous vertebral bodies involved, indicating skip lesions and involvement of the pedicle.
• Spinal cord injury
 Quantifies degree of spinal cord compression and injury
Quantifies degree of spinal cord compression and injury

Fig. 8.3 Sagittal T2-weighted MRI image of the lumbar spine demonstrates large dorsal abscess causing severe compression of the neural elements at L4–5.
 High sensitivity in identifying ligamentous injury, including status of the posterior ligamentous complex, that may otherwise be missed on plain radiographs or CT
High sensitivity in identifying ligamentous injury, including status of the posterior ligamentous complex, that may otherwise be missed on plain radiographs or CT
 Helps distinguish spinal cord edema (T1 low, T2 high) from hemorrhage (T1 high, T2 high)
Helps distinguish spinal cord edema (T1 low, T2 high) from hemorrhage (T1 high, T2 high)
• Disc degeneration
 Advanced imaging should be reserved for patients with true radicular symptoms, with objective evidence of root irritation on examination, who have failed an appropriate course of conservative nonoperative management.
Advanced imaging should be reserved for patients with true radicular symptoms, with objective evidence of root irritation on examination, who have failed an appropriate course of conservative nonoperative management.
 High-intensity zone (HIZ): radial tear of the posterior annulus, fissure extending from nucleus to the periphery, unknown clinical significance
High-intensity zone (HIZ): radial tear of the posterior annulus, fissure extending from nucleus to the periphery, unknown clinical significance
 Herniated disc can be found in 21% of asymptomatic individuals between the ages of 20 and 39 years.
Herniated disc can be found in 21% of asymptomatic individuals between the ages of 20 and 39 years.
 Disc herniation nomenclature3:
Disc herniation nomenclature3:
 Protrusion: Herniation that maintains contact with the disc of origin with a bridge as wide as or wider than the diameter of the displaced material
Protrusion: Herniation that maintains contact with the disc of origin with a bridge as wide as or wider than the diameter of the displaced material
 Extruded: Diameter of the disc material beyond the interspace is greater than the width of the bridge that may or may not connect to the disc of origin.
Extruded: Diameter of the disc material beyond the interspace is greater than the width of the bridge that may or may not connect to the disc of origin.
 Sequestered: An extrusion that is no longer contiguous with the disc of origin
Sequestered: An extrusion that is no longer contiguous with the disc of origin
 Degenerative changes in the cervical and lumbar spine are age related and equally present in asymptomatic and symptomatic individuals.
Degenerative changes in the cervical and lumbar spine are age related and equally present in asymptomatic and symptomatic individuals.
 MRI findings must be strictly correlated with the clinical presentation.
MRI findings must be strictly correlated with the clinical presentation.
 Modic end plate changes2:
Modic end plate changes2:
 Type 1
Type 1
 T1 low, T2 high
T1 low, T2 high
 Associated with segmental spine instability and pain
Associated with segmental spine instability and pain
 Type 2
Type 2
 T1 high, T2 normal
T1 high, T2 normal
 More common than type 1, and may be less symptomatic
More common than type 1, and may be less symptomatic
 Type 3
Type 3
 T1 low, T2 low
T1 low, T2 low
 Indicative of advanced degeneration and sclerosis with less segmental instability
Indicative of advanced degeneration and sclerosis with less segmental instability
• Poor imaging will result from metal artifact from implants unless specific techniques are used (plastic < titanium < tantalum < stainless steel < cobalt chrome).
• Contraindications: pacemaker, inner ear implant, metal debris in the eye, ferrous metal implant in the brain
– Bone scintigraphy
• Standard part of workup for assessing metastatic bone disease (monostotic versus polyostotic). Helps point to area for more advanced imaging and evaluation.
• May be of value in distinguishing acute and chronic pars interarticularis fractures
III. Surgical Pearls
– Prior to obtaining any advanced imaging, a clear plan must be established for how the results will be utilized to facilitate the next line of treatment.
– A clinical diagnosis should be established based on a complete history and physical and correlated with findings on imaging prior to instituting a surgical or nonoperative treatment plan.
– Advanced imaging can be invaluable in confirming diagnosis and identifying treatment that has the best chance of clinical success.
Common Clinical Questions
1. A 57-year-old female presents with one week of intractable back pain, fever, chills, positive blood cultures, and elevated inflammatory markers. There is concern over discitis in the thoracolumbar region. MRI will likely show:
A. Increased T1 signal and decreased T2 signal with disc space involvement
B. Increased T1 signal, decreased T2 signal without disc space involvement
C. Increased T2 signal and decreased T1 signal with disc space involvement
D. Increased T2 signal and decreased T1 signal without disc space involvement
E. Increased T2 signal and increased T1 signal with disc space involvement
2. Which of the following statements regarding spinal imaging is true?
A. Adipose tissue causes a low-intensity signal on T1-weighted sequences and a high-intensity signal on T2-weighted images.
B. The presence of HIZ has been correlated with the presence of symptomatic back pain.
C. As the patient ages the sensitivity and specificity of imaging modalities such as CT and MRI improve.
D. Spinal cord edema can be distinguished from hemorrhage via a low-intensity signal on T1-weighted images and a high-intensity signal on T2-weighted images.
E. Benign Modic changes are characterized by a low-intensity signal on both T1- and T2-weighted images.
3. What is the best imaging modality for studying the bony anatomy preoperatively?
4. What is the appropriate initial radiographic study for spinal deformity?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






